Korean Circ J.
2009 Nov;39(11):488-493. 10.4070/kcj.2009.39.11.488.
The Association Between Left Ventricular Hypertrophy and Biomarkers in Patients on Continuous Ambulatory Peritoneal Dialysis
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. hwgil@schca.ac.kr
- KMID: 2225652
- DOI: http://doi.org/10.4070/kcj.2009.39.11.488
Abstract
- BACKGROUND AND OBJECTIVES
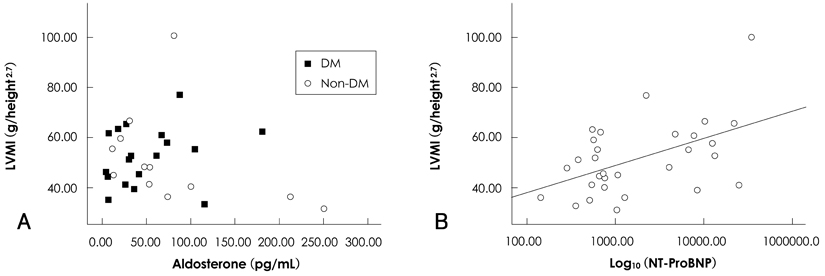
Left ventricular hypertrophy (LVH) is a major cardiovascular complication and an important predictor of mortality in patients with end stage renal disease. Some studies have shown that the serum aldosterone levels are correlated with LVH in non-diabetic patients undergoing hemodialysis. The objective of this study was to elucidate the relationships between serum biomarkers, including aldosterone, and echocardiographic findings, such as LVH, in patients on peritoneal dialysis.
SUBJECTS AND METHODS
Thirty patients on continuous ambulatory peritoneal dialysis (CAPD) for >12 months at Soonchunhyang University Cheonan Hospital were included. Transthoracic echocardiography was performed and the left ventricular mass index (LVMI) was calculated using the Devereux formula. Serum biomarkers {N-terminal pro B-type natriuretic peptide (NT-proBNP), troponin T, C-reactive protein, renin, and aldosterone} were measured.
RESULTS
Sixteen of 30 patients had LVH on the basis of the LVMI. The mean serum aldosterone level was 62.53+/-60.73 pg/mL (range, 5.03-250.68 pg/mL). LVH, on the basis of the LVMI, was not correlated with the serum aldosterone level. The serum aldosterone levels were not associated with echocardiographic findings, even with co-existing diabetes mellitus. The LVMI had a negative correlation with the hemoglobin (r=-0.405, p=0.029) and hematocrit (r=-0.374, p=0.042), and a positive correlation with NT-proBNP (r=0.560, p=0.002). The other biomarkers (renin, aldosterone, troponin T, and C-reactive protein) were not correlated with the LVMI. The LVMI was correlated with the left atrium volume index (r=0.675, p<0.001).
CONCLUSION
NT-proBNP is a good marker to predict LVH in patients undergoing CAPD. The serum aldosterone level is not correlated with LVMI, even with co-existing diabetes mellitus.
MeSH Terms
-
Aldosterone
Biomarkers
C-Reactive Protein
Diabetes Mellitus
Echocardiography
Heart Atria
Hematocrit
Hemoglobins
Humans
Hypertrophy, Left Ventricular
Kidney Failure, Chronic
Natriuretic Peptide, Brain
Peptide Fragments
Peritoneal Dialysis
Peritoneal Dialysis, Continuous Ambulatory
Renal Dialysis
Renin
Troponin T
Aldosterone
C-Reactive Protein
Hemoglobins
Natriuretic Peptide, Brain
Peptide Fragments
Renin
Troponin T
Figure
Reference
-
1. Foley RN, Parfrey PS, Harnett JD, et al. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int. 1995. 47:186–192.2. Silberberg JS, Barre PE, Prichard SS, Sniderman AD. Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int. 1989. 36:286–290.3. Wang AY, Wang M, Woo J, et al. Inflammation, residual kidney function, and cardiac hypertrophy are interrelated and combine adversely to enhance mortality and cardiovascular death risk of peritoneal dialysis patients. J Am Soc Nephrol. 2004. 15:2186–2194.4. Diris JH, Hackeng CM, Kooman JP, Pinto YM, Hermens WT, van Dieijen-Visser MP. Impaired renal clearance explains elevated troponin T fragments in hemodialysis patients. Circulation. 2004. 109:23–25.5. Deegan PB, Lafferty ME, Blumsohn A, Henderson IS, McGregor E. Prognostic value of troponin T in hemodialysis patients is in dependent of comorbidity. Kidney Int. 2001. 60:2399–2405.6. deFilippi C, Wasserman S, Rosanio S, et al. Cardiac troponin T and C-reactive protein for predicting prognosis, coronary atherosclerosis, and cardiomyopathy in patients undergoing long-term hemodialysis. JAMA. 2003. 290:353–359.7. Mallamaci F, Zoccali C, Parlongo S, et al. Diagnostic value of troponin T for alterations in left ventricular mass and function in dialysis patients. Kidney Int. 2002. 