Ann Surg Treat Res.
2019 Aug;97(2):83-92. 10.4174/astr.2019.97.2.83.
The Krüppel-like factor (KLF5) as a predictive biomarker in preoperative chemoradiation therapy for rectal cancer
- Affiliations
-
- 1Department of Surgery, Colorectal Cancer Special Clinic, University Health System, Yonsei University College of Medicine, Seoul, Korea. namkyuk@yuhs.ac
- 2Department of Surgery, Dongtan Sacred Heart Hospital, Hallym University Medical Center, Hwasung, Korea.
- 3Department of Biochemistry, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Pathology, Hangang Sacred Heart Hospital, Hallym University Medical Center, Seoul, Korea.
- KMID: 2455982
- DOI: http://doi.org/10.4174/astr.2019.97.2.83
Abstract
- PURPOSE
Preoperative chemoradiation therapy (CRT) has become the standard treatment for patients with locally advanced rectal cancer, 15%-30% of patients still progress while being treated with CRT. The aim of this study was to identify as important biomarker of poor response and evaluate the mechanism associated with CRT resistance.
METHODS
This study included 60 human colon tumour pre-irradiation specimens. Expressions of epidermal growth factor receptor (EGFR), p53, Krüppel-like factor 5 (KLF5), C-ern, Ki67 were assessed and correlated with tumor regression grades and complete remission. We added in vitro study with biomarker which has been identified as important biomarker of poor response to evaluate the mechanism associated with CRT resistance.
RESULTS
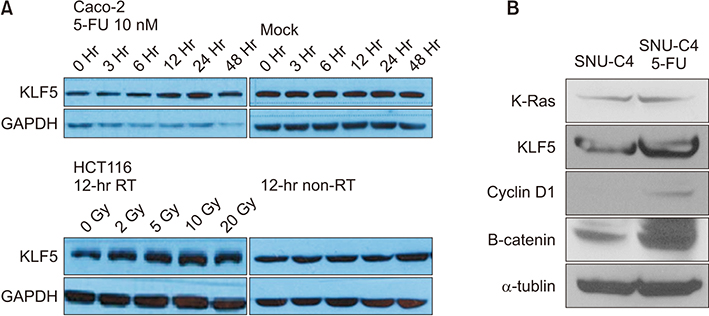
Pathologic complete remission (pCR) was achieved by 9 patients (18%). EGFR and KLF5 were significantly associated with pCR (P = 0.048, P = 0.023, respectfully). And multivariate analysis showed high KLF5 intensity was worse factor for pCR (P = 0.012). In vitro study, radiation or chemotherapy therapy stabilized KLF5 protein levels in a time- and dose-depended manner in HCT116 and Caco-2 cells. KLF5 overexpression in HCT116 stable cell line showed significantly better cell viability by increasing cyclinD1 and b-catenin compared to control cells in MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay, suggesting that KLF5 mediates cell survival.
CONCLUSION
KLF5 was significantly associated with the presence of KRAS mutations, and KLF5 was an independent poor response predictor of CRT in rectal cancer. Our study is pilot study and more research will be needed in the future.
Keyword
MeSH Terms
Figure
Reference
-
1. Swedish Rectal Cancer Trial. Cedermark B, Dahlberg M, Glimelius B, Påhlman L, Rutqvist LE, et al. Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med. 1997; 336:980–987.
Article2. Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radio therapy in rectal cancer. N Engl J Med. 2006; 355:1114–1123.3. Kaminsky-Forrett MC, Conroy T, Luporsi E, Peiffert D, Lapeyre M, Boissel P, et al. Prognostic implications of downstaging following preoperative radiation therapy for operable T3-T4 rectal cancer. Int J Radiat Oncol Biol Phys. 1998; 42:935–941.
Article4. Yoon WH, Kim HJ, Kim CH, Joo JK, Kim YJ, Kim HR. Oncologic impact of pathologic response on clinical outcome after preoperative chemoradiotherapy in locally advanced rectal cancer. Ann Surg Treat Res. 2015; 88:15–20.
Article5. Valentini V, Coco C, Picciocchi A, Morganti AG, Trodella L, Ciabattoni A, et al. Does downstaging predict improved outcome after preoperative chemoradiation for extraperitoneal locally advanced rectal cancer? A long-term analysis of 165 patients. Int J Radiat Oncol Biol Phys. 2002; 53:664–674.
Article6. Reerink O, Karrenbeld A, Plukker JT, Verschueren RC, Szabo BG, Sluiter WJ, et al. Molecular prognostic factors in locally irresectable rectal cancer treated preoperatively by chemo-radiotherapy. Anticancer Res. 2004; 24:1217–1221.7. Crane CH, Skibber JM, Feig BW, Vauthey JN, Thames HD, Curley SA, et al. Response to preoperative chemoradiation increases the use of sphincter-preserving surgery in patients with locally advanced low rectal carcinoma. Cancer. 2003; 97:517–524.
Article8. Wheeler JM, Dodds E, Warren BF, Cunningham C, George BD, Jones AC, et al. Preoperative chemoradiotherapy and total mesorectal excision surgery for locally advanced rectal cancer: correlation with rectal cancer regression grade. Dis Colon Rectum. 2004; 47:2025–2031.
Article9. Huh JW, Park YA, Jung EJ, Lee KY, Sohn SK. Accuracy of endorectal ultrasonography and computed tomography for restaging rectal cancer after preoperative chemoradiation. J Am Coll Surg. 2008; 207:7–12.
