J Korean Med Sci.
2023 Apr;38(13):e102. 10.3346/jkms.2023.38.e102.
Baseline Lipoprotein(a) Levels and Long-Term Cardiovascular Outcomes After Acute Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2541043
- DOI: http://doi.org/10.3346/jkms.2023.38.e102
Abstract
- Background
Lipoprotein(a) is a known independent risk factor for atherosclerotic cardiovascular disease. However, the prognostic impact of the baseline lipoprotein(a) levels on long-term clinical outcomes among patients with acute myocardial infarction remain unclear.
Methods
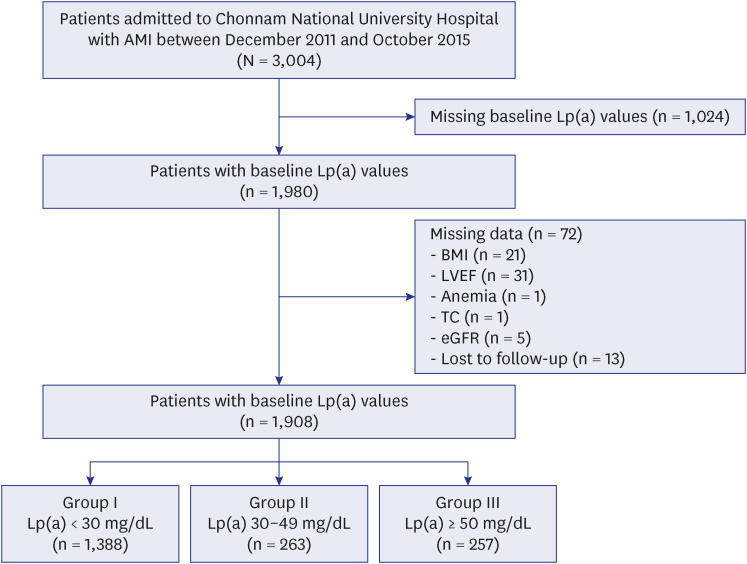
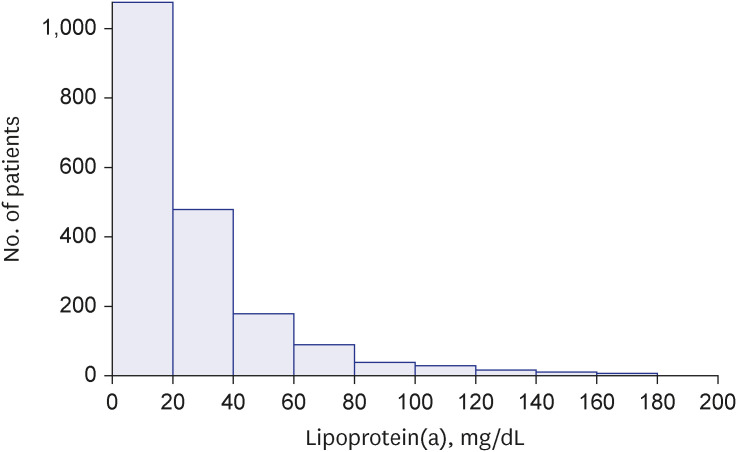
We analyzed 1,908 patients with acute myocardial infarction from November 2011 to October 2015 from a single center in Korea. They were divided into 3 groups according to their baseline lipoprotein(a) levels: groups I (< 30 mg/dL, n = 1,388), II (30–49 mg/dL, n = 263), and III (≥50 mg/dL, n = 257). Three-point major adverse cardiovascular events (a composite of nonfatal myocardial infarction, nonfatal stroke, and cardiac death) at 3 years were compared among the 3 groups.
