J Dent Anesth Pain Med.
2016 Sep;16(3):217-222. 10.17245/jdapm.2016.16.3.217.
Use of ADMSâ„¢ during sedation for dental treatment of an intellectually disabled patient: a case report
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea. stone90@snu.ac.kr
- 2Research Institute, Unimedics CO., LTD., Seoul, Korea.
- 3Special Care Clinic, Seoul National University Dental Hospital, Seoul, Korea.
- KMID: 2354659
- DOI: http://doi.org/10.17245/jdapm.2016.16.3.217
Abstract
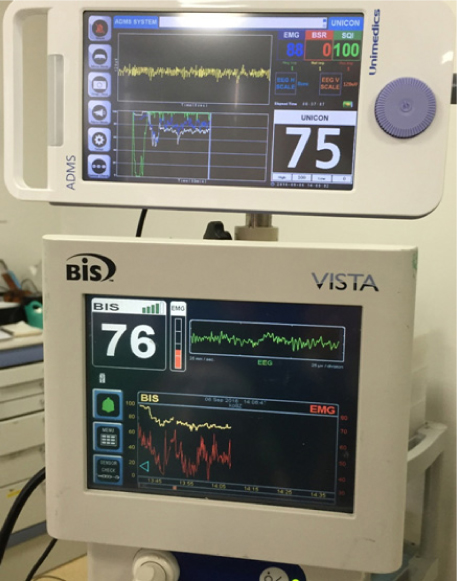
- Dental treatment is often performed under general anesthesia or sedation when an intellectually disabled patient has a heightened fear of treatment or has difficulty cooperating. When it is impossible to control the patient due to the severity of intellectual disability, conscious sedation is not a viable option, and only deep sedation should be performed. Deep sedation is usually achieved by propofol infusion using the target controlled infusion (TCI) system, with deep sedation being achieved at a slightly lower concentration of propofol in disabled patients. In such cases, anesthesia depth monitoring using EEG, as with a Bispectral Index (BIS) monitor, can enable dental treatment under appropriate sedation depth. In the present case, we performed deep sedation for dental treatment on a 27-year-old female patient with mental retardation and severe dental phobia. During sedation, we used BIS and a newly developed Anesthetic Depth Monitor for Sedation (ADMSâ„¢), in addition to electrocardiography, pulse oximetry, blood pressure monitoring, and capnometry for patient safety. Oxygen was administered via nasal prong to prevent hypoxemia during sedation. The BIS and ADMSâ„¢ values were maintained at approximately 70, and dental treatment was successfully performed in approximately 30 min..
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effects site concentrations of propofol using target-controlled infusion in dental treatment under deep sedation among different intellectual disability types
Keyling S. Salinas Salmeron, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2019;19(4):217-226. doi: 10.17245/jdapm.2019.19.4.217.
Reference
-
1. Caputo AC. Providing deep sedation and general anesthesia for patients with special needs in the dental office-based setting. Spec Care Dentist. 2009; 29:26–30.
Article2. Romer M. Consent, restraint, and people with special needs: A review. Spec Care Dentist. 2009; 29:58–66.3. Gordon SM, Dionne RA, Snyder J. Dental fear and anxiety as a barrier to accessing oral health care among patients with special health care needs. Spec Care Dentist. 1998; 18:88–92.4. Bing JH, Jeon JY, Jung SH, Hwang KG, Park CJ, Seo KS, et al. Sedation for dental treatment of patients with disabilities. J Korean Dent Soc Anesthesiol. 2007; 7:114–119.
Article5. Malamed SF, Gottschalk HW, Mulligan R, Quinn CL. Intravenous sedation for conservative dentistry for disabled patients. Anesth Prog. 1989; 36:140–142.
Article6. Lee BS, Shin TJ, Kim HJ, Choi YJ, Lee SE, Chang J, et al. Effect site concentrations of propofol for dental treatment under deep sedation in intellectually disabled patients. J Korean Dent Soc Anesthesiol. 2014; 14:167–172.
Article7. Donaldson M, Goodchild JH. Use of bispectral index system (bis) to monitor enteral conscious (moderate) sedation during general dental procedures. J Can Dent Assoc. 2009; 75:709.
