Nutritional Counseling for Obese Children with Obesity-Related Metabolic Abnormalities in Korea
- Affiliations
-
- 1Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Jeju National University Hospital, Jeju, Korea. kskang@jejunu.ac.kr
- KMID: 2384819
- DOI: http://doi.org/10.5223/pghn.2017.20.2.71
Abstract
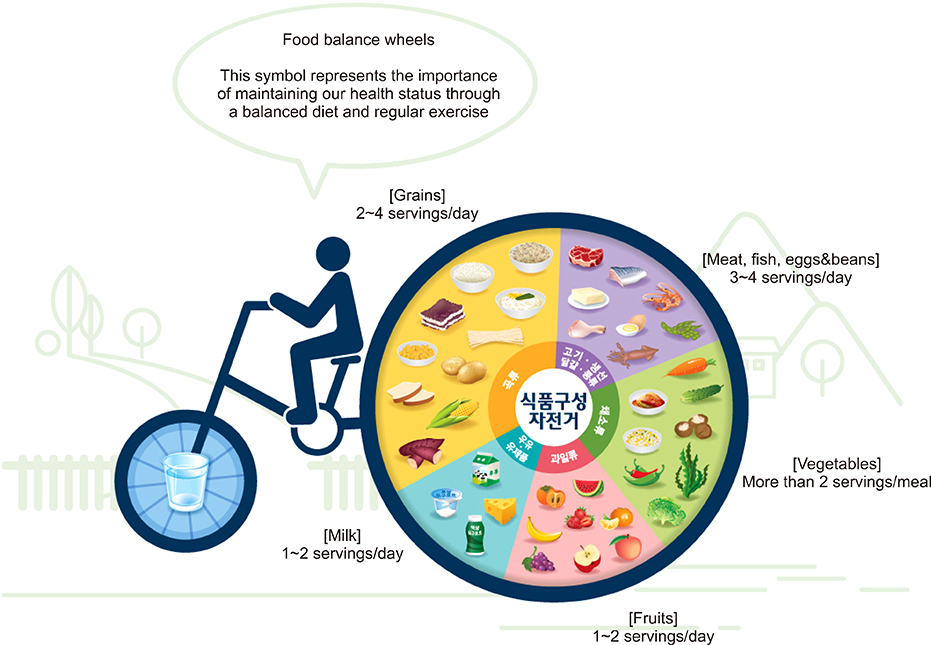
- Child obesity has become a significant health issue in Korea. Prevalence of obesity in school-age children in Korea has been alarmingly rising since 2008. Prevalence of obesity among infants and preschool-age children in Korea has doubled since 2008. Obese children may develop serious health complications. Before nutritional counseling is pursued, several points should be initially considered. The points are modifiable risk factors, assessment for child obesity, and principles of treatment. Motivational interviewing and a multidisciplinary team approach are key principles to consider in managing child obesity effectively in the short-term as well as long-term. Nutritional counseling begins with maintaining a daily log of food and drink intake, which could possibly be causing obesity in a child. Several effective tools for nutritional counseling in practice are the Traffic Light Diet plan, MyPlate, Food Balance Wheel, and "˜Food Exchange Table'. Detailed nutritional counseling supported by a qualified dietitian is an art of medicine enabling insulin therapy and hypoglycemic agents to effectively manage diabetes mellitus in obese children.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Investigation of Clinical and Pathological Relationships between Adult- and Pediatric-type NASH in Korean Children
Jungmin Yoon, Byung Han Park, Ja Hye Kim, Jin-Hwa Moon, Young Ho Lee, Se Min Jang, Yong Joo Kim
J Korean Med Sci. 2018;33(5):. doi: 10.3346/jkms.2018.33.e34.The Analysis of Factors Causing the High Prevalence of Child Obesity in Jeju Island
Eun Hye Park, Min-Su Oh, Sorina Kim, Juyeon Lee, Ki Soo Kang
Pediatr Gastroenterol Hepatol Nutr. 2018;21(2):127-133. doi: 10.5223/pghn.2018.21.2.127.Clinical Practice Guideline for the Diagnosis and Treatment of Pediatric Obesity: Recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition
Dae Yong Yi, Soon Chul Kim, Ji Hyuk Lee, Eun Hye Lee, Jae Young Kim, Yong Joo Kim, Ki Soo Kang, Jeana Hong, Jung Ok Shim, Yoon Lee, Ben Kang, Yeoun Joo Lee, Mi Jin Kim, Jin Soo Moon, Hong Koh, JeongAe You, Young-Sook Kwak, Hyunjung Lim, Hye Ran Yang
Pediatr Gastroenterol Hepatol Nutr. 2019;22(1):1-27. doi: 10.5223/pghn.2019.22.1.1.An Update on Mental Health Problems and Cognitive Behavioral Therapy in Pediatric Obesity
Na Ri Kang, Young Sook Kwack
Pediatr Gastroenterol Hepatol Nutr. 2020;23(1):15-25. doi: 10.5223/pghn.2020.23.1.15.Factors associated with Advanced Bone Age in Overweight and Obese Children
Min-Su Oh, Sorina Kim, Juyeon Lee, Mu Sook Lee, Yoon-Joo Kim, Ki-Soo Kang
Pediatr Gastroenterol Hepatol Nutr. 2020;23(1):89-97. doi: 10.5223/pghn.2020.23.1.89.
