J Korean Med Sci.
2016 Apr;31(4):542-546. 10.3346/jkms.2016.31.4.542.
Long-term Prognosis of Anti-Neutrophil Cytoplasmic Antibody-Negative Renal Vasculitis: Cohort Study in Korea
- Affiliations
-
- 1Department of Immunology, Seoul National University Postgraduate School, Seoul, Korea. mednep@snubh.org
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2363692
- DOI: http://doi.org/10.3346/jkms.2016.31.4.542
Abstract
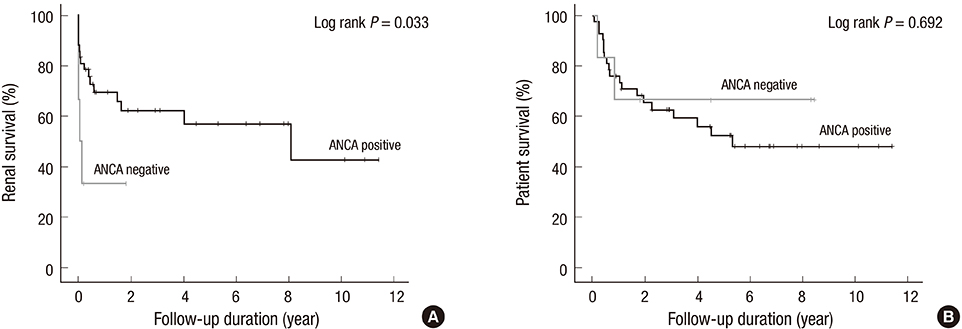
- Few studies have reported on the long-term prognosis of anti-neutrophil cytoplasmic antibody (ANCA)-negative renal vasculitis. Between April 2003 and December 2013, 48 patients were diagnosed with renal vasculitis. Their ANCA status was tested using indirect immunofluorescence and enzyme-linked immunosorbent assays. During a median (interquartile range) follow-up duration of 933.5 (257.5-2,079.0) days, 41.7% of patients progressed to end stage renal disease (ESRD) and 43.8% died from any cause. Of 48 patients, 6 and 42 were ANCA-negative and positive, respectively. The rate of ESRD within 3 months was higher in ANCA-negative patients than in ANCA-positive patients (P = 0.038). In Kaplan-Meier survival analysis, ANCA-negative patients showed shorter renal survival than did ANCA-positive patients (log-rank P = 0.033). In univariate Cox-proportional hazard regression analysis, ANCA-negative patients showed increased risk of ESRD, with a hazard ratio 3.190 (95% confidence interval, 1.028-9.895, P = 0.045). However, the effect of ANCA status on renal survival was not statistically significant in multivariate analysis. Finally, ANCA status did not significantly affect patient survival. In conclusion, long-term patient and renal survival of ANCA-negative renal vasculitis patients did not differ from those of ANCA-positive renal vasculitis patients. Therefore, different treatment strategy depending on ANCA status might be unnecessary.
Keyword
MeSH Terms
-
Age Factors
Aged
Antibodies, Antineutrophil Cytoplasmic/*analysis
Cohort Studies
Enzyme-Linked Immunosorbent Assay
Female
Follow-Up Studies
Humans
Kaplan-Meier Estimate
Kidney Diseases/*diagnosis/mortality
Kidney Failure, Chronic/etiology
Male
Microscopy, Fluorescence
Middle Aged
Prognosis
Proportional Hazards Models
Republic of Korea
Retrospective Studies
Risk Factors
Severity of Illness Index
Sex Factors
Vasculitis/complications/*diagnosis/mortality
Antibodies, Antineutrophil Cytoplasmic
Figure
Cited by 1 articles
-
Antineutrophil Cytoplasmic Antibody-Associated Vasculitis in Korea: A Narrative Review
Chan-Bum Choi, Yong-Beom Park, Sang-Won Lee
Yonsei Med J. 2019;60(1):10-21. doi: 10.3349/ymj.2019.60.1.10.
