J Korean Ophthalmol Soc.
2014 Oct;55(10):1535-1542. 10.3341/jkos.2014.55.10.1535.
The Effect of Simvastatin on the Expression of Catalase in Human Retinal Pigment Epithelial Cells
- Affiliations
-
- 1Department of Ophthalmology, Inha University School of Medicine, Incheon, Korea. hschin@inha.ac.kr
- KMID: 2216875
- DOI: http://doi.org/10.3341/jkos.2014.55.10.1535
Abstract
- PURPOSE
To evaluate the effects of simvastatin on the catalase expression in human retinal pigment epithelium.
METHODS
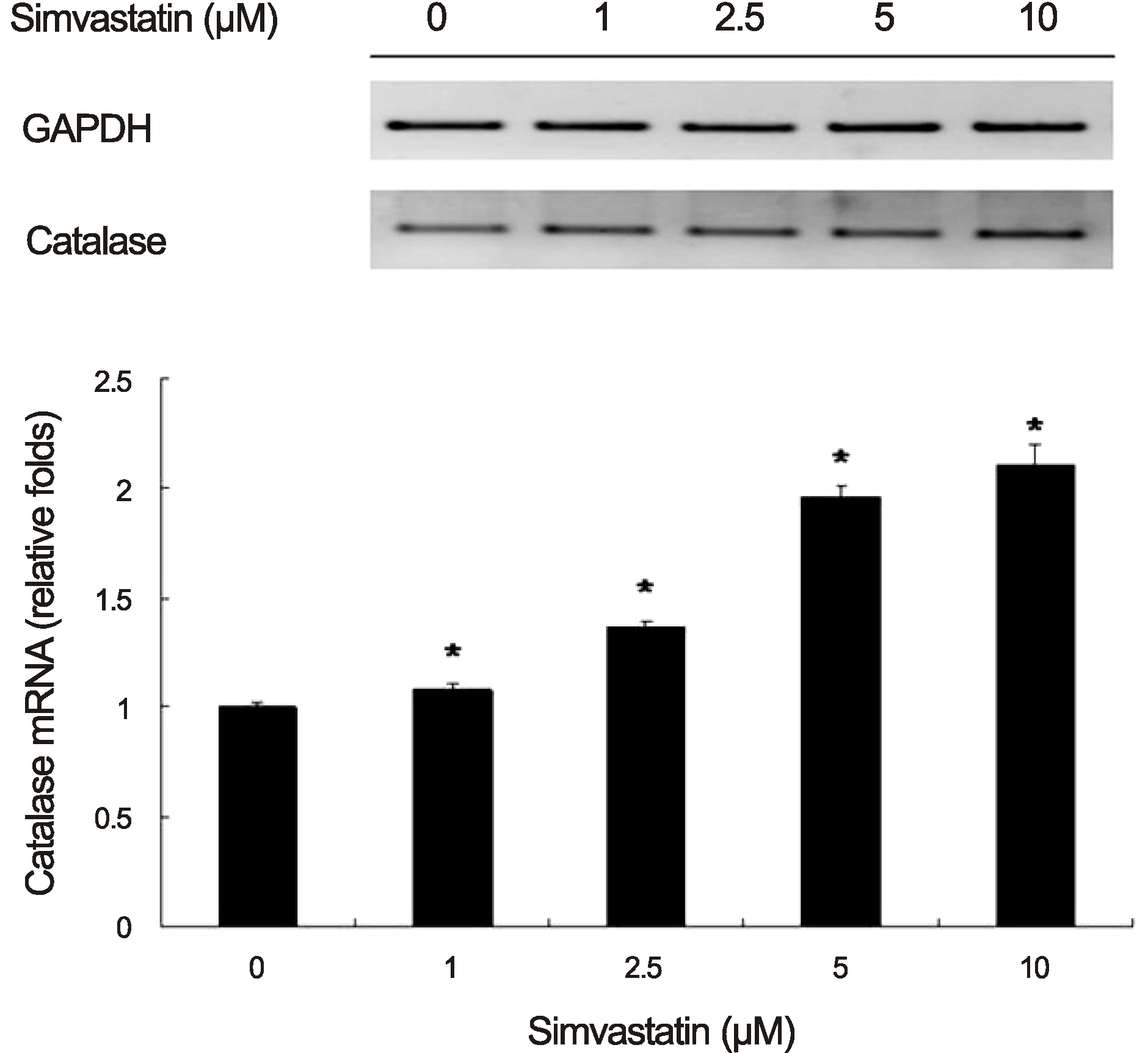