62:1884–1890.8. Wang AY, Lam CW, Yu CM, et al. N-terminal pro-brain natriuretic peptide: an independent risk predictor of cardiovascular congestion, mortality, and adverse cardiovascular outcomes in chronic peritoneal dialysis patients. J Am Soc Nephrol. 2007. 18:321–330.9. Rossi GP, Sacchetto A, Visentin P, et al. Changes in left ventricular anatomy and function in hypertension and primary aldosteronism. Hypertension. 1996. 27:1039–1045.10. Denolle T, Chatellier G, Julien J, Battaglia C, Luo P, Plouin PF. Left ventricular mass and geometry before and after etiologic treatment in renovascular hypertension, aldosterone-producing adenoma, and pheochromocytoma. Am J Hypertens. 1993. 6:907–913.11. Steigerwalt S, Zafar A, Mesiha N, Gardin J, Provenzano R. Role of aldosterone in left ventricular hypertrophy among African-American patients with end-stage renal disease on hemodialysis. Am J Nephrol. 2007. 27:159–163.12. Sato A, Funder JW, Saruta T. Involvement of aldosterone in left ventricular hypertrophy of patients with end-stage renal failure treated with hemodialysis. Am J Hypertens. 1999. 12:867–873.13. Devereux RB, de Simone G, Koren MJ, Roman MJ, Laragh JH. Left ventricular mass as a predictor of development of hypertension. Am J Hypertens. 1991. 4:603S–607S.14. Savage DD, Garrison RJ, Kannel WB, et al. The spectrum of left ventricular hypertrophy in a general population sample: the framingham study. Circulation. 1987. 75:I26–I33.15. Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991. 114:345–352.16. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006. 7:79–108.17. Delles C, Schmidt BM, Muller HJ, Oehmer S, Klingbeil AU, Schmieder RE. Functional relevance of aldosterone for the determination of left ventricular mass. Am J Cardiol. 2003. 91:297–301.18. Song JS. Studies on plasma rennin and aldosterone in essential hypertension. Korean Circ J. 1974. 4:1–24.19. Ratge D, Augustin R, Wisser H. Catecholamines, renin, aldosterone and arterial pressure in patients on chronic hemodialysis treatment. Int J Artif Organs. 1983. 6:255–260.20. Hong ZR, Gil HW, Yang JO, Lee EY, Ahn JO, Hong SY. Associations between sympathetic activity, plasma concentrations of renin, aldosterone, and parathyroid hormone, and the degree of intractability of blood pressure control in hemodialysis patients. J Korean Med Sci. 2007. 22:604–610.21. Malmqvist K, Ohman K, Lind L, Nystrom F, Kahan T. Relationships between left ventricular mass and the renin-angiotensin system, catecholamines, insulin and leptin. J Intern Med. 2002. 252:430–439.22. Suh SY, Park CG, Chwe UR, et al. Plasma renin activity and clinical implication in Korean hypertensive patients. Korean Circ J. 2005. 35:658–664.23. Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB. Relation of arterial structure and function to left ventricular geometric patterns in hypertensive adults. J Am Coll Cardiol. 1996. 28:751–756.24. London GM, Guerin AP, Marchais SJ, et al. Cardiac and arterial interactions in end-stage renal disease. Kidney Int. 1996. 50:600–608.25. Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol. 1995. 25:871–878.26. Choong CY, Herrmann HC, Weyman AE, Fifer MA. Preload dependence of doppler-derived indexes of left ventricular diastolic function in humans. J Am Coll Cardiol. 1987. 10:800–808.27. Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002. 90:1284–1289.28. Cho IJ, Pyun WB, Shin GJ. The influence of the left ventricular geometry on the left atrial size and left ventricular filling pressure in hypertensive patients, as assessed by echocardiography. Korean Circ J. 2009. 39:145–150.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Blood Pressure Control and Left Ventricular Hypertrophy in Patients on Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD)
- Peritoneal-pleural leak improved by switching from continuous ambulatory peritoneal dialysis to automated peritoneal dialysis
- Continuous Ambulatory Peritoneal Dialysis
- A clinical study of continuous ambulatory peritoneal dialysis in childhood
- Persistent Genital Swelling after Hydrocele Ligation in a Patient Receiving Continuous Ambulatory Peritoneal Dialysis