Nutr Res Pract.
2011 Apr;5(2):150-156.
Relationship between inflammation biomarkers, antioxidant vitamins, and bone mineral density in patients with metabolic syndrome
- Affiliations
-
- 1Major in Food and Nutrition, Wonkwang University, Sinyong-dong, Iksan, Jeonbuk 570-749, Korea. ccha@wku.ac.kr
- 2Department of Food Science and Nutrition, Daejin University, Pocheon 487-711, Korea.
- 3Health Promotion Center, Seoul National University of Bundang Hospital, Seongnam 463-707, Korea.
Abstract
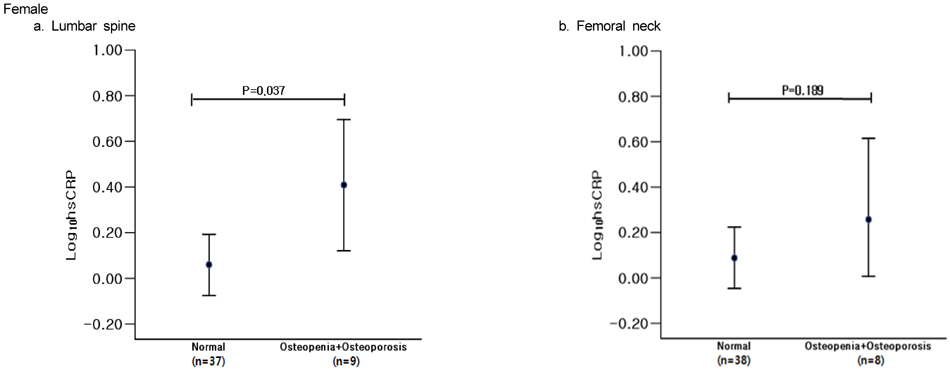
- Few studies have shown the correlation between metabolic syndrome and bone mineral density (BMD). The main pathogenic mechanisms of metabolic syndrome rely on chronic low-level inflammatory status and oxidative stress. There are few studies that examine the gender-specific effects of inflammation and antioxidants on BMD. In this study, we evaluated the relative contribution of these factors in patients with metabolic syndrome. We conducted a cross-sectional study of 67 men and 46 postmenopausal women with metabolic syndrome; metabolic syndrome was defined as having three or more metabolic syndrome risk factors. BMD, body fat mass, and lean body mass were evaluated. We also examined the levels of high sensitive C-reactive protein (hs-CRP), interleukin-6 (IL-6), adiponectin, vitamin E, and C in serum. Log-transformed hs-CRP levels were significantly higher in lumbar spine osteoporotic subjects than in normal subjects for women but not for men. There was no significant difference between the normal group and the osteoporotic group in other inflammatory markers. Stepwise regression analyses for BMD of the lumbar spine showed that lean body mass and vitamin E were significant determinants in men. Lean body mass and log-transformed hs-CRP were significant determinants in women Analysis for BMD of the femoral neck showed that lean body mass was a significant determinant for both men and women. There was no significant factor among the inflammatory markers or antioxidant vitamins affecting the femoral neck BMD for either gender. In conclusion, while hs-CRP is an independent predictor of the BMD of the lumbar spine in women, vitamin E showed profound effects on BMD in men but not women with metabolic syndrome.
Keyword
MeSH Terms
Figure
Reference
-
1. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001. 24:683–689.
Article2. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002. 288:2709–2716.
Article3. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.4. Ministry of Health and Welfare (MOHW). Korea National Health and Nutrition Examination Survey Report (KNHANES III)-Health Examination. 2005.5. Kim JH, Choi SR, Lee JR, Shin JH, Lee SJ, Han MA, Park J, Bae HY, Kim SY. Association of hemoglobin A1c with cardiovascular disease risk factors and metabolic syndrome in nondiabetic adults. Korean Diabetes J. 2008. 32:435–444.
Article6. Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005. 115:1111–1119.
