Allergy Asthma Immunol Res.
2020 May;12(3):485-495. 10.4168/aair.2020.12.3.485.
Hospitalization Due to Asthma Exacerbation: A China Asthma Research Network (CARN) Retrospective Study in 29 Provinces Across Mainland China
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, China-Japan Friendship Hospital, Beijing, China. jiangtao_l@263.net
- 2Department of Respiration, Qingdao Municipal Hospital, Qingdao, Shandong, China.
- 3Department of Pulmonary and Critical Care Medicine, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China.
- 4Department of Respiration, The Second Hospital of Hebei Medical University, Shijiazhuang, China.
- 5Department of Respiration, Qinghai People's Hospital, Xining, China.
- 6Department of Respiratory Diseases, General Hospital of Shenyang Military Command, Shenyang, China.
- 7Department of Respiration, The First Affiliated Hospital of Lanzhou University, Lanzhou, China.
- 8Department of Pulmonary and Critical Care Medicine, The Second Hospital of Jilin University, Changchun, China.
- 9Department of Respiration, Tongji Hospital, Wuhan, China.
- 10Department of Respiration, Xinqiao Hospital, Third Military Medical University, Chongqing, China.
- 11Department of Respiration, General Hospital of Ningxia Medical University, Yinchuan, China.
- 12Department of Pulmonary and Critical Care Medicine, Inner Mongolia People's Hospital, Hohhot, China.
- 13Department of Respiration, The First Affiliated Hospital of Guangxi Medical University, Nanning, China.
- 14Department of Respiration, Henan Provincial People's Hospital, Zhengzhou, China.
- 15Department of Pulmonary and Critical Care Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China.
- 16Department of Respiration, The First Affiliated Hospital of Fujian Medical University, Fuzhou, China.
- 17Department of Respiration, Xiangya Hospital, Changsha, China.
- 18Department of Pulmonary and Critical Care Medicine, People's Hospital of Xinjiang Uygur Autonomous Region, Urumqi, China.
- 19Department of Respiration, The First Affiliated Hospital of Harbin Medical University, Harbin China.
- 20Department of Respiration, Guizhou Provincial People's Hospital, Guiyang, China.
- 21Department of Respiration, Shanghai Central Hospital, Shanghai, China.
- 22Department of Respiration, Tianjin First Central Hospital, Tianjin, China.
- 23Department of Respiration, The First Affiliated Hospital of Nanchang University, Nanchang, China.
- 24Department of Respiration, Hainan General Hospital, Haikou, China.
- 25Department of Respiration, Kunming General Hospital of the People's Liberation Army, Kunming, China.
- 26Department of Respiration, The First Affiliated Hospital of Anhui Medical University, Hefei, China.
- 27Department of Respiration, Nanfang Hospital, Guangzhou, China.
- 28Department of Respiration, Shanxi Bethune Hospital, Taiyuan, China.
- 29Department of Respiration, The First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China.
- KMID: 2471231
- DOI: http://doi.org/10.4168/aair.2020.12.3.485
Abstract
- PURPOSE
Details of patients hospitalized for asthma exacerbation in mainland China are lacking. To improve disease control and reduce economic burden, a large sample survey among this patient population is indispensable. This study aimed to investigate the clinical characteristics and outcomes of such patients.
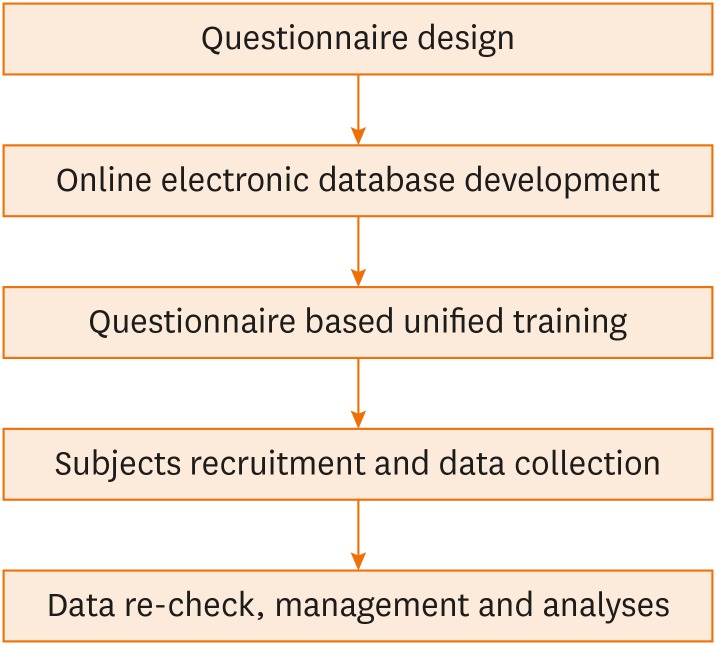
METHODS
A retrospective study was conducted on patients hospitalized for asthma exacerbation in 29 hospitals of 29 regions in mainland China during the period 2013 to 2014. Demographic features, pre-admission conditions, exacerbation details, and outcomes were summarized. Risk factors for exacerbation severity were analyzed.
