J Lipid Atheroscler.
2019 Sep;8(2):173-182. 10.12997/jla.2019.8.2.173.
The Potential Role of Biomarkers Associated with ASCVD Risk: Risk-Enhancing Biomarkers
- Affiliations
-
- 1Division of Cardiology, Kangnam Sacred Heart Hospital, Hallym University, College of Medicine, Seoul, Korea. heartcsh@gmail.com
- KMID: 2458382
- DOI: http://doi.org/10.12997/jla.2019.8.2.173
Abstract
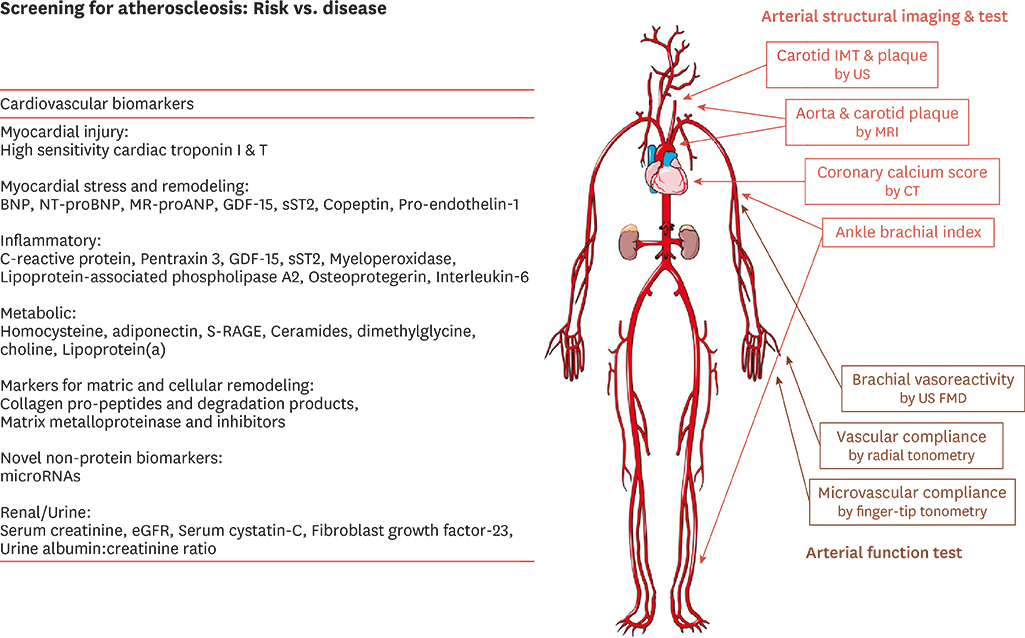
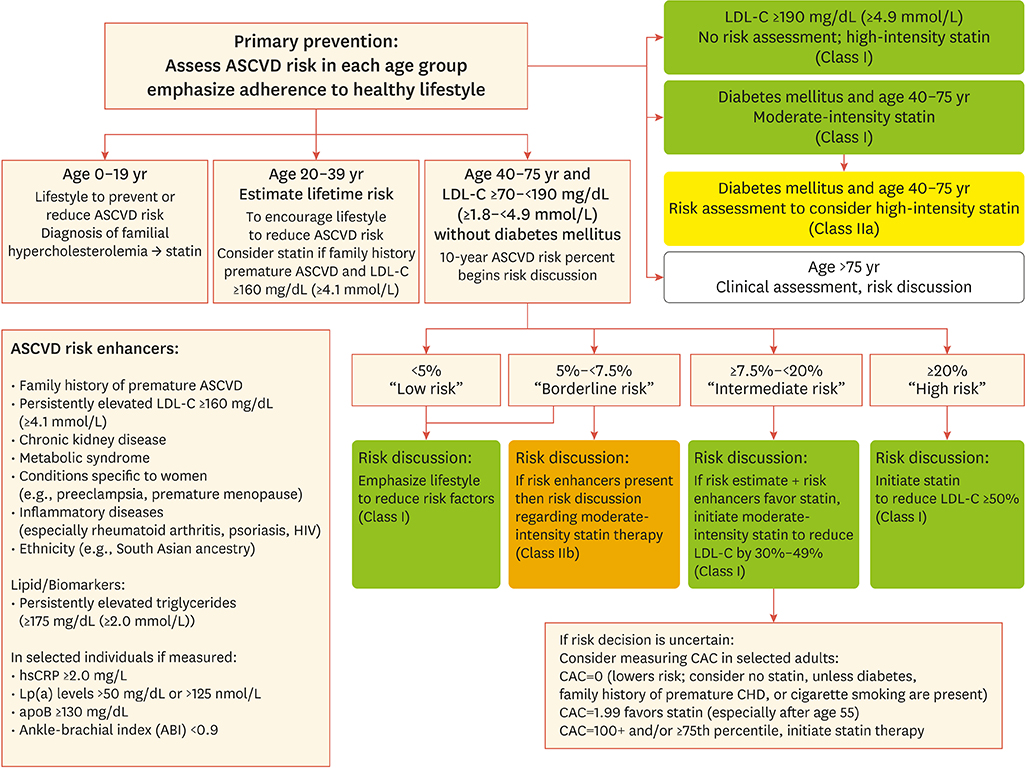
- Serum cholesterol is major risk factor and contributor to atherosclerotic cardiovascular disease (ASCVD). Therapeutic cholesterol-lowering drugs, especially statin, revealed that reduction in low-density lipoprotein cholesterol (LDL-C) produces marked reduction of ASCVD events. In the preventive scope, lower LDL-C is generally accepted as better in proven ASCVD patients and high-risk patient groups. However, in patients with low to intermediate risk without ASCVD, risk assessment is clinically guided by traditional major risk factors. In this group, the complement approach to detailed risk assessment about traditional major risk factors is needed. These non-traditional risk factors include ankle-brachial index (ABI), high-sensitivity C-reactive protein (hsCRP) level, lipoprotein(a) (Lp[a]), apolipoprotein B (apoB), or coronary artery calcium (CAC) score. CAC measurements have an additive role in the decision to use statin therapy in non-diabetic patients 40-75 years old with intermediate risk in primary prevention. This review comprises ASCVD lipid/biomarkers other than CAC. The 2013 and 2018 American College of Cardiology/American Heart Association (ACC/AHA) guidelines suggest these factors as risk-enhancing factors to help health care providers better determine individualized risk and treatment options especially regarding abnormal biomarkers. The recent 2018 Korean guidelines for management of dyslipidemia did not include these biomarkers in clinical decision making. The current review describes the current roles of hsCRP, ABI, LP(a), and apoB in personal modulation and management of health based on the 2018 ACC/AHA guideline on the management of blood cholesterol.
Keyword
MeSH Terms
-
Ankle Brachial Index
Apolipoproteins
Apolipoproteins B
Biomarkers*
C-Reactive Protein
Calcium
Cardiovascular Diseases
Cholesterol
Clinical Decision-Making
Complement System Proteins
Coronary Vessels
Dyslipidemias
Health Personnel
Heart
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors
Lipoprotein(a)
Lipoproteins
Primary Prevention
Risk Assessment
Risk Factors
Apolipoproteins
Apolipoproteins B
Biomarkers
C-Reactive Protein
Calcium
Cholesterol
Complement System Proteins
Lipoprotein(a)
Lipoproteins
Figure