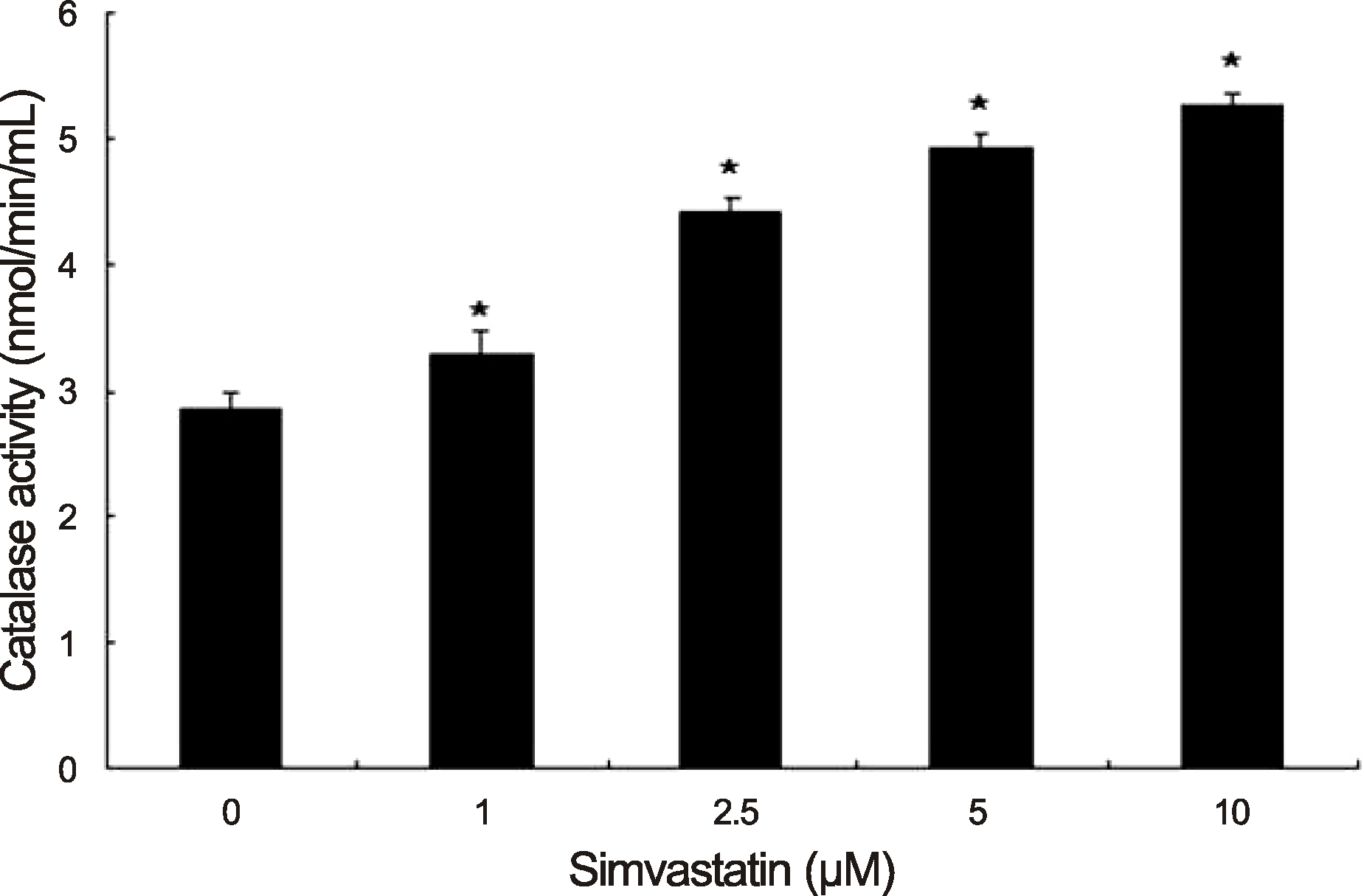
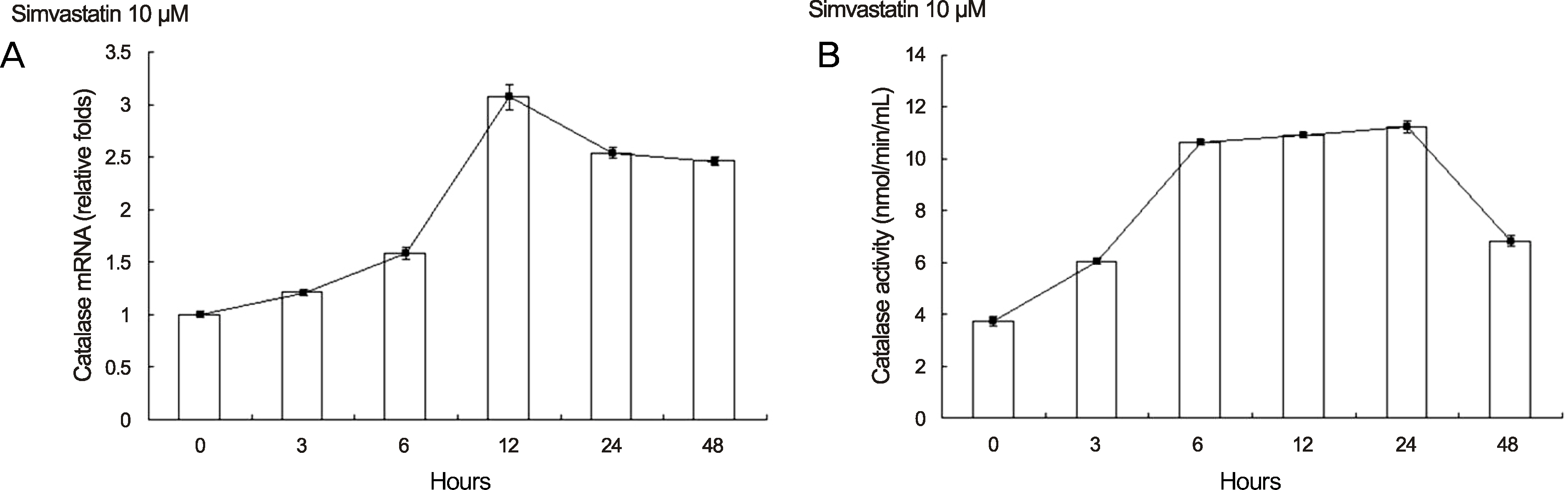
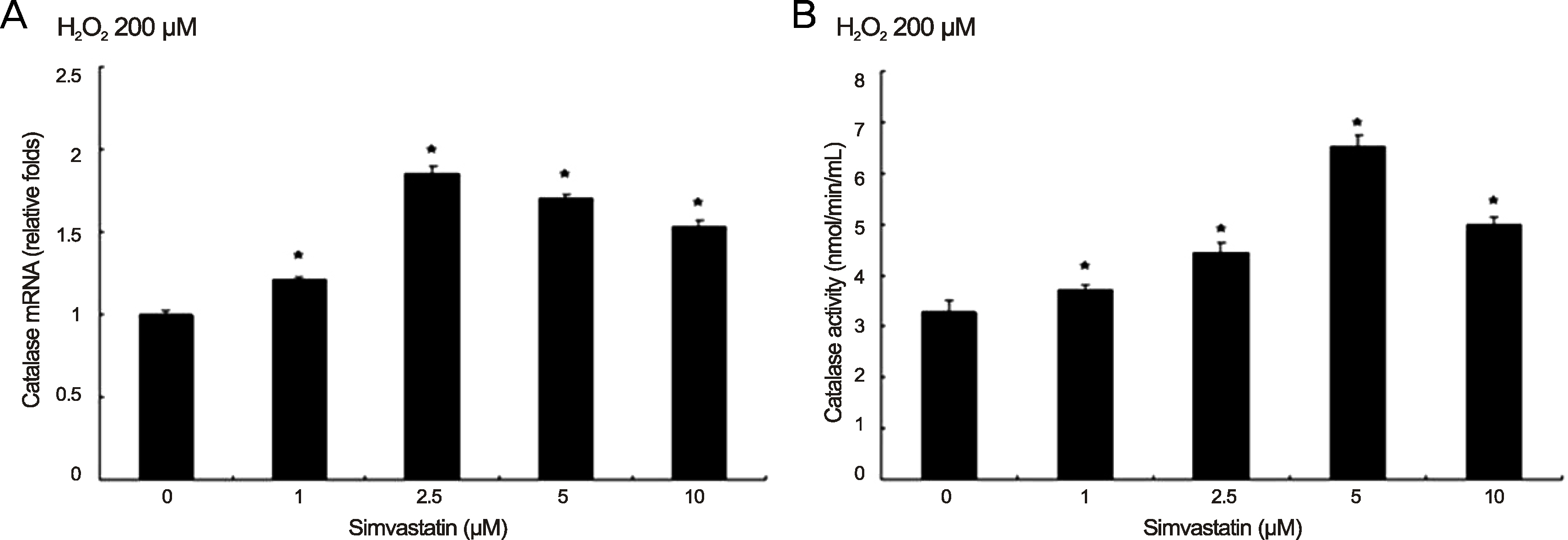
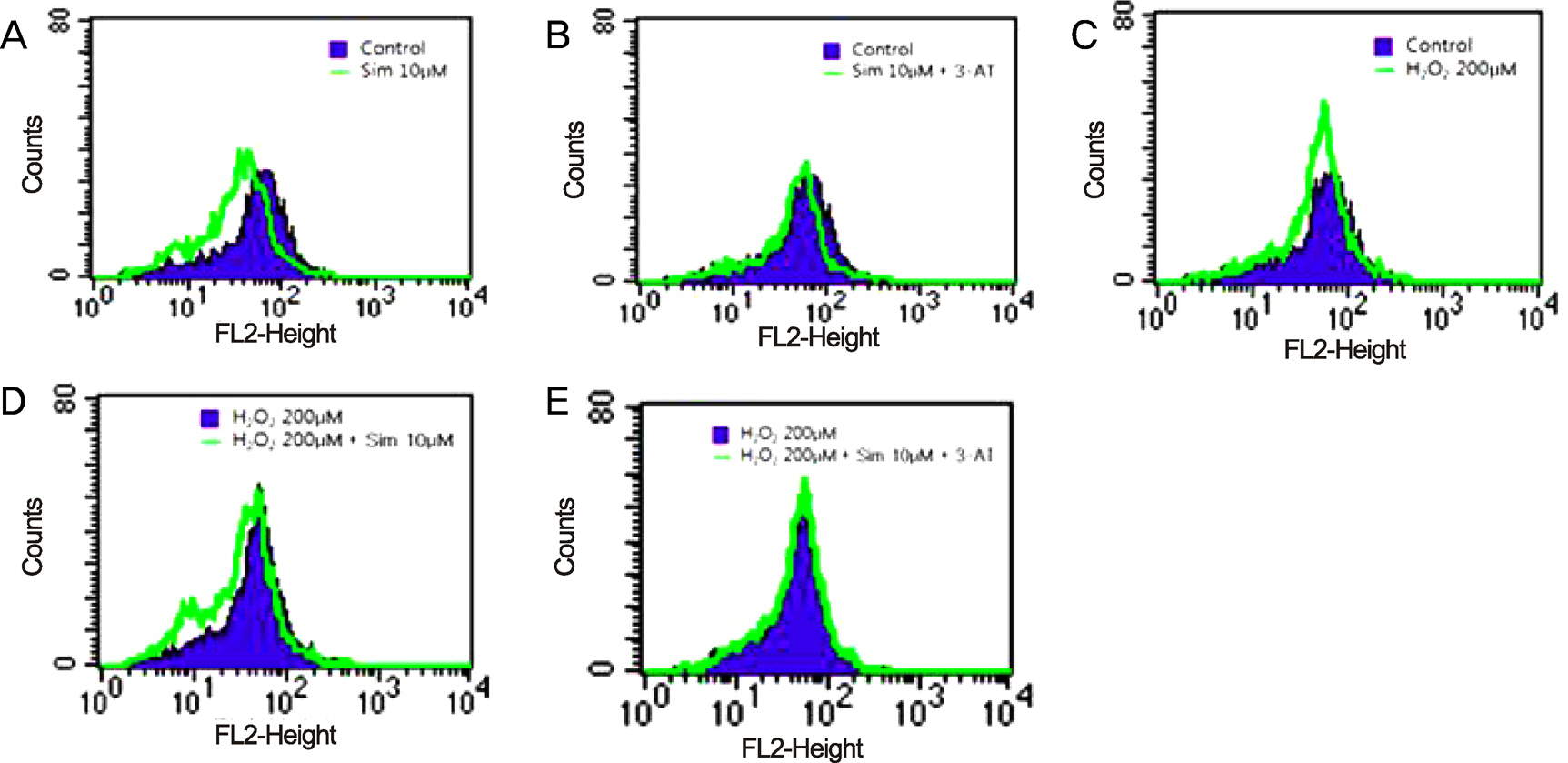
Retinal pigment epithelial (RPE) cells were incubated for 6 hours and 24 hours with various concentrations of simvastatin. In addition, RPE cells were incubated with 200 microM of H2O2 and various concentrations of simvastatin. After incubation, real-time polymerase chain reaction (PCR) was performed to examine the catalase messenger ribonucleic acid (mRNA) expression