RESULTS
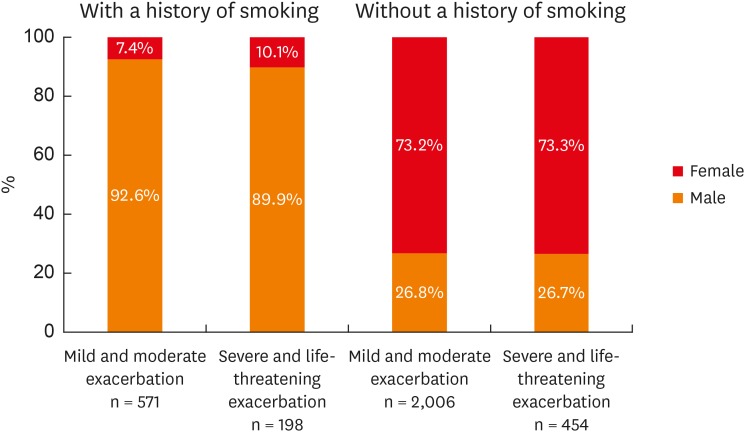
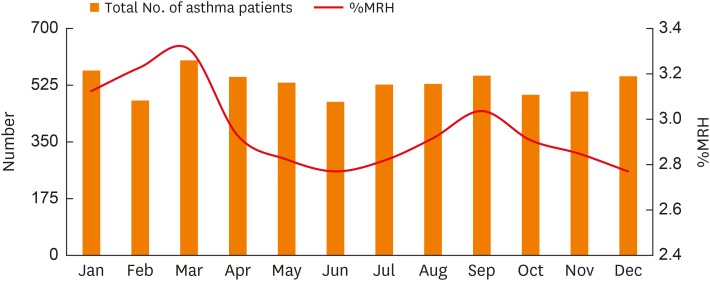
There were 3,240 asthmatic patients included in this study (57.7% females, 42.3% males). Only 28.0% used daily controller medications; 1,287 (39.7%) patients were not currently on inhaled corticosteroids. Acute upper airway infection was the most common trigger of exacerbation (42.3%). Patients with severe to life-threatening exacerbation tended to have a longer disease course, a smoking history, and had comorbidities such as hypertension, chronic obstructive pulmonary disease (COPD), and food allergy. The multivariate analysis showed that smoking history, comorbidities of hypertension, COPD, and food allergy were independent risk factors for more severe exacerbation. The number of patients hospitalized for asthma exacerbation varied with seasons, peaking in March and September. Eight patients died during the study period (mortality 0.25%).
CONCLUSIONS
Despite enhanced education on asthma self-management in China during recent years, few patients were using daily controller medications before the onset of their exacerbation, indicating that more educational efforts and considerations are needed. The findings of this study may improve our understanding of hospital admission for asthma exacerbation in mainland China and provide evidence for decision-making.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones
Asthma*
China*
Comorbidity
Disease Progression
Education
Female
Food Hypersensitivity
Hospitalization*
Humans
Hypertension
Inpatients
Medication Adherence
Mortality
Multivariate Analysis
Pulmonary Disease, Chronic Obstructive
Retrospective Studies*
Risk Factors
Seasons
Self Care
Smoke
Smoking
Adrenal Cortex Hormones
Smoke
Figure
Reference
-
1. Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59:469–478. PMID: 15080825.
Article2. Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2009; 64:476–483. PMID: 19237391.
Article3. Wang WY, Lin JT, Su N, Liu GL, Feng XK, He QY, et al. Survey on the prevalence rate of bronchial asthma in Beijing area among the residents aged over 14 years from 2010 to 2011. Zhonghua Yi Xue Za Zhi. 2013; 93:1383–1387. PMID: 24025502.4. Krishnan V, Diette GB, Rand CS, Bilderback AL, Merriman B, Hansel NN, et al. Mortality in patients hospitalized for asthma exacerbations in the United States. Am J Respir Crit Care Med. 2006; 174:633–638. PMID: 16778163.
Article5. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007; 147:573–577. PMID: 17938396.