Results
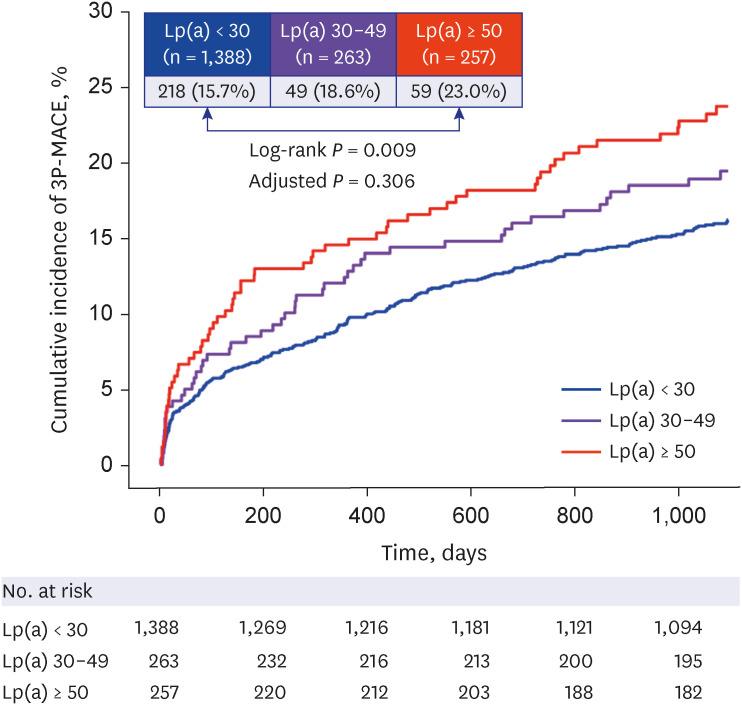
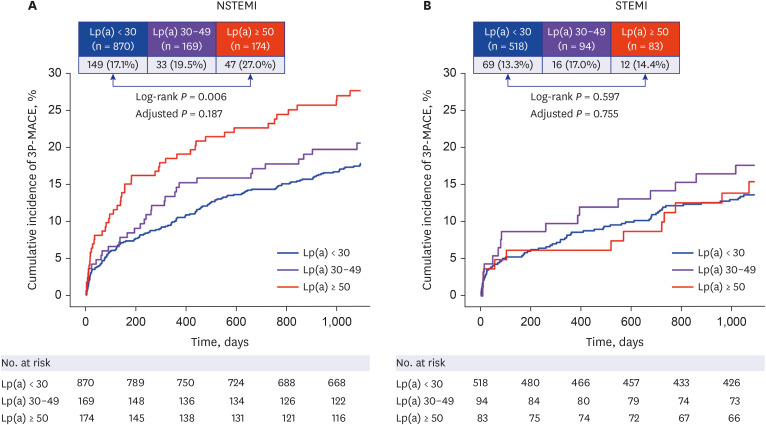
The patients were followed for 1094.0 (interquartile range, 1,033.8–1,095.0) days, during which a total of 326 (17.1%) three-point major adverse cardiovascular events occurred. Group III had higher rates of three-point major adverse cardiovascular events compared with Group I (23.0% vs. 15.7%; log-rank P = 0.009). In the subgroup analysis, group III had higher rates of three-point major adverse cardiovascular events compared with group I in patients with non-ST-segment elevation myocardial infarction (27.0% vs. 17.1%; log-rank P = 0.006), but not in patients with ST-segment elevation myocardial infarction (14.4% vs. 13.3%; logrank P = 0.597). However, in multivariable Cox time-to-event models, baseline lipoprotein(a) levels were not associated with an increased incidence of three-point major adverse cardiovascular events, regardless of the type of acute myocardial infarction. Sensitivity analyses in diverse subgroups showed similar findings to those of the main analysis.
Conclusion
Baseline lipoprotein(a) levels in Korean patients with acute myocardial infarction were not independently associated with increased major adverse cardiovascular events at 3 years.
Keyword
Figure
Reference
-
1. Marcovina SM, Koschinsky ML. Lipoprotein(a) as a risk factor for coronary artery disease. Am J Cardiol. 1998; 82(12A):57U–66U.