Reference
-
1. Wilde B, van Paassen P, Witzke O, Tervaert JW. New pathophysiological insights and treatment of ANCA-associated vasculitis. Kidney Int. 2011; 79:599–612.2. Tarzi RM, Cook HT, Pusey CD. Crescentic glomerulonephritis: new aspects of pathogenesis. Semin Nephrol. 2011; 31:361–368.3. Rutgers A, Sanders JS, Stegeman CA, Kallenberg CG. Pauci-immune necrotizing glomerulonephritis. Rheum Dis Clin North Am. 2010; 36:559–572.4. Han JY, Yoon SA, Woo JY, Park IS, Kim SY, Chang YS, Bang BK. ‘Pauci-immune’ rapidly progressive glomerulonephritis associated with systemic vasculitis. J Korean Med Sci. 1992; 7:264–270.5. Chapter 13: pauci-immune focal and segmental necrotizing glomerulonephritis. Kidney Int Suppl. 2011; 2012:233–239.6. Chen M, Yu F, Wang SX, Zou WZ, Zhao MH, Wang HY. Antineutrophil cytoplasmic autoantibody-negative Pauci-immune crescentic glomerulonephritis. J Am Soc Nephrol. 2007; 18:599–605.7. Hung PH, Chiu YL, Lin WC, Chiang WC, Chen YM, Lin SL, Wu KD, Tsai TJ. Poor renal outcome of antineutrophil cytoplasmic antibody negative Pauci-immune glomerulonephritis in Taiwanese. J Formos Med Assoc. 2006; 105:804–812.8. Bajema IM, Hagen EC, Hermans J, Noël LH, Waldherr R, Ferrario F, Van Der Woude FJ, Bruijn JA. Kidney biopsy as a predictor for renal outcome in ANCA-associated necrotizing glomerulonephritis. Kidney Int. 1999; 56:1751–1758.9. Weidner S, Geuss S, Hafezi-Rachti S, Wonka A, Rupprecht HD. ANCA-associated vasculitis with renal involvement: an outcome analysis. Nephrol Dial Transplant. 2004; 19:1403–1411.10. Hauer HA, Bajema IM, van Houwelingen HC, Ferrario F, Noël LH, Waldherr R, Jayne DR, Rasmussen N, Bruijn JA, Hagen EC, et al. Renal histology in ANCA-associated vasculitis: differences between diagnostic and serologic subgroups. Kidney Int. 2002; 61:80–89.11. Little MA, Nazar L, Farrington K. Outcome in glomerulonephritis due to systemic small vessel vasculitis: effect of functional status and non-vasculitic co-morbidity. Nephrol Dial Transplant. 2004; 19:356–364.12. Hedger N, Stevens J, Drey N, Walker S, Roderick P. Incidence and outcome of pauci-immune rapidly progressive glomerulonephritis in Wessex, UK: a 10-year retrospective study. Nephrol Dial Transplant. 2000; 15:1593–1599.13. de Groot K, Gross WL, Herlyn K, Reinhold-Keller E. Development and validation of a disease extent index for Wegener’s granulomatosis. Clin Nephrol. 2001; 55:31–38.14. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–612.15. Oh SW, Kim S, Na KY, Chae DW, Kim S, Jin DC, Chin HJ. Clinical implications of pathologic diagnosis and classification for diabetic nephropathy. Diabetes Res Clin Pract. 2012; 97:418–424.16. Möllsten A, Svensson M, Waernbaum I, Berhan Y, Schön S, Nyström L, Arnqvist HJ, Dahlquist G; Swedish Childhood Diabetes Study Group. Cumulative risk, age at onset, and sex-specific differences for developing end-stage renal disease in young patients with type 1 diabetes: a nationwide population-based cohort study. Diabetes. 2010; 59:1803–1808.17. Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, de Zeeuw D, Shahinfar S, Toto R, Levey AS, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med. 2003; 139:244–252.18. Gatenby PA. Anti-neutrophil cytoplasmic antibody-associated systemic vasculitis: nature or nurture? Intern Med J. 2012; 42:1066–1067.19. Sinico RA, Di Toma L, Radice A. Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. Autoimmun Rev. 2013; 12:477–482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital Apex Syndrome with Perinuclear Anti-neutrophil Cytoplasmic Antibody-associated Pachymeningitis
- Methimazole-Induced Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis in the Peripheral Nerves
- A Case of Membranous Glomerulonephritis with Superimposed Anti-Neutrophil Cytoplasmic Antibody-Associated Rapidly Progressive Crescentic Glomerulonephritis
- Mononeuritis Multiplex in Association with Anti-neutrophil Cytoplasmic Autoantibody(?) Vasculitis: A case report
- A Case of Different Organ Responses to Immunosuppressive Therapy In a Microscopic Polyangiitis Patient with Interstitial Lung Disease