J Korean Med Sci.
2014 Apr;29(4):556-563. 10.3346/jkms.2014.29.4.556.
Effects of Transglutaminase 2 Inhibition on Ventilator-Induced Lung Injury
- Affiliations
-
- 1Department of Laboratory Medicine, College of Medicine, Kangwon National University, Chuncheon, Korea.
- 2Division of Pulmonary, Sleep and Critical Care Medicine, Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea. chepraxis@korea.ac.kr
- 3College of Nursing, Korea University, Seoul, Korea.
- 4Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea.
- 5Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea.
- KMID: 1774462
- DOI: http://doi.org/10.3346/jkms.2014.29.4.556
Abstract
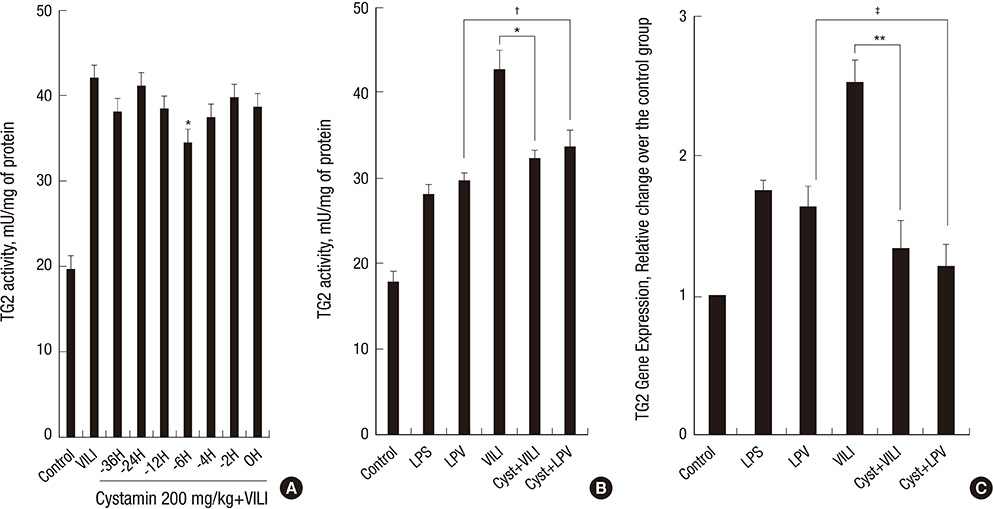
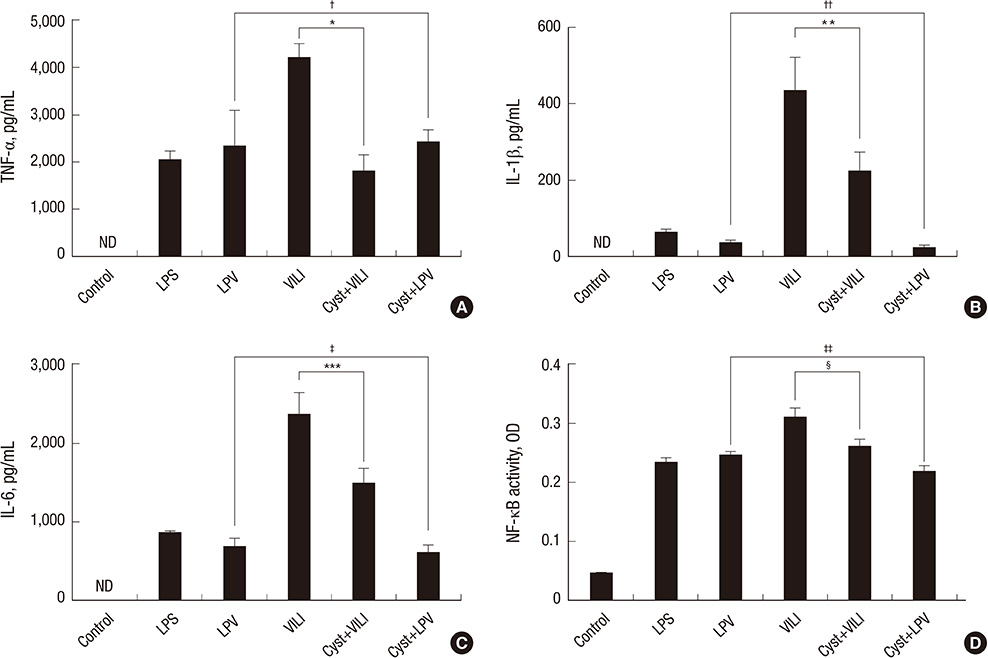
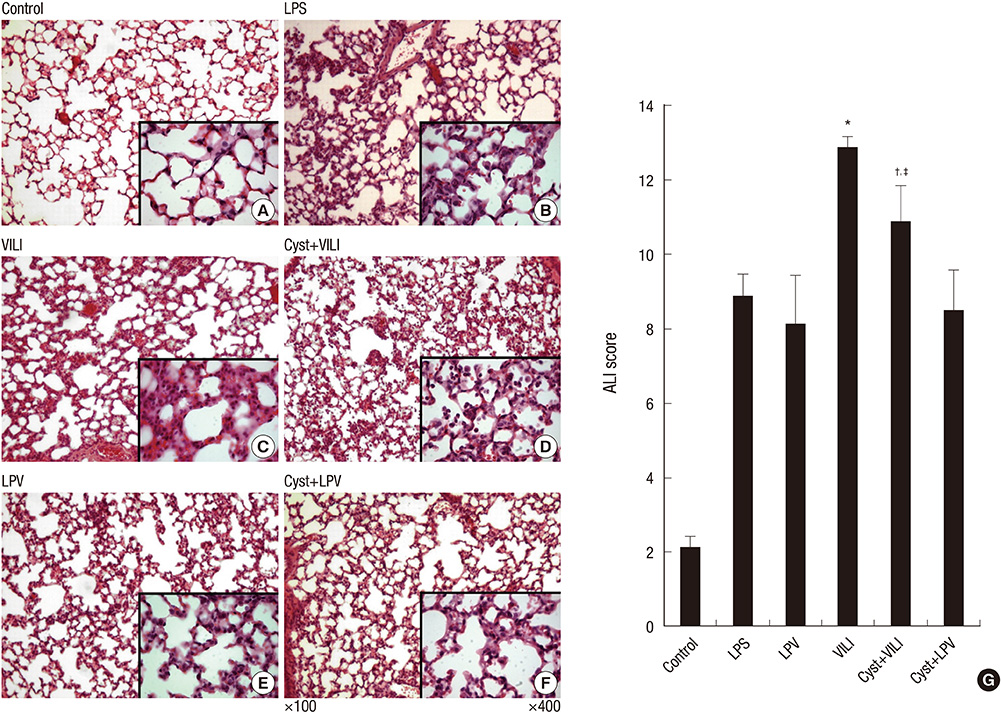
- This study was performed to examine the role of transglutaminase 2 (TG2) in ventilator-induced lung injury (VILI). C57BL/6 mice were divided into six experimental groups: 1) control group; 2) lipopolysaccharide (LPS) group; 3) lung protective ventilation (LPV) group; 4) VILI group; 5) VILI with cystamine, a TG2 inhibitor, pretreatment (Cyst+VILI) group; and 6) LPV with cystamine pretreatment (Cyst+LPV) group. Acute lung injury (ALI) score, TG2 activity and gene expression, inflammatory cytokines, and nuclear factor-kappaB (NF-kappaB) activity were measured. TG2 activity and gene expression were significantly increased in the VILI group (P < 0.05). Cystamine pretreatment significantly decreased TG2 activity and gene expression in the Cyst+VILI group (P < 0.05). Inflammatory cytokines were higher in the VILI group than in the LPS and LPV groups (P < 0.05), and significantly lower in the Cyst+VILI group than the VILI group (P < 0.05). NF-kappaB activity was increased in the VILI group compared with the LPS and LPV groups (P < 0.05), and significantly