Role of random biopsies in surveillance of dysplasia in ulcerative colitis patients with high risk of colorectal cancer
- Affiliations
-
- 1Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India. vins_ahuja@hotmail.com
- 2Department of Pathology, All India Institute of Medical Sciences, New Delhi, India.
- 3Department of Biostatistics, All India Institute of Medical Sciences, New Delhi, India.
- KMID: 2354969
- DOI: http://doi.org/10.5217/ir.2016.14.3.264
Abstract
- BACKGROUND/AIMS
Recent data suggest that the incidence of ulcerative colitis (UC) related colorectal cancer (CRC) in India is similar to that of West. The optimum method for surveillance is still a debate. Surveillance with random biopsies has been the standard of care, but is a tedious process. We therefore undertook this study to assess the yield of random biopsy in dysplasia surveillance.
METHODS
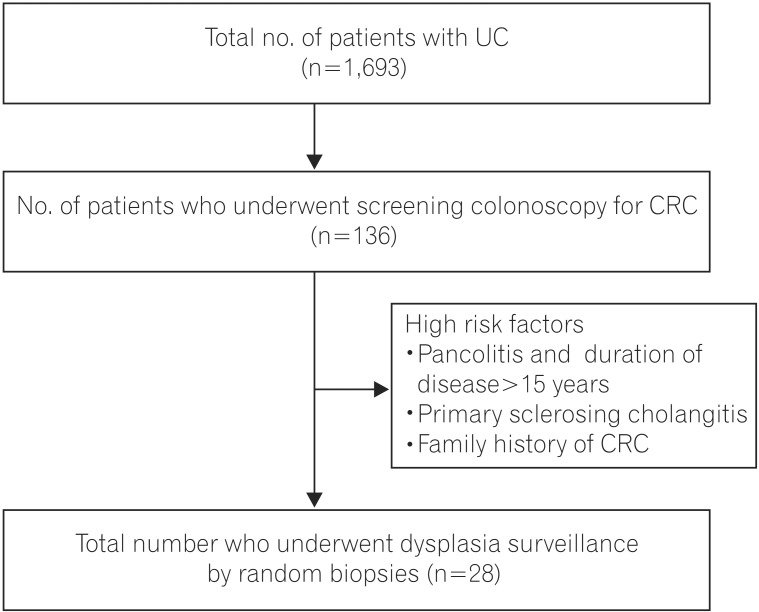
Between March 2014 and July 2015, patients of UC attending the Inflammatory Bowel Disease clinic at the All India Institute of Medical Sciences with high risk factors for CRC like duration of disease >15 years and pancolitis, family history of CRC, primary sclerosing cholangitis underwent surveillance colonoscopy for dysplasia. Four quadrant random biopsies at 10 cm intervals were taken (33 biopsies). Two pathologists examined specimens for dysplasia, and the yield of dysplasia was calculated.
RESULTS
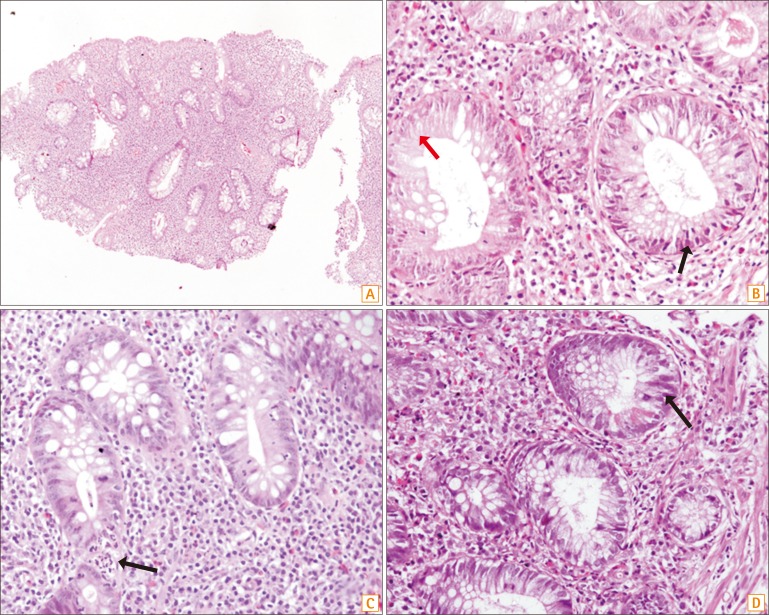
Twenty-eight patients were included. Twenty-six of these had pancolitis with a duration of disease greater than 15 years, and two patients had associated primary sclerosing cholangis. No patient had a family history of CRC. The mean age at onset of disease was 28.89±8.73 years and the duration of disease was 19.00±8.78 years. Eighteen patients (64.28%) were males. A total of 924 biopsies were taken. None of the biopsies revealed any evidence of dysplasia, and 7/924 (0.7%) were indefinite for dysplasia.