Article2. Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009; 302(4):412–423. PMID: 19622820.
Article3. Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009; 301(22):2331–2339. PMID: 19509380.
Article4. Thanassoulis G, Campbell CY, Owens DS, Smith JG, Smith AV, Peloso GM, et al. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med. 2013; 368(6):503–512. PMID: 23388002.
Article5. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019; 73(24):e285–e350. PMID: 30423393.6. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41(1):111–188. PMID: 31504418.7. Boffa MB, Koschinsky ML. Oxidized phospholipids as a unifying theory for lipoprotein(a) and cardiovascular disease. Nat Rev Cardiol. 2019; 16(5):305–318. PMID: 30675027.8. Gallone G, Baldetti L, Pagnesi M, Latib A, Colombo A, Libby P, et al. Medical therapy for long-term prevention of atherothrombosis following an acute coronary syndrome: JACC state-of-the-art review. J Am Coll Cardiol. 2018; 72(23 Pt A):2886–2903. PMID: 30522652.
Article9. Wei WQ, Li X, Feng Q, Kubo M, Kullo IJ, Peissig PL, et al. LPA variants are associated with residual cardiovascular risk in patients receiving statins. Circulation. 2018; 138(17):1839–1849. PMID: 29703846.
Article10. Willeit P, Ridker PM, Nestel PJ, Simes J, Tonkin AM, Pedersen TR, et al. Baseline and on-statin treatment lipoprotein(a) levels for prediction of cardiovascular events: individual patient-data meta-analysis of statin outcome trials. Lancet. 2018; 392(10155):1311–1320. PMID: 30293769.
Article11. O’Donoghue ML, Fazio S, Giugliano RP, Stroes ES, Kanevsky E, Gouni-Berthold I, et al. Lipoprotein(a), PCSK9 inhibition, and cardiovascular Risk. Circulation. 2019; 139(12):1483–1492. PMID: 30586750.12. Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017; 376(18):1713–1722. PMID: 28304224.
Article13. Gencer B, Rigamonti F, Nanchen D, Vuilleumier N, Kern I, Aghlmandi S, et al. Prognostic value of elevated lipoprotein(a) in patients with acute coronary syndromes. Eur J Clin Invest. 2019; 49(7):e13117. PMID: 30937890.
Article14. Roth C, Krychtiuk KA, Gangl C, Schrutka L, Distelmaier K, Wojta J, et al. Lipoprotein(a) plasma levels are not associated with survival after acute coronary syndromes: an observational cohort study. PLoS One. 2020; 15(1):e0227054. PMID: 31917789.15. Zhang M, Liu HH, Jin JL, Yan XN, Dong Q, Li JJ. Lipoprotein(a) and cardiovascular death in oldest-old (≥80 years) patients with acute myocardial infarction: a prospective cohort study. Atherosclerosis. 2020; 312:54–59. PMID: 32977121.16. Takahashi D, Wada H, Ogita M, Yasuda K, Nishio R, Takeuchi M, et al. Impact of lipoprotein(a) as a residual risk factor in long-term cardiovascular outcomes in patients with acute coronary syndrome treated with statins. Am J Cardiol. 2022; 168:11–16. PMID: 35067346.17. Paré G, Çaku A, McQueen M, Anand SS, Enas E, Clarke R, et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation. 2019; 139(12):1472–1482. PMID: 30667276.18. Cho KH, Jeong MH, Ahn Y, Kim YJ, Chae SC, Hong TJ, et al. Low-density lipoprotein cholesterol level in patients with acute myocardial infarction having percutaneous coronary intervention (the cholesterol paradox). Am J Cardiol. 2010; 106(8):1061–1068. PMID: 20920639.19. Cho KH, Kim MC, Choo EH, Choi IJ, Lee SN, Park MW, et al. Impact of low baseline low-density lipoprotein cholesterol on long-term postdischarge cardiovascular outcomes in patients with acute myocardial infarction. J Am Heart Assoc. 2022; 11(17):e025958. PMID: 36000434.20. Markaki I, Nilsson U, Kostulas K, Sjöstrand C. High cholesterol levels are associated with improved long-term survival after acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23(1):e47–e53. PMID: 24103674.