and a catalase assay was performed to examine the catalase activity in RPE. Intracellular reactive oxygen species (ROS) was measured using a fluorescence activated cell sorter (FACS).
RESULTS
Simvastatin increased the amount of catalase mRNA and catalase activity at 10 microM in RPE cells. Under oxidative stress (200 microM of H2O2), 2.5 microM of simvastatin increased the catalase mRNA expression and 5 microM of simvastatin increased catalase activity in RPE cells. In addition, simvastatin reduced free radical formation but this effect was diminished in the presence of an irreversible catalase inhibitor, 3-amino-1,2,4-triazole (3-AT).
CONCLUSIONS
Simvastatin exhibits anti-oxidative effects by inducing the catalase expression in human RPE cells. This anti-oxidative effect may be beneficial for preventing age-related macular degeneration induced by oxidative stress.
MeSH Terms
Figure
Reference
-
References
1. Friedman DS, O'Colmain BJ, Muñoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004; 122:564–72.
Article2. Bressler NM, Bressler SB, Congdon NG, et al. Potential public health impact of Age-Related Eye Disease Study results: AREDS report no. 11. Arch Ophthalmol. 2003; 121:1621–4.3. Klein R, Chou CF, Klein BE, et al. Prevalence of age-related macular degeneration in the US population. Arch Ophthalmol. 2011; 129:75–80.
Article4. Rein DB, Wittenborn JS, Zhang X, et al. Forecasting age-related macular degeneration through the year 2050: the potential impact of new treatments. Arch Ophthalmol. 2009; 127:533–40.5. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011; 25:421–33.