Reference
-
1. Keane VA. Assessment of growth. In : Kliegman RM, Stanton BF, St. Geme III JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2016.2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014; 311:806–814.
Article3. European Commission. EU action plan on childhood obesity 2014-2020 [Internet]. European Commission;2014. 02. 24. cited 2017 Jun 2. Available from: https://ec.europa.eu/health/nutrition_physical_activity/key_documents_en#anchor1.4. Ministry of Education, Republic of Korea. Report of student health test results 2016 [Internet]. Seoul: Ministry of Education;2017. cited 2017 Jun 2. Available from: https://goo.gl/kiyZuM.5. National Health Insurance Service, Republic of Korea. The white paper for obesity 2016 [Internet]. Seoul: National Health Insurance Service;2017. cited 2017 Jun 2. Available from: http://www.nhis.or.kr/bbs7/boards/B0039/22703.6. Grant-Guimaraes J, Feinstein R, Laber E, Kosoy J. Childhood overweight and obesity. Gastroenterol Clin North Am. 2016; 45:715–728.
Article7. Skelton J, Cohen G. Obesity. In : Wyllie R, Hyams J, Kay M, editors. Pediatric gastrointestinal and liver disease. 5th ed. Philadelphia: Elsevier;2016.8. Oh MS, Kim S, Jang JH, Park JY, Kang HS, Lee MS, et al. Associations among the degree of nonalcoholic fatty liver disease, metabolic syndrome, degree of obesity in children, and parental obesity. Pediatr Gastroenterol Hepatol Nutr. 2016; 19:199–206.
Article9. Welker E, Lott M, Story M. The school food environment and obesity prevention: progress over the last decade. Curr Obes Rep. 2016; 5:145–155.
Article10. Aceves-Martins M, Llauradó E, Tarro L, Moriña D, Papell-Garcia I, Prades-Tena J. A school-based, peer-led, social marketing intervention to engage Spanish adolescents in a healthy lifestyle (“We are cool”-Som la Pera study): a parallel-cluster randomized controlled study. Child Obes. 2017; DOI: 10.1089/chi.2016.0216. [Epub ahead of print].
Article11. Gahagan S. Overweight and obesity. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2016.12. Kiess W, Blüher S, Kapellen T, Körner A. Metabolic syndrome in children and adolescents: prevalence, public health issue, and time for initiative. J Pediatr Gastroenterol Nutr. 2009; 49:268–271.
Article13. Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004; 350:2362–2374.
Article14. Lambert M, Paradis G, O'Loughlin J, Delvin EE, Hanley JA, Levy E. Insulin resistance syndrome in a representative sample of children and adolescents from Quebec, Canada. Int J Obes Relat Metab Disord. 2004; 28:833–841.
Article15. Butte NF, Comuzzie AG, Cole SA, Mehta NR, Cai G, Tejero M, et al. Quantitative genetic analysis of the metabolic syndrome in Hispanic children. Pediatr Res. 2005; 58:1243–1248.