Cited by 1 articles
-
Associations of Dietary Intake with Cardiovascular Disease, Blood Pressure, and Lipid Profile in the Korean Population: a Systematic Review and Meta-Analysis
Jeongseon Kim, Tung Hoang, So Young Bu, Ji-Myung Kim, Jeong-Hwa Choi, Eunju Park, Seung-Min Lee, Eunmi Park, Ji Yeon Min, In Seok Lee, So Young Youn
J Lipid Atheroscler. 2020;9(1):205-229. doi: 10.12997/jla.2020.9.1.205.
Reference
-
1. Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986; 256:2823–2828.
Article2. Kannel WB, Castelli WP, Gordon T, McNamara PM. Serum cholesterol, lipoproteins, and the risk of coronary heart disease. The Framingham study. Ann Intern Med. 1971; 74:1–12.
Article3. Boekholdt SM, Hovingh GK, Mora S, Arsenault BJ, Amarenco P, Pedersen TR, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol. 2014; 64:485–494.
Article4. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015; 372:2387–2397.
Article5. Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017; 376:1713–1722.
Article6. Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016; 316:1289–1297.
Article7. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2889–2934.
Article8. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; 139:e1046–e1081.9. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J. 2016; 37:2999–3058.
Article10. Committee of Clinical Practice Guideline of the Korean Society of Lipid and Atherosclerosis (KSoLA). 2018 Korean Guidelines for the Management of Dyslipidemia. 4th ed. Seoul: Korean Society of Lipid and Atherosclerosis;2018.11. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:S1–S45.12. Muntner P, Colantonio LD, Cushman M, Goff DC Jr, Howard G, Howard VJ, et al. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA. 2014; 311:1406–1415.
Article13. Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963; 107:539–556.
Article14. Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991; 1:263–276.
Article15. Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979; 110:281–290.16. Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988; 41:1105–1116.
Article17. The ARIC investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989; 129:687–702.18. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837–1847.
Article19. Mora S, Wenger NK, Cook NR, Liu J, Howard BV, Limacher MC, et al. Evaluation of the Pooled Cohort risk equations for cardiovascular risk prediction in a multiethnic cohort from the Women's Health Initiative. JAMA Intern Med. 2018; 178:1231–1240.
Article20. Asia Pacific Cohort Studies Collaboration. Barzi F, Patel A, Gu D, Sritara P, Lam TH, et al. Cardiovascular risk prediction tools for populations in Asia. J Epidemiol Community Health. 2007; 61:115–121.