Article10. Huh JW, Min JJ, Lee JH, Kim HR, Kim YJ. The predictive role of sequential FDG-PET/CT in response of locally advanced rectal cancer to neoadjuvant chemoradiation. Am J Clin Oncol. 2012; 35:340–344.
Article11. Negri FV, Campanini N, Camisa R, Pucci F, Bui S, Ceccon G, et al. Biological predictive factors in rectal cancer treated with preoperative radiotherapy or radiochemotherapy. Br J Cancer. 2008; 98:143–147.
Article12. Bertolini F, Bengala C, Losi L, Pagano M, Iachetta F, Dealis C, et al. Prognostic and predictive value of baseline and posttreatment molecular marker expression in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:1455–1461.
Article13. Hur H, Kim NK, Min BS, Baik SH, Lee KY, Koom WS, et al. Can a biomarker-based scoring system predict pathologic complete response after preoperative chemoradiotherapy for rectal cancer? Dis Colon Rectum. 2014; 57:592–601.
Article14. Rödel C, Martus P, Papadoupolos T, Fuzesi L, Klimpfinger M, Fietkau R, et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol. 2005; 23:8688–8696.
Article15. Bateman NW, Tan D, Pestell RG, Black JD, Black AR. Intestinal tumor progression is associated with altered function of KLF5. J Biol Chem. 2004; 279:12093–12101.
Article16. Nandan MO, Chanchevalap S, Dalton WB, Yang VW. Kruppel-like factor 5 promotes mitosis by activating the cyclin B1/Cdc2 complex during oncogenic Ras-mediated transformation. FEBS Lett. 2005; 579:4757–4762.17. Nandan MO, Yoon HS, Zhao W, Ouko LA, Chanchevalap S, Yang VW. Krüppel-like factor 5 mediates the transforming activity of oncogenic H-Ras. Oncogene. 2004; 23:3404–3413.
Article18. Nandan MO, McConnell BB, Ghaleb AM, Bialkowska AB, Sheng H, Shao J, et al. Kruppel-like factor 5 mediates cellular transformation during oncogenic KRAS-induced intestinal tumorigenesis. Gastroenterology. 2008; 134:120–130.19. Qiu H, Sirivongs P, Rothenberger M, Rothenberger DA, Garcia-Aguilar J. Molecular prognostic factors in rectal cancer treated by radiation and surgery. Dis Colon Rectum. 2000; 43:451–459.
Article20. Lin JT, Chang TH, Chang CS, Wang WH, Su BW, Lee KD, et al. Prognostic value of pretreatment CD44 mRNA in peripheral blood of patients with locally advanced head and neck cancer. Oral Oncol. 2010; 46:e29–e33.
Article21. Garcia-Aguilar J, Chen Z, Smith DD, Li W, Madoff RD, Cataldo P, et al. Identification of a biomarker profile associated with resistance to neoadjuvant chemoradiation therapy in rectal cancer. Ann Surg. 2011; 254:486–492.
Article22. Rosty C, Young JP, Walsh MD, Clendenning M, Walters RJ, Pearson S, et al. Colorectal carcinomas with KRAS mutation are associated with distinctive morphological and molecular features. Mod Pathol. 2013; 26:825–834.
Article23. Normanno N, Tejpar S, Morgillo F, De Luca A, Van Cutsem E, Ciardiello F. Implications for KRAS status and EGFR-targeted therapies in metastatic CRC. Nat Rev Clin Oncol. 2009; 6:519–527.
Article24. Taieb J, Tabernero J, Mini E, Subtil F, Folprecht G, Van Laethem JL, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol. 2014; 15:862–873.
Article25. Liu Y, Wen JK, Dong LH, Zheng B, Han M. Kruppel-like factor (KLF) 5 mediates cyclin D1 expression and cell proliferation via interaction with c-Jun in Ang II-induced VSMCs. Acta Pharmacol Sin. 2010; 31:10–18.26. Bell KN, Shroyer NF. Krupple-like factor 5 is required for proper maintenance of adult intestinal crypt cellular proliferation. Dig Dis Sci. 2015; 60:86–100.27. Zhao Y, Hamza MS, Leong HS, Lim CB, Pan YF, Cheung E, et al. Kruppel-like factor 5 modulates p53-independent apoptosis through Pim1 survival kinase in cancer cells. Oncogene. 2008; 27:1–8.
Article28. Tut TG, Lim SH, Dissanayake IU, Descallar J, Chua W, Ng W, et al. Upregulated polo-like kinase 1 expression correlates with inferior survival outcomes in rectal cancer. PLoS One. 2015; 10:e0129313.
Article29. Zaborowski A, Stakelum A, Winter DC. Systematic review of outcomes after total neoadjuvant therapy for locally advanced rectal cancer. Br J Surg. 2019; 106:979–987.
Article30. Jiang D, Wang X, Wang Y, Philips D, Meng W, Xiong M, et al. Mutation in BRAF and SMAD4 associated with resistance to neoadjuvant chemoradiation therapy in locally advanced rectal cancer. Virchows Arch. 2019; 475:39–47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CORRIGENDUM: Correction of 4th author's name: The Krüppel-like factor (KLF5) as a predictive biomarker in preoperative chemoradiation therapy for rectal cancer
- Disadvantages of Preoperative Chemoradiation in Rectal Cancer
- How to Achieve a Higher Pathologic Complete Response in Patients With Locally Advanced Rectal Cancer Who Receive Preoperative Chemoradiation Therapy
- The Effects of Preoperative Chemoradiation Therapy in Pectal Cancer
- The Outcome of Preoperative Chemoradiation to Locally Advanced Rectal Cancer