Korean Circ J.
2008 Mar;38(3):161-169. 10.4070/kcj.2008.38.3.161.
Predictive Factors of Major Adverse Cardiac Events and Clinical Outcomes of Acute Myocardial Infarction in Young Korean Patients
- Affiliations
-
- 1Korea Acute Myocardial Infarction Registry of the Korean Society of Cardiology, Gwangju, Korea. myungho@chollian.net
- KMID: 2225833
- DOI: http://doi.org/10.4070/kcj.2008.38.3.161
Abstract
- BACKGROUND AND OBJECTIVES
Acute myocardial infarction (AMI) occurring in patients at a young age (40 years or younger) is an uncommon condition and is characterized by multiple cardiovascular risk factors. We analyzed the risk factors of young-aged Korean AMI patients (age of 40 years or younger) and other AMI patients, who were registered in the Korea Acute Myocardial Infarction Registry (KAMIR) for one year.
SUBJECTS AND METHODS
In 2006, 8,565 patients (mean age 64.4+/-12.7 years; 5,591 males) were registered in the KAMIR. The patients were divided into two groups: Group I (younger patients < or =40 years; n=261; mean age 35.9+/-4.5 years; 245 males) and Group II (older patients >40 years; n=8,304, mean age 65.4+/-11.8 years; 5,330 males). The clinical and angiographic characteristics and major adverse cardiac events (MACE) were compared for the two groups of patients.
RESULTS
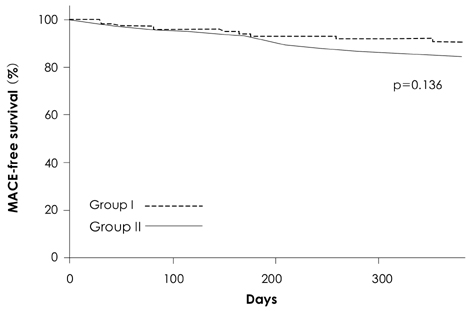
The baseline clinical characteristics of gender, age, risk factors (hypertension, smoking, diabetes, familial history) and body weight were different between the two groups (p<0.001). The baseline echocardiographic and laboratory findings of the initial ejection fraction, and the glomerular filtration rate, level of creatine kinase (CK), level of CK-MB isoenzyme, total cholesterol level, triglyceride level, and N-terminal prohormone brain natriuretic peptide (NT-proBNP) level were different between the two groups (p< or =0.001). According to the use of multiple logistic regression analysis, use of thrombolysis [p=0.009, adjusted hazard ratio (aHR)=9.140, 95% confidence interval (CI): 1.727-48.383], a high blood glucose level (p=0.029, aHR=1.008, 95% CI: 1.001-1.016), a low body mass index (<25 kg/m(2), p=0.031, aHR=6.236, 95% CI: 1.183-32.857), and a high CK-MB level and high Thrombolysis in Myocardial Infarction (TIMI) risk score were independent predictors of MACE at 1 year after an AMI in young age patients. Early clinical outcomes were better in Group I than in Group II patients, but one-, six- and twelve-month MACE were not different between the two groups.
CONCLUSION
The independent predictors of MACE at 1 year in young age AMI patients were the use of thrombolysis, a high blood glucose level, a low body mass index, a high CK-MB level and a high TIMI risk score. Patients that have had an acute myocardial infarction at a young age have a better early clinical outcome, but the long-term clinical outcomes were not different compared with older patients, and thus long-term intensive medical therapy will be required, even in young AMI patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Knowledge on Cardiovascular Prevention and Nicotine Dependency among Smoking Male College Students
Seon Young Hwang, Kyongok Park
J Korean Acad Community Health Nurs. 2014;25(2):75-84. doi: 10.12799/jkachn.2014.25.2.75.