Article21. Kim JH, Chae SC, Oh DJ, Kim HS, Kim YJ, Ahn Y, et al. Multicenter cohort study of acute myocardial infarction in Korea - Interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health Registry. Circ J. 2016; 80(6):1427–1436. PMID: 27118621.22. Cho KH, Shin MH, Kim MC, Sim DS, Hong YJ, Kim JH, et al. Prognostic value of baseline neutrophil-to-lymphocyte ratio combined with anemia in patients with ST-segment elevation myocardial infarction: a nationwide prospective cohort study. J Lipid Atheroscler. 2022; 11(2):147–160. PMID: 35656148.23. Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018; 379(22):2097–2107. PMID: 30403574.24. Schwartz GG, Szarek M, Bittner VA, Diaz R, Goodman SG, Jukema JW, et al. Lipoprotein(a) and benefit of PCSK9 inhibition in patients with nominally controlled LDL cholesterol. J Am Coll Cardiol. 2021; 78(5):421–433. PMID: 34325831.25. Schwartz GG, Ballantyne CM, Barter PJ, Kallend D, Leiter LA, Leitersdorf E, et al. Association of lipoprotein(a) with risk of recurrent ischemic events following acute coronary syndrome: analysis of the dal-outcomes randomized clinical trial. JAMA Cardiol. 2018; 3(2):164–168. PMID: 29071331.26. Mitsuda T, Uemura Y, Ishii H, Takemoto K, Uchikawa T, Koyasu M, et al. Lipoprotein(a) levels predict adverse vascular events after acute myocardial infarction. Heart Vessels. 2016; 31(12):1923–1929. PMID: 26936452.27. Clarke R, Peden JF, Hopewell JC, Kyriakou T, Goel A, Heath SC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009; 361(26):2518–2528. PMID: 20032323.28. Zewinger S, Kleber ME, Tragante V, McCubrey RO, Schmidt AF, Direk K, et al. Relations between lipoprotein(a) concentrations, LPA genetic variants, and the risk of mortality in patients with established coronary heart disease: a molecular and genetic association study. Lancet Diabetes Endocrinol. 2017; 5(7):534–543. PMID: 28566218.29. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39(2):119–177. PMID: 28886621.30. O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 61(4):e78–140. PMID: 23256914.31. Iribarren C, Reed DM, Chen R, Yano K, Dwyer JH. Low serum cholesterol and mortality. Which is the cause and which is the effect? Circulation. 1995; 92(9):2396–2403. PMID: 7586337.32. Matsuoka M, Inoue T, Shinjo T, Miiji A, Tamashiro M, Oba K, et al. Cardiovascular risk profile and frailty in Japanese outpatients: the Nambu Cohort Study. Hypertens Res. 2020; 43(8):817–823. PMID: 32203449.33. Schalk BW, Visser M, Deeg DJ, Bouter LM. Lower levels of serum albumin and total cholesterol and future decline in functional performance in older persons: the Longitudinal Aging Study Amsterdam. Age Ageing. 2004; 33(3):266–272. PMID: 15082432.34. Maeda S, Abe A, Seishima M, Makino K, Noma A, Kawade M. Transient changes of serum lipoprotein(a) as an acute phase protein. Atherosclerosis. 1989; 78(2-3):145–150. PMID: 2476992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical application of stem cell in cardiovascular diseases
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- High Lipoprotein(a) Levels are Associated With Long-Term Adverse Outcomes in Acute Myocardial Infarction Patients in High Killip Classes
- Differences in the Korea Acute Myocardial Infarction Registry Compared with Western Registries
- Long-term Outcomes of Primary Stenting in Acute Myocaridal Infarction