Article6. Folk JC, Stone EM. Ranibizumab therapy for neovascular age-related macular degeneration. N Engl J Med. 2010; 363:1648–55.
Article7. Young RW. Pathophysiology of age-related macular degeneration. Surv Ophthalmol. 1987; 31:291–306.
Article8. Winkler BS, Boulton ME, Gottsch JD, Sternberg P. Oxidative damage and age-related macular degeneration. Mol Vis. 1999; 5:32.9. Beatty S, Koh H, Phil M, et al. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000; 45:115–34.
Article10. Jäättelä M. Heat shock proteins as cellular lifeguards. Ann Med. 1999; 31:261–71.
Article11. Tate DJ Jr, Miceli MV, Newsome DA. Phagocytosis and H2O2 induce catalase and metallothionein gene expression in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 1995; 36:1271–9.12. Kim KJ, Kim KS, Kim NR, Chin HS. Effects of simvastatin on the expression of heme oxygenase-1 in human RPE cells. Invest Ophthalmol Vis Sci. 2012; 53:6456–64.
Article13. Haque R, Chun E, Howell JC, et al. MicroRNA-30b-mediated regulation of catalase expression in human ARPE-19 cells. PLoS One. 2012; 7:e42542.
Article14. Chelikani P, Fita I, Loewen PC. Diversity of structures and properties among catalases. Cell Mol Life Sci. 2004; 61:192–208.
Article15. Shepherd J. Statins: is there a need for alternative or adjunctive therapy? Br Heart J. 1995; 74:13.
Article16. Brown G, Albers JJ, Fisher LD, et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N Engl J Med. 1990; 323:1289–98.
Article17. Chuo JY, Wiens M, Etminan M, Maberley DA. Use of lipid-lowering agents for the prevention of age-related macular degeneration: a meta-analysis of observational studies. Ophthalmic Epidemiol. 2007; 14:367–74.
Article18. Pruefer D, Scalia R, Lefer AM. Simvastatin inhibits leukocyte-endothelial cell interactions and protects against inflammatory processes in normocholesterolemic rats. Arterioscler Thromb Vasc Biol. 1999; 19:2894–900.
Article19. Jialal I, Stein D, Balis D, et al. Effect of hydroxymethyl glutaryl coenzyme a reductase inhibitor therapy on high sensitive C-reactive protein levels. Circulation. 2001; 103:1933–5.
Article20. Wassmann S, Laufs U, Müller K, et al. Cellular antioxidant effects of atorvastatin in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2002; 22:300–5.
Article21. Yamada K, Sakurai E, Itaya M, et al. Inhibition of laser-induced choroidal neovascularization by atorvastatin by downregulation of monocyte chemotactic protein-1 synthesis in mice. Invest Ophthalmol Vis Sci. 2007; 48:1839–43.
Article22. Dobrucki LW, Kalinowski L, Dobrucki IT, Malinski T. Statin-stimulated nitric oxide release from endothelium. Med Sci Monit. 2001; 7:622–7.23. Qian J, Keyes KT, Long B, et al. Impact of HMG-CoA reductase inhibition on oxidant-induced injury in human retinal pigment epithelium cells. J Cell Biochem. 2011; 112:2480–9.
Article24. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001; 119:1417–36.25. Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013; 309:2005–15.26. Peponis V, Chalkiadakis SE, Bonovas S, Sitaras NM. The controversy over the association between statins use and progression of age-related macular degeneration: a mini review. Clin Ophthalmol. 2010; 4:865–9.27. Guymer RH, Dimitrov PN, Varsamidis M, et al. Can HMG Co-A reductase inhibitors (“statins”# slow the progression of age-related macular degeneration? The age-related maculopathy statin study #ARMSS#. Clin Interv Aging. 2008; 3:581–93.28. Friedman E, Rigas IK, Makar M. The relationship of statin use to the development of age-related macular degeneration. Invest Ophthalmol Vis Sci. 2005; 46:199.29. Delcourt C, Michel F, Colvez A, et al. Associations of cardiovascular disease and its risk factors with age-related macular degeneration: the POLA study. Ophthalmic Epidemiol. 2001; 8:237–49.