Reference
-
1. Shiraishi J, Kohno Y, Yamaguchi S, et al. Acute myocardial infarction in young Japanese adults. Circ J. 2005. 69:1454–1458.2. Fournier JA, Sanchez A, Quero J, et al. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. 1996. 19:631–636.3. Jeong PH, Lee JY, Yoo BS, et al. Acute myocardial infarction in the young adult. Korean Circ J. 1998. 28:8–12.4. Shiraishi J, Kohno Y, Yamaguchi S, et al. Medium-term prognosis of young Japanese adults having acute myocardial infarction. Circ J. 2006. 70:518–524.5. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996. 93:879–888.6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.7. Morillas P, Bertomeu V, Pabon P, et al. Characteristics and outcome of acute myocardial infarction in young patients. Cardiology. 2007. 107:217–225.8. Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003. 107:2864–2869.9. Barbash GI, White HD, Modan M, et al. Acute myocardial infarction in the young: the role of smoking. Eur Heart J. 1995. 16:313–316.10. Imamura H, Izawa A, Kai R, et al. Trends over the last 20 years in the clinical background of young Japanese patients with coronary artery disease. Circ J. 2004. 68:186–191.11. Ogawa K, Numao T, Iizuka M, et al. Angiographic and coronary risk factor analyses of Japanese patients with ischemic heart disease before age 40: a multicenter cooperative study. Jpn Circ J. 1996. 60:822–830.12. Saigo M, Waters DD, Abe S, et al. Soluble fibrin, C-reactive protein, fibrinogen, factor VII, antithrombin, proteins C and S, tissue factor, D-dimer, and prothrombin fragment 1+2 in men with acute myocardial infarction </=45 years of age. Am J Cardiol. 2004. 94:1410–1413.13. McGill HC Jr, McMahan CA, Herderick EE, et al. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation. 2002. 105:2712–2718.14. Whincup PH, Gilg JA, Donald AE, et al. Arterial distensibility in adolescents: the influence of adiposity, the metabolic syndrome, and classic risk factors. Circulation. 2005. 112:1789–1797.15. Tong W, Lai H, Yang C, Ren S, Dai S, Lai S. Age, gender and metabolic syndrome-related coronary heart disease in U.S. adults. Int J Cardiol. 2005. 104:288–291.16. Chung EH, Curran PJ, Sivasankaran S, et al. Prevalence of metabolic syndrome in patients < or =45 years of age with acute myocardial infarction having percutaneous coronary intervention. Am J Cardiol. 2007. 100:1052–1055.17. Shiraishi J, Kohno Y, Sawada T, et al. Relation of obesity to acute myocardial infarction in Japanese patients. Circ J. 2006. 70:1525–1530.18. Gurm HS, Brennan DM, Booth J, Tcheng JE, Lincoff AM, Topol EJ. Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox). Am J Cardiol. 2002. 90:42–45.19. Powell BD, Lennon RJ, Lerman A, et al. Association of body mass index with outcome after percutaneous coronary intervention. Am J Cardiol. 2003. 91:472–476.20. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction ): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007. 116:e148–e304.21. Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007. 115:450–458.22. Cho JY, Jeong MH, Choi OJ, et al. Predictive factors after percutaneous coronary intervention in young patients with acute myocardial infarction. Korean Circ J. 2007. 37:373–379.23. Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007. 298:309–316.24. Skelding KA, Mehta LS, Pica MC, et al. Primary percutaneous interventions for acute myocardial infarction in octogenarians: a single-center experience. Clin Cardiol. 2002. 25:363–366.25. Sakai K, Nakagawa Y, Kimura T, et al. Comparison of results of coronary angioplasty for acute myocardial infarction in patients > or =75 years of age versus patients <75 years of age. Am J Cardiol. 2002. 89:797–800.26. Zimmerman FH, Cameron A, Fisher LD, Ng G. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry ). J Am Coll Cardiol. 1995. 26:654–661.27. Wolfe MW, Vacek JL. Myocardial infarction in the young: angiographic features and risk factor analysis of patients with myocardial infarction at or before the age of 35 years. Chest. 1988. 94:926–930.28. Genest JJ, McNamara JR, Salem DN, Schaefer EJ. Prevalence of risk factors in men with premature coronary artery disease. Am J Cardiol. 1991. 67:1185–1189.29. Zeller M, Masson D, Farnier M, et al. High serum cholesteryl ester transfer rates and small high-density lipoproteins are associated with young age in patients with acute myocardial infarction. J Am Coll Cardiol. 2007. 50:1948–1955.30. Lim SY, Jeong MH, Yang BR, et al. Long-term clinical outcomes after primary percutaneous coronary intervention in patients with acute myocardial infarction older than 75 years. Korean Circ J. 2005. 35:613–619.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Baseline Lipoprotein(a) Levels and Long-Term Cardiovascular Outcomes After Acute Myocardial Infarction
- Cardiac arrest due to an unexpected acute myocardial infarction during head and neck surgery: A case report
- Impact of Previous Angina on Clinical Outcomes in ST-Elevation Myocardial Infarction Underwent Percutaneous Coronary Intervention
- Impact of Comorbid Disease Burden on Clinical Outcomes of Female Acute Myocardial Infarction Patients
- Clinical Study of Risk Factors in Patients with Acute Myocardial Infarction