Article6. Global Initiative for Asthma. 2012 GINA report, global strategy for asthma management and prevention [Internet]. place unknown: Global Initiative for Asthma;2013. Available from: http://www.ginasthma.org.7. Chinses Medical Association of Respiratory Disease. The guideline for the prevention and treatment of asthma (definition, diagnosis, treatment and management of asthma). Zhonghua Jie He He Hu Xi Za Zhi. 2008; 31:177–185.8. Kaur BP, Lahewala S, Arora S, Agnihotri K, Panaich SS, Secord E, et al. Asthma: hospitalization trends and predictors of in-hospital mortality and hospitalization costs in the USA (2001–2010). Int Arch Allergy Immunol. 2015; 168:71–78. PMID: 26595589.
Article9. Yamauchi Y, Yasunaga H, Matsui H, Hasegawa W, Jo T, Takami K, et al. Comparison of in-hospital mortality in patients with COPD, asthma and asthma-COPD overlap exacerbations. Respirology. 2015; 20:940–946. PMID: 25998444.
Article10. Postma DS. Gender differences in asthma development and progression. Gend Med. 2007; 4 Suppl B:S133–46. PMID: 18156099.
Article11. Boulet LP, FitzGerald JM, McIvor RA, Zimmerman S, Chapman KR. Influence of current or former smoking on asthma management and control. Can Respir J. 2008; 15:275–279. PMID: 18716691.
Article12. Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998; 339:1194–1200. PMID: 9780339.
Article13. Lazarus SC, Chinchilli VM, Rollings NJ, Boushey HA, Cherniack R, Craig TJ, et al. Smoking affects response to inhaled corticosteroids or leukotriene receptor antagonists in asthma. Am J Respir Crit Care Med. 2007; 175:783–790. PMID: 17204725.
Article14. Nong Y, Lin JT, Chen P, Zhou X, Wan HY, Yin KS, et al. The relationship between smoking status and epidermiology of asthma in people aged over 14 years in China. Zhonghua Nei Ke Za Zhi. 2017; 56:485–489. PMID: 28693055.15. Rank MA, Hagan JB, Park MA, Podjasek JC, Samant SA, Volcheck GW, et al. The risk of asthma exacerbation after stopping low-dose inhaled corticosteroids: a systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol. 2013; 131:724–729. PMID: 23321206.16. Johnston NW. The similarities and differences of epidemic cycles of chronic obstructive pulmonary disease and asthma exacerbations. Proc Am Thorac Soc. 2007; 4:591–596. PMID: 18073388.
Article17. Weiss KB. Seasonal trends in US asthma hospitalizations and mortality. JAMA. 1990; 263:2323–2328. PMID: 2325233.
Article18. Lee SW, Lee S, Sheen YH, Ha EK, Choi SH, Yang MS, et al. Seasonal cycle and relationship of seasonal rhino- and influenza virus epidemics with episodes of asthma exacerbation in different age groups. Allergy Asthma Immunol Res. 2017; 9:517–525. PMID: 28913991.
Article19. Sears MR, Johnston NW. Understanding the September asthma epidemic. J Allergy Clin Immunol. 2007; 120:526–529. PMID: 17658590.
Article20. Yao L, Zhang H. Concentration of airborne pollen in Beijing city with burkard sampler. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2009; 23:913–916. PMID: 20128277.21. U.S. Department of Health & Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics. CDC Wonder On-line Database, compiled from Compressed Mortality File 1999–2009. CD-Rom Series 20, No. 20 [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;2012. Available from: https://www.cdc.gov/nchs/data/mortab/1999-2009CMFDocumentationR.pdf.22. To T, Simatovic J, Zhu J, Feldman L, Dell SD, Lougheed MD, et al. Asthma deaths in a large provincial health system. A 10-year population-based study. Ann Am Thorac Soc. 2014; 11:1210–1217. PMID: 25166217.
Article23. Watson L, Turk F, James P, Holgate ST. Factors associated with mortality after an asthma admission: a national United Kingdom database analysis. Respir Med. 2007; 101:1659–1664. PMID: 17462875.
Article24. Bellia V, Pedone C, Catalano F, Zito A, Davì E, Palange S, et al. Asthma in the elderly: mortality rate and associated risk factors for mortality. Chest. 2007; 132:1175–1182. PMID: 17890479.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Bronchiectasis on Asthma Exacerbation
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- Management Practice of Allergic Rhinitis in China During the COVID-19 Pandemic
- Increasing Prevalence of Allergic Rhinitis in China
- Clinical Outcomes after Recovery from Severe Exacerbation in Asthma