J Dent Anesth Pain Med.
2018 Apr;18(2):119-123. 10.17245/jdapm.2018.18.2.119.
Airway management during general anesthesia in an intellectually disabled patient with undiagnosed tracheomalacia
- Affiliations
-
- 1Department of Advanced General Dentistry, School of Dentistry, Dankook University, Cheonan, Korea.
- 2Department of Anesthesiololgy, School of Dentistry, Dankook University, Cheonan, Korea. ksomd@dankook.ac.kr
- KMID: 2410146
- DOI: http://doi.org/10.17245/jdapm.2018.18.2.119
Abstract
- In cases of intellectually disabled patients, there is sometimes difficult to obtain sufficient information due to the intellectual disorder, even though the patient has significant medical problems. Herein, we report a case of decreased oxygen saturation and inadequate air exchange during general anesthesia in an intellectually disabled patient. We also describe the subsequent management, including the diagnosis of tracheomalacia (TM) using bronchoscopy, and the management of airway compromise with manual and/or controlled respiration, which led to the prevention of complications.
MeSH Terms
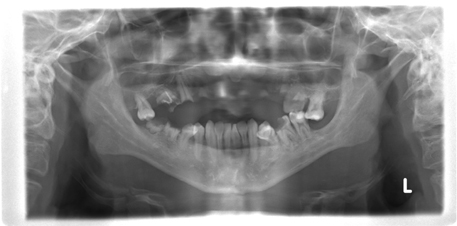
Figure
Reference
-
1. Johnson TH, Mikita JJ, Wilson RJ, Feist JH. Acquired tracheomalacia. Radiology. 1973; 109:576–580.
Article2. Carden KA, Boiselle PM, Waltz D, Ernst A. Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest. 2005; 127:984–1005.
Article3. Wright CD. Tracheomalacia. Chest Surg Clin N Am. 2003; 13:349–357.
Article4. Czyhlarz ER. Ueber ein pulsiondivertikel der trachea mit bemerkungen uber das verhalten der elastichen fasern an normalen tracheen und brounchein. Zentralbl Allg pathol. 1897; 18:721–728.5. Mounier-Kuhn P. Dilation de al trachee: Constantations rudui-graphiques et bronchoscopiques. Lyons Medical. 1932; 150:106–109.6. Jokinen K, Palva T, Sutinen S, Nuutinen J. Acquired tracheobronchomalacia. Ann Clin Res. 1977; 9:52–57.7. Jacobs IN, Wetmore RF, Tom LW. Tracheobronchomalacia in children. Arch Otolaryngol Head Neck Surg. 1994; 120:154–158.
Article8. Mose CA, Izukawa T, Trusler GA. Innominate artery compression of the trachea. Arch Otolaryngol. 1975; 101:733–738.
Article9. Cohen D. Tracheopexy-tracheal suspension for severe tracheomalacia. Aust Paediatr J. 1981; 17:117–121.10. Creenholz DK, Karrer FM, Lilly JR. Contemporary surgery of tracheomalacia. J Pediatr Surg. 1986; 21:511–514.
Article11. Feist JH, Johnson TH, Wilson RJ. Acquired tracheomalacia: etiology and differential diagnosis. Chest. 1975; 68:340–345.
Article12. Proctor H. The stove-in chest with paradoxical respiration. Br J Surg. 1955; 42:622–633.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dental treatment under general anesthesia in an intellectually disabled child with intellectually disabled parents
- Reversible airway obstruction caused by changing the size and length of an endotracheal tube in a premature neonate with suspected tracheomalacia: A case report
- Successful Intubation with Intra-Oral Camera in Difficult Intubation Case
- A Survey of Dental Treatment under General Anesthesia in Division of Pediatric Dentistry, Ajou University Hospital
- Successful Management of Acquired Tracheomalacia of Patients With Amyotrophic Lateral Sclerosis: A Report of Three Cases