Article30. van Leeuwen R, Klaver CC, Vingerling JR, et al. Cholesterol and age-related macular degeneration: is there a link? Am J Ophthalmol. 2004; 137:750–2.
Article31. Drobek-Słowik M, Karczewicz D, Safranow K, et al. [Use of statins as a form of protection against age-related macular degeneration (AMD)]. Klin Oczna. 2008; 110:50–4.32. Fong DS, Contreras R. Recent statin use and 1-year incidence of exudative age-related macular degeneration. Am J Ophthalmol. 2010; 149:955–8.e1.
Article33. Anderson DH, Mullins RF, Hageman GS, Johnson LV. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol. 2002; 134:411–31.
Article34. Johnson LV, Leitner WP, Staples MK, Anderson DH. Complement activation and inflammatory processes in Drusen formation and age related macular degeneration. Exp Eye Res. 2001; 73:887–96.
Article35. Mullins RF, Russell SR, Anderson DH, Hageman GS. Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. FASEB J. 2000; 14:835–46.
Article36. Albert MA, Danielson E, Rifai N, Ridker PM. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation /CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001; 286:64–70.37. Lopez PF, Sippy BD, Lambert HM, et al. Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Invest Ophthalmol Vis Sci. 1996; 37:855–68.
Article38. Simons M. Molecular multitasking: statins lead to more arteries, less plaque. Nat Med. 2000; 6:965–6.
Article39. Dichtl W, Dulak J, Frick M, et al. HMG-CoA reductase inhibitors regulate inflammatory transcription factors in human endothelial and vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2003; 23:58–63.
Article40. Frank RN, Amin RH, Puklin JE. Antioxidant enzymes in the macular retinal pigment epithelium of eyes with neovascular age-related macular degeneration. Am J Ophthalmol. 1999; 127:694–709.41. Olsen RH, Johnson LA, Zuloaga DG, et al. Enhanced hippocampus-dependent memory and reduced anxiety in mice over-expressing human catalase in mitochondria. J Neurochem. 2013; Feb 5. [Epub ahead of print].
Article42. Gáspár T, Domoki F, Lenti L, et al. Neuroprotective effect of adenoviral catalase gene transfer in cortical neuronal cultures. Brain Res. 2009; 1270:1–9.
Article43. Milton NG. Inhibition of catalase activity with 3-amino-triazole enhances the cytotoxicity of the Alzheimer's amyloid-beta peptide. Neurotoxicology. 2001; 22:767–74.44. Piechota-Polanczyk A, Goraca A, Demyanets S, et al. Simvastatin decreases free radicals formation in the human abdominal aortic aneurysm wall via NF-κB. Eur J Vasc Endovasc Surg. 2012; 44:133–7.
Article45. Wassmann S, Laufs U, Müller K, et al. Cellular antioxidant effects of atorvastatin in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2002; 22:300–5.
Article46. Broncel M, Koter-Michalak M, Chojnowska-Jezierska J. [The effect of statins on lipids peroxidation and activities of antioxidants enzymes in patients with dyslipidemia]. Przegl Lek. 2006; 63:738–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Simvastatin on the Expression of VEGF in Human Retinal Pigment Epithelial Cells
- The Effect of 5-Fluorouraci1 on the Activity of the Retinal Pigment Epithelium in Vitro
- The Effects of High Glucose on Paraquat-induced Cell Injury in Human Retinal Pigment Epithelial Cells
- Growth Patterns of Human Retinal Pigment Epithelium in Vitro
- Comparison of Inhibitory Effects of 5-Fluorouracil and Mitomycin C on Proliferation of Fibroblagts and Retinal Pigment Epithelial Cells