Article7. Luc G, Bard JM, Juhan-Vague I, Ferrieres J, Evans A, Amouyel P, Arveiler D, Fruchart JC, Ducimetiere P. C-reactive protein, interleukin-6, and fibrinogen as predictors of coronary heart disease: the PRIME study. Arterioscler Thromb Vasc Biol. 2003. 23:1255–1261.
Article8. Furukawa S, Fujita T, shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004. 114:1752–1761.
Article9. Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations. Diabetes. 2003. 52:2346–2352.
Article10. Palmieri VO, Grattagliano I, Portincasa P, Palasciano G. Systemic oxidative alterations are associated with visceral adiposity and liver steatosis in patients with metabolic syndrome. J Nutr. 2006. 136:3022–3326.
Article11. Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen Q, Chihara K. Plasma lipids and osteoporosis in postmenopausal women. Endocr J. 2002. 49:211–217.
Article12. Cui LH, Shin MH, Chung EK, Lee YH, Kweon SS, Park KS, Choi JS. Association between bone mineral densities and serum lipid profiles of pre- and post-menopausal rural women in South Korea. Osteoporos Int. 2005. 16:1975–1981.
Article13. von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E. Associations between the metabolic syndrome and bone health in older men and women: the Rancho Bernardo Study. Osteoporos Int. 2007. 18:1337–1344.
Article14. Kang YH, Kam S. Association of bone mineral density with the metabolic syndrome. J Radiol Sci Technol. 2008. 31:259–266.15. Kim HY, Choe JW, Kim HK, Bae SJ, Kim BJ, Lee SH, Koh JM, Han KO, Park HM, Kim GS. Negative association between metabolic syndrome and bone mineral density in Koreans, especially in men. Calcif Tissue Int. 2010. 86:350–358.
Article16. Oh KW. Diabetes and osteoporosis. Korean J Bone Metab. 2008. 15:91–98.
Article17. Lazarenko OP, Rzonca SO, Hogue WR, Swain FL, Suva LJ, Lecka-Czernik B. Rosiglitazone induces decreases in bone mass and strength that are reminiscent of aged bone. Endocrinology. 2007. 148:2669–2680.
Article18. Sorocéanu MA, Miao D, Bai XY, Su H, Goltzman D, Karaplis AC. Rosiglitazone impacts negatively on bone by promoting osteoblast/osteocyte apoptosis. J Endocrinol. 2004. 183:203–216.
Article19. Lara-Castro C, Fu Y, Chung BH, Garvey WT. Adiponectin and the metabolic syndrome: mechanisms mediating risk for metabolic and cardiovascular disease. Curr Opin Lipidol. 2007. 18:263–270.
Article20. Yamaguchi N, Kukita T, Li YJ, Kamio N, Fukumoto S, Nonaka K, Ninomiya Y, Hanazawa S, Yamashita Y. Adiponectin inhibits induction of TNF-alpha/RANKL-stimulated NFATc1 via the AMPK signaling. FEBS Lett. 2008. 582:451–456.
Article21. Feingold KR, Grunfeld C. Role of cytokines in inducing hyperlipidemia. Diabetes. 1992. 41:97–101.
Article22. Hotamisligil GS, Murray DL, Choy LN, Spiegelman BM. Tumor necrosis factor alpha inhibits signaling from the insulin receptor. Proc Natl Acad Sci U S A. 1994. 91:4854–4858.
Article23. Ridker PM. High-sensitivity C-reactive protein: potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001. 103:1813–1818.
Article24. Whitcomb BW, Bruder JM, Bauer RL, Mahaney MC, Tracy RP, Kammerer CM, Mitchell BD. C-reactive protein levels are associated with decreased bone mineral density in Mexican Americans. J Bone Miner Res. 2004. 19:S289.25. Bae SJ, Son HY, Pyun DK, Nah SS, Koh JM, Kim GS. Higher circulating hs-CRP levels are associated with lower bone mineral density in healthy premenopausal and postmenopausal women: evidence for link between systemic inflammation and osteoporosis. Korean J Bone Metab. 2004. 11:147–157.26. Kim BJ, Kim WG, Jung CH, Byun SW, Koh JM, Kim GS. Relationship between bone turnover rate and a systemic inflammatory marker in Korean women. Korean J Bone Metab. 2006. 13:129–138.27. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. Harmonizing the Metabolic Syndrome A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009. 120:1640–1645.28. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO technical report series. 1994. Geneva: WHO.29. Bieri JG, Tolliver TJ, Catignani GL. Simultaneous determination of α-tocopherol and retinol in plasma or red cells by high pressure liquid chromatography. Am J Clin Nutr. 1979. 32:2143–2149.
