Chonnam Med J.
2015 Aug;51(2):102-105. 10.4068/cmj.2015.51.2.102.
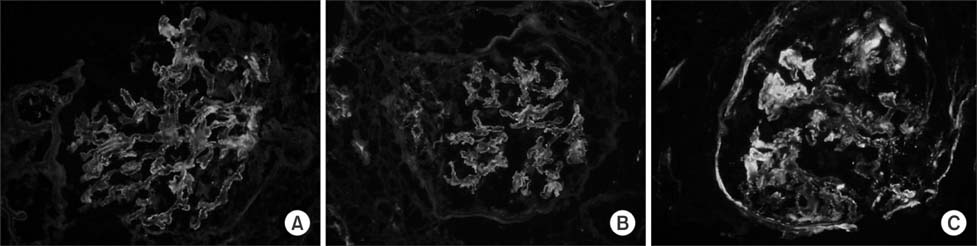
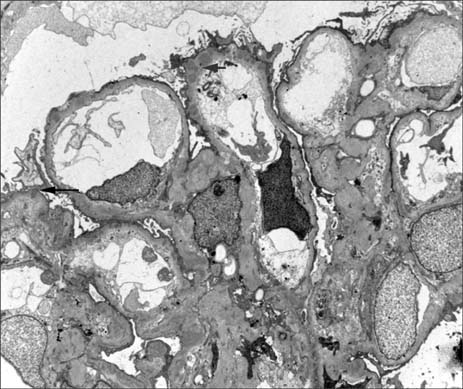
A Case of Membranous Glomerulonephritis with Superimposed Anti-Neutrophil Cytoplasmic Antibody-Associated Rapidly Progressive Crescentic Glomerulonephritis
- Affiliations
-
- 1Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea. drngr@cnu.ac.kr
- KMID: 2172139
- DOI: http://doi.org/10.4068/cmj.2015.51.2.102
Abstract
- Idiopathic membranous glomerulonephritis (IMGN) is commonly diagnosed in adults with proteinuria. Rapid deterioration of renal function is a rare complication of IMGN, except when accompanied by renal vein thrombosis, malignant hypertension, or other underlying disease, including lupus nephritis. Here, we present a case of rapid deterioration of renal function in a patient with MGN superimposed with anti-neutrophil cytoplasmic antibody (ANCA)-associated rapidly progressive crescentic glomerulonephritis (RPGN). Overall, about 20 cases of MGN with ANCA-associated RPGN have been reported. This case of biopsy-proven MGN with ANCA-associated RPGN is the first to be reported in Korea.
Keyword
MeSH Terms
-
Adult
Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis
Antibodies
Antibodies, Antineutrophil Cytoplasmic
Cytoplasm*
Glomerulonephritis*
Glomerulonephritis, Membranous*
Humans
Hypertension, Malignant
Korea
Lupus Nephritis
Membranes
Proteinuria
Renal Veins
Thrombosis
Antibodies
Antibodies, Antineutrophil Cytoplasmic
Figure
Reference
-
1. Ponticelli C. Membranous nephropathy. J Nephrol. 2007; 20:268–287.2. James SH, Lien YH, Ruffenach SJ, Wilcox GE. Acute renal failure in membranous glomerulonephropathy: a result of superimposed crescentic glomerulonephritis. J Am Soc Nephrol. 1995; 6:1541–1546.
Article3. Tse WY, Howie AJ, Adu D, Savage CO, Richards NT, Wheeler DC, et al. Association of vasculitic glomerulonephritis with membranous nephropathy: a report of 10 cases. Nephrol Dial Transplant. 1997; 12:1017–1027.
Article4. Kim TW, Park KK, Lee IH. A case of idiopathic membranous nephropathy with crescents formation associated with anti-gbm antibody. Korean J Nephrol. 2010; 29:628–633.5. Lim SH, Kwon HH, Park KC, Ryu JI, You SS, Park MS, et al. A case of crescentric glomerulonephritis superimposed on preexisting membranous nephropathy. Korean J Nephrol. 2002; 21:820–825.6. Haas M, Eustace JA. Immune complex deposits in ANCA-associated crescentic glomerulonephritis: a study of 126 cases. Kidney Int. 2004; 65:2145–2152.
Article7. Basford AW, Lewis J, Dwyer JP, Fogo AB. Membranous nephropathy with crescents. J Am Soc Nephrol. 2011; 22:1804–1808.
Article8. Cameron JS. Membranous nephropathy--still a treatment dilemma. N Engl J Med. 1992; 327:638–639.9. Jayne DR, Gaskin G, Rasmussen N, Abramowicz D, Ferrario F, Guillevin L, et al. European Vasculitis Study Group. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007; 18:2180–2188.
Article10. Nasr SH, Said SM, Valeri AM, Stokes MB, Masani NN, D'Agati VD, et al. Membranous glomerulonephritis with ANCA-associated necrotizing and crescentic glomerulonephritis. Clin J Am Soc Nephrol. 2009; 4:299–308.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Crescentic Glomerulonephritis with Coexisting Anti-Glomerular Basement Membrane Antibodies and Myeloperoxidase-Anti-Neutrophil Cytoplasmic Autoantibodies
- Crescentic glomerulonephritis: a clinicopathologic analysis of 17 cases with emphasis on glomerular and interstitial neutrophil infiltration
- A Case of Rapidly Progressive Glomerulonephritis Associated with Hepatitis C Virus
- 'Pauci-immune' rapidly progressive glomerulonephritis associated with systemic vasculitis
- Overview of IgG4-Related Tubulointerstitial Nephritis and Its Mimickers