Article8. Malviya S, Voepel-Lewis T, Prochaska G, Tait AR. Prolonged recovery and delayed side effects of sedation for diagnostic imaging studies in children. Pediatrics. 2000; 105:e42.
Article9. Liu J, Singh H, White PF. Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofol-induced sedation. Anesth Analg. 1997; 84:185–189.
Article10. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2007; CD003843.11. Klopman MA, Sebel PS. Cost-effectiveness of bispectral index monitoring. Curr Opin Anaesthesiol. 2011; 24:177–181.12. Messieha ZS, Ananda RC, Hoffman WE, Punwani IC, Koenig HM. Bispectral index system (bis) monitoring reduces time to discharge in children requiring intramuscular sedation and general anesthesia for outpatient dental rehabilitation. Pediatr Dent. 2004; 26:256–260.
Article13. Haenggi M, Ypparila-Wolters H, Hauser K, Caviezel C, Takala J, Korhonen I, et al. Intra- and inter-individual variation of bis-index and entropy during controlled sedation with midazolam/remifentanil and dexmedetomidine/remifentanil in healthy volunteers: An interventional study. Crit Care. 2009; 13:R20.
Article14. Shah P, Manley G, Craig D. Bispectral index (bis) monitoring of intravenous sedation for dental treatment. SAAD Dig. 2014; 30:7–11.
Article15. Yang Z, Wang Y, Ouyang G. Adaptive neuro-fuzzy inference system for classification of background eeg signals from eses patients and controls. ScientificWorldJournal. 2014; 2014:140863.
Article16. Rampil IJ, Kim JS, Lenhardt R, Negishi C, Sessler DI. Bispectral eeg index during nitrous oxide administration. Anesthesiology. 1998; 89:671–677.
Article17. Dahaba AA. Different conditions that could result in the bispectral index indicating an incorrect hypnotic state. Anesth Analg. 2005; 101:765–773.
Article18. Pilge S, Zanner R, Schneider G, Blum J, Kreuzer M, Kochs EF. Time delay of index calculation: Analysis of cerebral state, bispectral, and narcotrend indices. Anesthesiology. 2006; 104:488–494.
Article19. Vivien B, Di Maria S, Ouattara A, Langeron O, Coriat P, Riou B. Overestimation of bispectral index in sedated intensive care unit patients revealed by administration of muscle relaxant. Anesthesiology. 2003; 99:9–17.
Article20. Baldesi O, Bruder N, Velly L, Gouin F. Spurious bispectral index values due to electromyographic activity. Eur J Anaesthesiol. 2004; 21:324–325.
Article21. Deogaonkar A, Gupta R, DeGeorgia M, Sabharwal V, Gopakumaran B, Schubert A, et al. Bispectral index monitoring correlates with sedation scales in brain-injured patients. Crit Care Med. 2004; 32:2403–2406.
Article22. Renna M, Handy J, Shah A. Low baseline bispectral index of the electroencephalogram in patients with dementia. Anesth Analg. 2003; 96:1380–1385.
Article23. Choudhry DK, Brenn BR. Bispectral index monitoring: A comparison between normal children and children with quadriplegic cerebral palsy. Anesth Analg. 2002; 95:1582–1585.
Article24. Valkenburg AJ, de Leeuw TG, Tibboel D, Weber F. Lower bispectral index values in children who are intellectually disabled. Anesth Analg. 2009; 109:1428–1433.
Article25. Pandit JJ, Schmelzle-Lubiecki B, Goodwin M, Saeed N. Bispectral index-guided management of anaesthesia in permanent vegetative state. Anaesthesia. 2002; 57:1190–1194.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dental treatment under general anesthesia in an intellectually disabled child with intellectually disabled parents
- Effect Site Concentrations of Propofol for Dental Treatment under Deep Sedation in Intellectually Disabled Patients
- Airway management during general anesthesia in an intellectually disabled patient with undiagnosed tracheomalacia
- Use of Sevoflurane Inhalation Sedation for Disabled Outpatient Dental Treatment
- Application of sevoflurane inhalation sedation in dental treatment: a mini review