CONCLUSIONS
Random biopsy for surveillance in longstanding extensive colitis has a low yield for dysplasia and does not suffice for screening. Newer techniques such as chromoendoscopy-guided biopsies need greater adoption.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Screening strategy for colorectal cancer according to risk
Dong Soo Han
J Korean Med Assoc. 2017;60(11):893-898. doi: 10.5124/jkma.2017.60.11.893.Safety and effectiveness of adalimumab in the treatment of ulcerative colitis: results from a large-scale, prospective, multicenter, observational study
Haruhiko Ogata, Takashi Hagiwara, Takeshi Kawaberi, Mariko Kobayashi, Toshifumi Hibi
Intest Res. 2021;19(4):419-429. doi: 10.5217/ir.2020.00033.Low prevalence of primary sclerosing cholangitis in patients with inflammatory bowel disease in India
Arshdeep Singh, Vandana Midha, Vikram Narang, Saurabh Kedia, Ramit Mahajan, Pavan Dhoble, Bhavjeet Kaur Kahlon, Ashvin Singh Dhaliwal, Ashish Tripathi, Shivam Kalra, Narender Pal Jain, Namita Bansal, Rupa Banerjee, Devendra Desai, Usha Dutta, Vineet Ahuja, Ajit Sood
Intest Res. 2023;21(4):452-459. doi: 10.5217/ir.2022.00087.
Reference
-
1. Ahuja V, Tandon RK. Inflammatory bowel disease: the Indian augury. Indian J Gastroenterol. 2012; 31:294–296. PMID: 23150035.
Article2. Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010; 11:134–147. PMID: 20579217.
Article3. Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001; 48:526–535. PMID: 11247898.
Article4. Desai D, Shah S, Deshmukh A, et al. Colorectal cancers in ulcerative colitis from a low-prevalence area for colon cancer. World J Gastroenterol. 2015; 21:3644–3649. PMID: 25834332.
Article5. Lutgens MW, Oldenburg B, Siersema PD, et al. Colonoscopic surveillance improves survival after colorectal cancer diagnosis in inflammatory bowel disease. Br J Cancer. 2009; 101:1671–1675. PMID: 19826420.
Article6. Cairns SR, Scholefield JH, Steele RJ, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010; 59:666–689. PMID: 20427401.
Article7. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012; 6:965–990. PMID: 23040452.
Article8. Rubin CE, Haggitt RC, Burmer GC, et al. DNA aneuploidy in colonic biopsies predicts future development of dysplasia in ulcerative colitis. Gastroenterology. 1992; 103:1611–1620. PMID: 1426881.
Article9. Kiesslich R, Fritsch J, Holtmann M, et al. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003; 124:880–888. PMID: 12671882.
Article10. Kiesslich R, Neurath MF. Magnifying chromoendoscopy: effective diagnostic tool for screening colonoscopy. J Gastroenterol Hepatol. 2007; 22:1700–1701. PMID: 17914935.
Article11. Picco MF, Pasha S, Leighton JA, et al. Procedure time and the determination of polypoid abnormalities with experience: implementation of a chromoendoscopy program for surveillance colonoscopy for ulcerative colitis. Inflamm Bowel Dis. 2013; 19:1913–1920. PMID: 23811635.12. Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998; 43:29–32. PMID: 9771402.
Article13. Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000; 47:251–255. PMID: 10896917.
Article14. Ekbom A, Helmick C, Zack M, Adami HO. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med. 1990; 323:1228–1233. PMID: 2215606.15. Rutter M, Bernstein C, Matsumoto T, Kiesslich R, Neurath M. Endoscopic appearance of dysplasia in ulcerative colitis and the role of staining. Endoscopy. 2004; 36:1109–1114. PMID: 15578305.
Article16. Leung K, Pinsky P, Laiyemo AO, Lanza E, Schatzkin A, Schoen RE. Ongoing colorectal cancer risk despite surveillance colonoscopy: the Polyp Prevention Trial Continued Follow-up Study. Gastrointest Endosc. 2010; 71:111–117. PMID: 19647250.
Article17. Ueno Y, Tanaka S, Chayama K. Non-polypoid colorectal neoplasms in ulcerative colitis. Gastrointest Endosc Clin N Am. 2010; 20:525–542. PMID: 20656250.
Article18. Sharan R, Schoen RE. Cancer in inflammatory bowel disease. An evidence-based analysis and guide for physicians and patients. Gastroenterol Clin North Am. 2002; 31:237–254. PMID: 12122735.19. Rutter MD, Saunders BP, Wilkinson KH, Kamm MA, Williams CB, Forbes A. Most dysplasia in ulcerative colitis is visible at colonoscopy. Gastrointest Endosc. 2004; 60:334–339. PMID: 15332019.
Article20. Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastrointest Endosc. 2015; 81:489–501. PMID: 25708752.
Article21. Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY, et al. Chromoendoscopy for surveillance in inflammatory bowel disease does not increase neoplasia detection compared with conventional colonoscopy with random biopsies: results from a large retrospective study. Am J Gastroenterol. 2015; 110:1014–1021. PMID: 25823770.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Advances in Understanding Colorectal Cancer and Dysplasia Related to Ulcerative Colitis
- Colonoscopic Cancer Surveillance in Inflammatory Bowel Disease: What's New Beyond Random Biopsy?
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis
- A Case of Polyp with High Grade Dysplasia in Ulcerative Colitis
- A Case of Cholangiocarcinoma and Colorectal Cancer Diagnosed Simultaneously in a Patient with Ulcerative Colitis and Concurrent Primary Sclerosing Cholangitis