Article30. Kutnink MA, Hawkes WC, Schaus EE, Omaye ST. An internal standard method for the unattended high-performance liquid chromatographic analysis of ascorbic acid in blood components. Anal Biochem. 1987. 166:424–430.
Article31. Nishida M, Moriyama T, Ishii K, Takashima S, Yoshizaki K, Sugita Y, Yamauchi-Takihara K. Effects of IL-6, adiponectin, CRP and metabolic syndrome on subclinical atherosclerosis. Clin Chim Acta. 2007. 384:99–104.
Article32. Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS. Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int. 2005. 16:1263–1271.
Article33. Kinjo M, Setoguchi S, Solomon DH. Bone Mineral Density in adults with the Metabolic Syndrome: analysis in a population-based U.S. Sample. J Clin Endocrinol Metab. 2007. 92:4161–4164.
Article34. McLean RR, Zhang X, Benjamin EJ, Cupples LA, Kiel DP, Hannan MT. No link between C-Reactive Protein (CRP) and Bone Mineral Density (BMD) in men, but menopause status modifies the relation in women: The Framingham Osteoporosis Study. Arthritis Rheum. 2009. 60:Suppl 10. 1131.35. Scheidt-Nave C, Bismar H, Leidig-Bruckner G, Woitge H, Seibel MJ, Ziegler R, Pfeilschifter J. Serum interleukin 6 is a major predictor of bone loss in women specific to the first decade past menopause. J Clin Endocrinol Metab. 2001. 86:2032–2042.
Article36. Richards JB, Valdes AM, Burling K, Perks UC, Spector TD. Serum adiponectin and bone mineral density in women. J Clin Endocrinol Metab. 2007. 92:1517–1523.
Article37. Zoico E, Zamboni M, Di Francesco V, Mazzali G, Fantin F, De Pergola G, Zivelonghi A, Adami S, Bosello O. Relation between adiponectin and bone mineral density in elderly post-menopausal women: role of body composition, leptin, insulin resistance, and dehydroepiandrosterone sulfate. J Endocrinol Invest. 2008. 31:297–302.
Article38. Russell M, Mendes N, Miller KK, Rosen CJ, Lee H, Klibanski A, Misra M. Visceral fat is a negative predictor of bone density measures in obese adolescent girls. J Clin Endocrinol Metab. 2010. 95:1247–1255.
Article39. Kim CJ, Rhee EJ, Kim HM, Kim HS, Lee EA, Kim YS, Choi JH, Jo SK, Jung CH, Won JC, Park CY, Lee WY, Oh KW, Park SW, Kim SW. Relationship between body composition and metabolic bone disease in Korean male adults. Korean J Bone Metab. 2008. 15:25–32.40. Miller ER 3rd, Pastor-Barriuso R, Dalal D, Riemersma RA, Appel LJ, Guallar E. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. 2005. 142:37–46.
Article41. Lim Y, Traber MG. Alpha-tocopherol transfer protein: insights from alpha-tocopherol transfer protein knockout mice. Nutr Res Pract. 2007. 1:247–253.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of the Metabolic Syndrome and Bone Mineral Density in Postmenopausal Women
- The relationship of maturation value of vaginal epithelium and bone mineral density in postmenopausal women
- Effect of Calcium and Activated Vitamin D ( 1- hydroxyvitamin-D ) on Bone Mineral Density in Osteoporosis
- Relationship between Metabolic Syndrome and Bone Mineral Density in Middle-aged Women
- The Relationship between Lifetime Sports Activity Measured with MET and Peak Strain Score and Bone Measurement in College-aged Women