J Korean Ophthalmol Soc.
2017 Apr;58(4):430-436. 10.3341/jkos.2017.58.4.430.
Associations between Intraocular Pressure and Systemic Parameters according to the KNHNES 2008-2011
- Affiliations
-
- 1Department of Ophthalmology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. nyny5555@naver.com
- KMID: 2376598
- DOI: http://doi.org/10.3341/jkos.2017.58.4.430
Abstract
- PURPOSE
In this study, we evaluated the associations between intraocular pressure (IOP) and systemic and socioeconomic factors.
METHODS
A population-based cross-sectional study using a nation-wide, stratified, multistage, clustered sampling method included 15,421 subjects aged ≥20 years with no history of ocular surgery or glaucoma who participated in the Korean National Health and Nutritional Examination Survey 2008-2011.
RESULTS
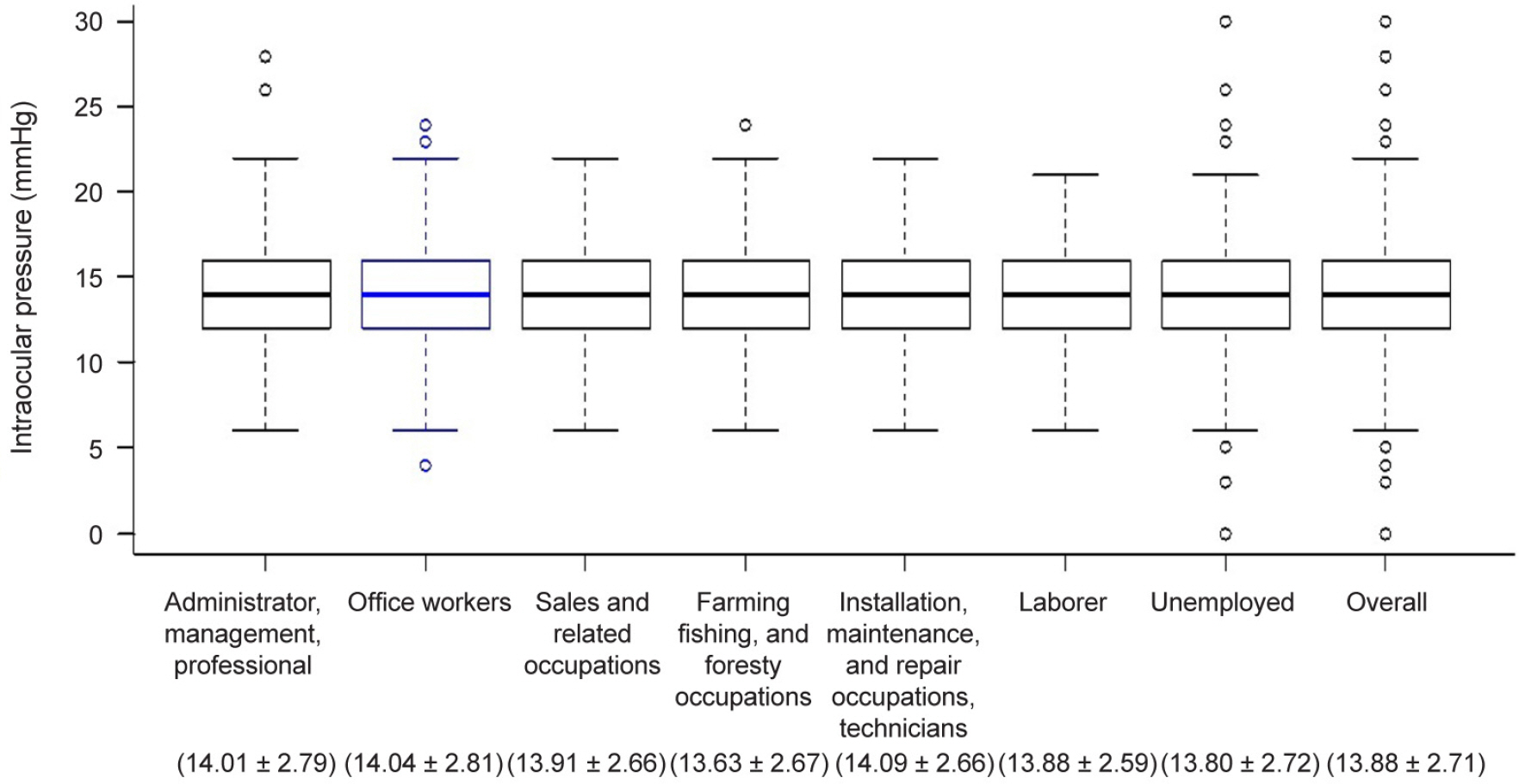
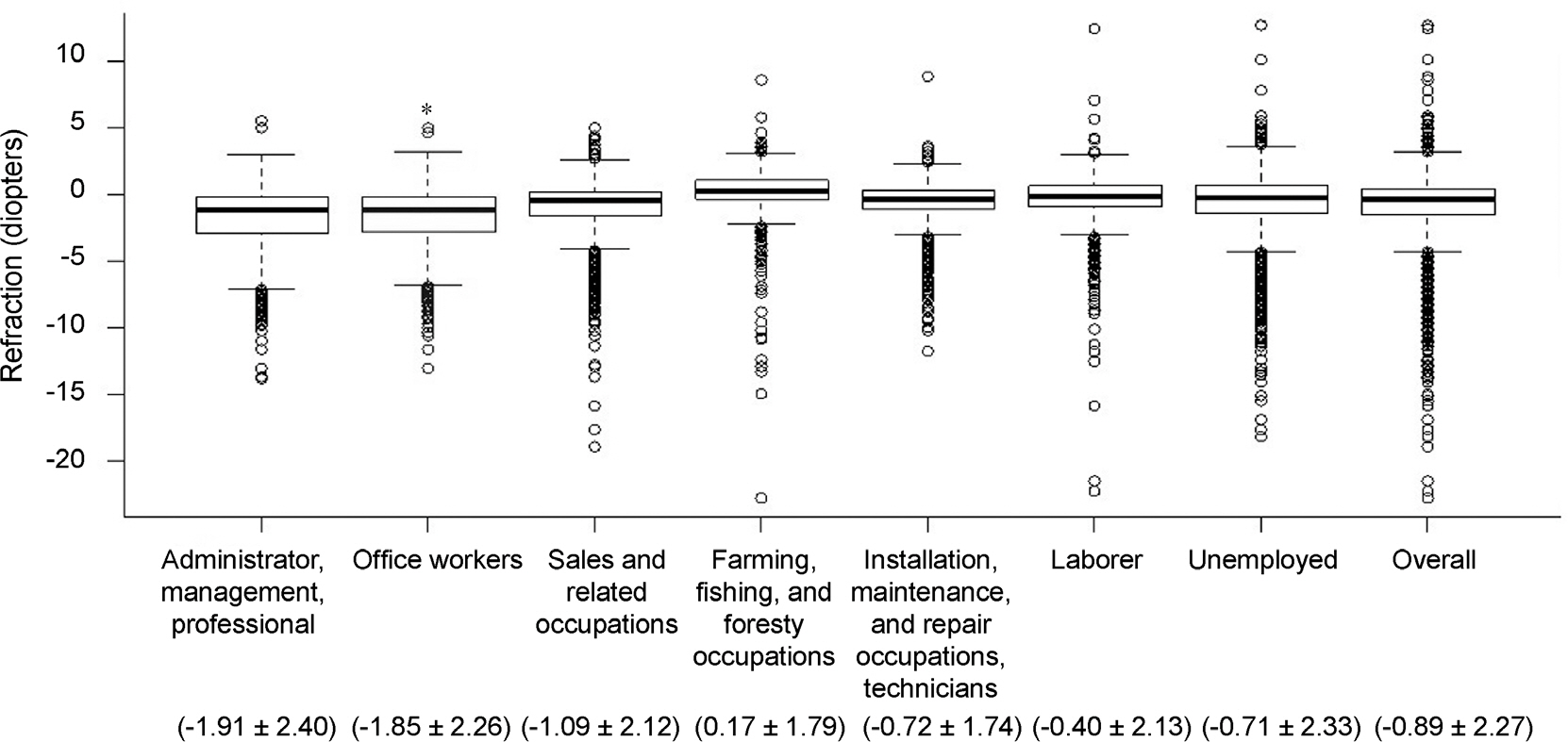
Univariate regression analyses showed statistically significant linear relationships between IOP and body mass index (BMI), smoking status, heavy drinking, systolic blood pressure, fasting blood glucose, total cholesterol, triglycerides, insulin, homeostasis model assessment of insulin resistance (HOMA-IR), metabolic syndrome (p < 0.001, respectively), low density lipoprotein cholesterol (p = 0.003), refractive error (p < 0.001), and office work (p = 0.029). In addition, analysis of variance (ANOVA) showed statistically significant differences in IOP and refraction according to occupation (p < 0.001, all).
CONCLUSIONS
We concluded that increased IOP was associated with age, BMI, heavy drinking, systolic blood pressure, total cholesterol, and refraction. There were statistically significant differences in IOP and refraction according to occupation.
MeSH Terms
-
Blood Glucose
Blood Pressure
Body Mass Index
Cholesterol
Cholesterol, LDL
Cross-Sectional Studies
Drinking
Fasting
Glaucoma
Homeostasis
Insulin
Insulin Resistance
Intraocular Pressure*
Methods
Occupations
Refractive Errors
Smoke
Smoking
Socioeconomic Factors
Triglycerides
Blood Glucose
Cholesterol
Cholesterol, LDL
Insulin
Smoke
Triglycerides
Figure
Reference
-
References
1. Kass MA, Heuer DK, Higginbotham EJ. . The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:701–13. discussion 829-30.2. Higginbotham EJ, Gordon MO, Beiser JA. . The Ocular Hypertension Treatment Study: topical medication delays or pre-vents primary open-angle glaucoma in African American individuals. Arch Ophthalmol. 2004; 122:813–20.3. Sommer A, Tielsch JM, Katz J. . Relationship between intra-ocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol. 1991; 109:1090–5.