Article16. Resnicow K, Harris D, Wasserman R, Schwartz RP, Perez-Rosas V, Mihalcea R, et al. Advances in motivational interviewing for pediatric obesity: results of the brief motivational interviewing to reduce body mass index trial and future directions. Pediatr Clin North Am. 2016; 63:539–562.17. Arai L, Panca M, Morris S, Curtis-Tyler K, Lucas PJ, Roberts HM. Time, monetary and other costs of participation in family-based child weight management interventions: qualitative and systematic review evidence. PLoS One. 2015; 10:e0123782.
Article18. Kelleher E, Davoren MP, Harrington JM, Shiely F, Perry IJ, McHugh SM. Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: a systematic review. Obes Rev. 2017; 18:183–194.
Article19. Reid AE, Chauhan BF, Rabbani R, Lys J, Copstein L, Mann A, et al. Early exposure to nonnutritive sweeteners and long-term metabolic health: a systematic review. Pediatrics. 2016; 137:e20153603.
Article20. Lu L, Xun P, Wan Y, He K, Cai W. Long-term association between dairy consumption and risk of childhood obesity: a systematic review and meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2016; 70:414–423.
Article21. Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet. 2010; 376:1775–1784.
Article22. Yon BA, Johnson RK, Harvey-Berino J, Gold BC. The use of a personal digital assistant for dietary self-monitoring does not improve the validity of self-reports of energy intake. J Am Diet Assoc. 2006; 106:1256–1259.
Article23. Dubin SM, Vadivelu J, Copur-Dahi N, Miranda L, Palermo D, Pandey B, et al. A simple dietary questionnaire correlates with formal dietitian evaluation and frequently identifies specific clinical interventions in an outpatient gastroenterology clinic. J Clin Gastroenterol. 2016; 50:e71–e76.
Article24. Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: The National Academies Press;2005. Available from: https://doi.org/10.17226/10490.25. Ministry of Health and Welfare. The Korean Nutrition Society. Dietary reference intakes for Koreans 2015. 3rd ed. Seoul: Ministry of Health and Welfare, The Korean Nutrition Society;2015.26. United States Department of Agriculture. Choose MyPlate.gov [Internet]. Washington, DC: USDA;2011. cited 2017 Jun 1. Available from: https://www.choosemyplate. gov.27. Food and Agriculture Organization of the United Nations. Food-based dietary guidelines [Internet]. Rome: FAO;2017. cited 2017 Jun 2. Available from: http://www.fao.org/nutrition/education/food-dietaryguidelines/home/en/.28. Korean Diabetes Association. User guidelines of food exchange table for diabetes. 3rd ed. Seoul: Korean Diabetes Association;2010.29. Ju DL, Jang HC, Cho YY, Cho JW, Yoo HS, Choi KS, et al. Korean food exchange lists for diabetes: revised 2010. J Nutr Health. 2011; 44:577–591.
Article30. American Diabetes Association. The diabetic exchange list [Internet]. Arlington: American Diabetes Association;cited 2017 Jun 2. Available from: http://glycemic.com/DiabeticExchange/The%20Diabetic%20Exchange%20List.pdf.31. Scott CR, Smith JM, Cradock MM, Pihoker C. Characteristics of youth-onset noninsulin-dependent diabetes mellitus and insulin-dependent diabetes mellitus at diagnosis. Pediatrics. 1997; 100:84–91.
Article32. Connell JE, Thomas-Dobersen D. Nutritional management of children and adolescents with insulin-dependent diabetes mellitus: a review by the diabetes care and education dietetic practice group. J Am Diet Assoc. 1991; 91:1556–1564.
Article33. Svoren BM, Jospe N. Type 2 diabetes mellitus. In : Kliegman RM, Stanton BF, St. Geme III JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2016.34. Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014; 14:508.
Article35. Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Lichtenstein AH, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006; 117:544–559.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Management in Childhood Obesity
- Clinical Predictive Factors for Metabolic Syndrome in Obese Children and Adolescents
- Perioperative Nutritional Management of Morbid Obesity
- The Effect of Problem Solving Group Counseling on the Index of Obesity and Health Habits of Obese Children
- The Influences of Obesity on Bone Mineral Density in Children