Article21. Jee SH, Park JW, Lee SY, Nam BH, Ryu HG, Kim SY, et al. Stroke risk prediction model: a risk profile from the Korean study. Atherosclerosis. 2008; 197:318–325.
Article22. Jee SH, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014; 4:e005025.
Article23. Park GM, Han S, Kim SH, Jo MW, Her SH, Lee JB, et al. Model for assessing cardiovascular risk in a Korean population. Circ Cardiovasc Qual Outcomes. 2014; 7:944–951.
Article24. Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Ann Intern Med. 2009; 151:483–495.
Article25. Cushman M, Arnold AM, Psaty BM, Manolio TA, Kuller LH, Burke GL, et al. C-reactive protein and the 10-year incidence of coronary heart disease in older men and women: the cardiovascular health study. Circulation. 2005; 112:25–31.
Article26. Koenig W, Löwel H, Baumert J, Meisinger C. C-reactive protein modulates risk prediction based on the Framingham Score: implications for future risk assessment: results from a large cohort study in southern Germany. Circulation. 2004; 109:1349–1353.
Article27. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008; 359:2195–2207.
Article28. Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Circulation. 1993; 88:837–845.
Article29. Weatherley BD, Nelson JJ, Heiss G, Chambless LE, Sharrett AR, Nieto FJ, et al. The association of the ankle-brachial index with incident coronary heart disease: the Atherosclerosis Risk In Communities (ARIC) study, 1987–2001. BMC Cardiovasc Disord. 2007; 7:3.
Article30. Newman AB, Shemanski L, Manolio TA, Cushman M, Mittelmark M, Polak JF, et al. Ankle-arm index as a predictor of cardiovascular disease and mortality in the Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 1999; 19:538–545.
Article31. Abbott RD, Petrovitch H, Rodriguez BL, Yano K, Schatz IJ, Popper JS, et al. Ankle/brachial blood pressure in men >70 years of age and the risk of coronary heart disease. Am J Cardiol. 2000; 86:280–284.
Article32. Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation. 2004; 109:733–739.
Article33. Moyer VA. U.S. Preventive Services Task Force. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013; 159:342–348.
Article34. Ogren M, Hedblad B, Engström G, Janzon L. Prevalence and prognostic significance of asymptomatic peripheral arterial disease in 68-year-old men with diabetes. Results from the population study ‘Men born in 1914’ from Malmö, Sweden. Eur J Vasc Endovasc Surg. 2005; 29:182–189.
Article35. Pang XH, Han J, Ye WL, Sun X, Ding Y, Huang WJ, et al. Lower extremity peripheral arterial disease is an independent predictor of coronary heart disease and stroke risks in patients with type 2 diabetes mellitus in China. Int J Endocrinol. 2017; 2017:9620513.
Article36. Emerging Risk Factors Collaboration. Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009; 302:1993–2000.
Article37. Sniderman AD, Williams K, Contois JH, Monroe HM, McQueen MJ, de Graaf J, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes. 2011; 4:337–345.
Article38. Sniderman AD, Tremblay A, De Graaf J, Couture P. Phenotypes of hypertriglyceridemia caused by excess very-low-density lipoprotein. J Clin Lipidol. 2012; 6:427–433.
Article39. Grundy SM, Vega GL, Tomassini JE, Tershakovec AM. Comparisons of apolipoprotein B levels estimated by immunoassay, nuclear magnetic resonance, vertical auto profile, and non-high-density lipoprotein cholesterol in subjects with hypertriglyceridemia (SAFARI Trial). Am J Cardiol. 2011; 108:40–46.
Article40. Writing Committee. Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD Jr, et al. 2016 ACC expert consensus decision pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2016; 68:92–125.
Article41. Bostom AG, Cupples LA, Jenner JL, Ordovas JM, Seman LJ, Wilson PW, et al. Elevated plasma lipoprotein(a) and coronary heart disease in men aged 55 years and younger. A prospective study. JAMA. 1996; 276:544–548.
Article42. Bostom AG, Gagnon DR, Cupples LA, Wilson PW, Jenner JL, Ordovas JM, et al. A prospective investigation of elevated lipoprotein (a) detected by electrophoresis and cardiovascular disease in women. The Framingham Heart Study. Circulation. 1994; 90:1688–1695.
Article43. Tsimikas S. A test in context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol. 2017; 69:692–711.44. Cook NR, Mora S, Ridker PM. Lipoprotein(a) and cardiovascular risk prediction among women. J Am Coll Cardiol. 2018; 72:287–296.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Potential Biomarkers to Improve the Prediction of Osteoporotic Fractures
- Role of Tumor Biomarkers in the Surveillance of Hepatocellular Carcinoma
- Clinical Utility of Novel Biomarkers in the Prediction of Coronary Heart Disease
- Emerging Circulating Biomarkers for Enhanced Cardiovascular Risk Prediction
- Biomarkers for Stroke