Cancer Res Treat.
2014 Jan;46(1):65-73.
Clinical Implications of Systemic Inflammatory Response Markers as Independent Prognostic Factors in Colorectal Cancer Patients
- Affiliations
-
- 1Department of Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea. cmcgslee@catholic.ac.kr
- 2Department of Biostatistics and Computing, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Cancer-related inflammation affects many aspects of malignancy. We confirm the effects of early postoperative systemic inflammation on cancer prognosis.
MATERIALS AND METHODS
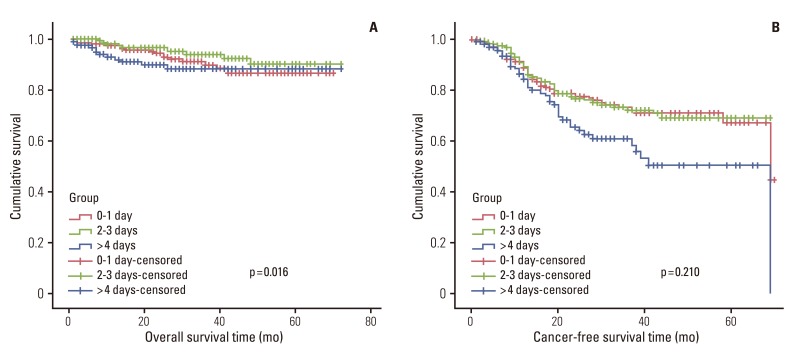
Six hundred consecutive patients underwent surgery for colorectal cancer from 2006 to 2009. Measurements of white blood cells, neutrophils, lymphocytes, monocytes, and platelet counts were performed preoperatively, daily until the fourth postoperative day, and subsequently every two days. Patients were divided into three groups based on the days spent on the leukocyte count to drop below 10,000/mm3 after surgery.
RESULTS
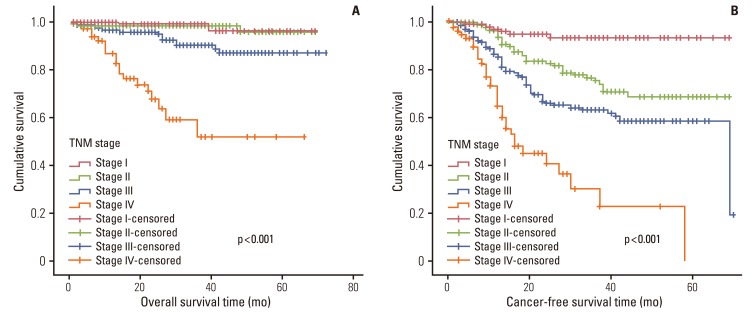
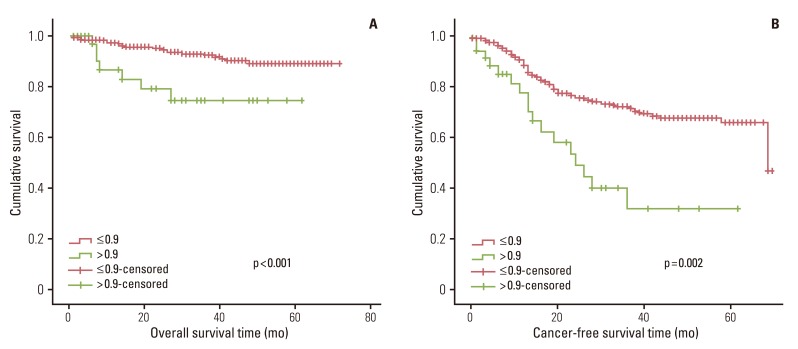
Preoperative white blood cell (WBC) counts correlated with stage of disease. In univariate survival analyses, tumor, node, metastasis (TNM) stage, and monocyte count were associated with cancer-free survival. In addition, cancer-free survival outcomes were worse in patients who required more than four days for the normalization of WBC count. A TNM stage greater than II and the neutrophil lymphocyte ratio were associated with the duration of overall survival. In a multivariate analysis of these significant variables, TNM stage, an interval longer than four days for normalization of WBC counts and monocyte count independently associated with cancer-free survival.
CONCLUSION
Postoperative early inflammatory phase and preoperative monocyte count correlate with poor colon cancer prognosis. We can conclude that preoperative and postoperative inflammatory response and period unfavorably affect the metastatic microenvironment.
MeSH Terms
Figure
Reference
-
2. Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006; 4:221–233. PMID: 16603636.
Article3. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008; 454:436–444. PMID: 18650914.
Article4. Lee IK, Vansaun MN, Shim JH, Matrisian LM, Gorden DL. Increased metastases are associated with inflammation and matrix metalloproteinase-9 activity at incision sites in a murine model of peritoneal dissemination of colorectal cancer. J Surg Res. 2013; 180:252–259. PMID: 22763216.
Article5. McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009; 12:223–226. PMID: 19318937.
Article6. Leitch EF, Chakrabarti M, Crozier JE, McKee RF, Anderson JH, Horgan PG, et al. Comparison of the prognostic value of selected markers of the systemic inflammatory response in patients with colorectal cancer. Br J Cancer. 2007; 97:1266–1270. PMID: 17923866.
Article7. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005; 91:181–184. PMID: 16118772.
Article8. Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, et al. Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009; 197:466–472. PMID: 18639229.
Article9. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC cancer staging handbook: from the AJCC cancer staging manual. New York: Springer;2002.10. Ishizuka M, Nagata H, Takagi K, Horie T, Kubota K. Inflammation-based prognostic score is a novel predictor of postoperative outcome in patients with colorectal cancer. Ann Surg. 2007; 246:1047–1051. PMID: 18043109.
Article11. Crozier JE, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC. Relationship between emergency presentation, systemic inflammatory response, and cancer-specific survival in patients undergoing potentially curative surgery for colon cancer. Am J Surg. 2009; 197:544–549. PMID: 18614139.
Article12. Okuse T, Chiba T, Katsuumi I, Imai K. Differential expression and localization of WNTs in an animal model of skin wound healing. Wound Repair Regen. 2005; 13:491–497. PMID: 16176457.
Article13. Rubin P, Constine L, Williams J. Late effects of cancer treatment. In : Perez CA, Brady LW, editors. Principles and practice of radiation oncology. Philadelphia: Lippincott-Raven;1998. p. 194–211.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Response Markers as Predictors of Colorectal Cancer Prognosis
- Prognostic implication of systemic inflammatory markers in young patients with resectable colorectal cancer
- Inflammation-based score (Glasgow prognostic score) as an independent prognostic factor in colorectal cancer patients
- Genomic Instability in Colorectal Cancer; from Bench to Bed
- TNM Staging, Molecular Staging and Prognostic Factors of Rectal Cancer