Article4. Dielemans I, Vingerling JR, Algra D. . Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population. The Rotterdam Study. Ophthalmology. 1995; 102:54–60.
Article5. Hennis A, Wu SY, Nemesure B. . Hypertension, diabetes, and longitudinal changes in intraocular pressure. Ophthalmology. 2003; 110:908–14.
Article6. Mitchell P, Smith W, Chey T, Healey PR. . Open-angle glaucoma and diabetes: the Blue Mountains eye study, Australia. Ophthalmology. 1997; 104:712–8.7. Aydin P, Oram O, Akman A, Dursun D. . Effect of wind instrument playing on intraocular pressure. J Glaucoma. 2000; 9:322–4.
Article8. Lee E, Yang JW, Kwon JD. . The effect of breath-hold diving on intraocular pressure, optic nerve, visual field in Korean Haenyeo (female divers). J Korean Ophthalmol Soc. 2012; 53:1480–7.
Article9. Jang HD, Kim DH, Han K. . Relationship between intraocular pressure and parameters of obesity in Korean adults: The 2008-2010 Korea National Health and Nutrition Examination Survey. Curr Eye Res. 2015; 40:1008–17.
Article10. Chun YH, Han K, Park SH. . Insulin resistance is associated with intraocular pressure elevation in a non-obese Korean population. PLoS One. 2015; 10:e112929.
Article11. Gwiazda J, Deng L, Dias L. . Association of education and oc-cupation with myopia in COMET parents. Optom Vis Sci. 2011; 88:1045–53.
Article12. Shimizu N, Nomura H, Ando F. . Refractive errors and factors associated with myopia in an adult Japanese population. Jpn J Ophthalmol. 2003; 47:6–12.
Article13. Wong TY, Foster PJ, Johnson GJ, Seah SK. . Education, socio-economic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br J Ophthalmol. 2002; 86:963–8.
Article14. Choi JA, Han K, Park YM, Park CK. . Age-related association of re-fractive error with intraocular pressure in the Korea National Health and Nutrition Examination Survey. PLoS One. 2014; 9:111879.
Article15. Kim KE, Kim MJ, Park KH. . Prevalence, awareness, and risk factors of primary open-angle glaucoma: Korea National Health and Nutrition Examination Survey 2008-2011. Ophthalmology. 2016; 123:532–41.16. Park HA. . The Korea national health and nutrition examination sur-vey as a primary data source. Korean J Fam Med. 2013; 34:79.
Article17. Kim Y, Park S, Kim NS, Lee BK. . Inappropriate survey design analysis of the Korean National Health and Nutrition Examination Survey may produce biased results. J Prev Med Public Health. 2013; 46:96–104.
Article18. Rim HT, Park SY, Yoon JS. . Hormone replacement therapy and eye diseases: KNHANES IV. J Korean Ophthalmol Soc. 2012; 53:1445–50.
Article19. Lim SG, Han K, Kim HA. . Association between insulin resist-ance and periodontitis in Korean adults. J Clin Periodontol. 2014; 41:121–30.
Article20. Kim YK, Tumurbaatar U, Ohn YH. . Cerebrospinal fluid pres-sure and trans-lamina cribrosa pressure difference in open-angle glaucoma: KNHANES V. J Korean Ophthalmol Soc. 2016; 57:1392–9.
Article21. Flammer J, Orgül S, Costa VP. . The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002; 21:359–93.
Article22. Schuman JS, Massicotte EC, Connolly S. . Increased intra-ocular pressure and visual field defects in high resistance wind in-strument players. Ophthalmology. 2000; 107:127–33.
Article23. Baskaran M, Raman K, Ramani KK. . Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners. Ophthalmology. 2006; 113:1327–32.
Article24. Wu SY, Nemesure B, Hennis A. . Nine-year changes in intra-ocular pressure: the Barbados Eye Studies. Arch Ophthalmol. 2006; 124:1631–6.25. Yoshida M, Ishikawa M, Kokaze A. . Association of life-style with intraocular pressure in middle-aged and older Japanese residents. Jpn J Ophthalmol. 2003; 47:191–8.
Article26. Gasch AT, Wang P, Pasquale LR. . Determinants of glaucoma awareness in a general eye clinic. Ophthalmology. 2000; 107:303–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraocular Pressure Changes After Gas Injection into the Rabbit Vitreous Cavity
- Effect of Digital Massage en Intraeeular Pressure
- Changes of Intraocular Pressure after General Anesthesis with Succinylcholine Pretreated with d-Tubocurarine and Pancuronium
- Change in Intraocular Pressure According to Sleeping Posture in Normal People
- Effect of Premedication and Honan Balloon prior to Cataract Surgery on Intraocular Pressure measured by Tono-pen