decreased in the Cyst+VILI group compared to the VILI group (P = 0.029). The ALI score of the Cyst+VILI group was lower than the VILI group, but the difference was not statistically significant (P = 0.105). These results suggest potential roles of TG2 in the pathogenesis of VILI.
Keyword
MeSH Terms
-
Acute Lung Injury/pathology
Animals
Cystamine/therapeutic use
Cytokines/analysis
Enzyme Inhibitors/therapeutic use
Enzyme-Linked Immunosorbent Assay
GTP-Binding Proteins/*antagonists & inhibitors/genetics/metabolism
Gene Expression
Lipopolysaccharides/toxicity
Male
Mice
Mice, Inbred C57BL
NF-kappa B/metabolism
Respiration, Artificial
Transglutaminases/*antagonists & inhibitors/genetics/metabolism
Ventilator-Induced Lung Injury/*enzymology/pathology/prevention & control
Cystamine
Cytokines
Enzyme Inhibitors
GTP-Binding Proteins
Lipopolysaccharides
NF-kappa B
Transglutaminases
Figure
Reference
-
1. Matthay MA, Bhattacharya S, Gaver D, Ware LB, Lim LH, Syrkina O, Eyal F, Hubmayr R. Ventilator-induced lung injury: in vivo and in vitro mechanisms. Am J Physiol Lung Cell Mol Physiol. 2002; 283:L678–L682.2. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome: the Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000; 342:1301–1308.3. Gattinoni L, Caironi P, Pelosi P, Goodman LR. What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med. 2001; 164:1701–1711.4. Beninati S, Piacentini M. The transglutaminase family: an overview: minireview article. Amino Acids. 2004; 26:367–372.5. Candi E, Schmidt R, Melino G. The cornified envelope: a model of cell death in the skin. Nat Rev Mol Cell Biol. 2005; 6:328–340.6. Fésüs L, Szondy Z. Transglutaminase 2 in the balance of cell death and survival. FEBS Lett. 2005; 579:3297–3302.7. Hitomi K. Transglutaminases in skin epidermis. Eur J Dermatol. 2005; 15:313–319.8. Folk JE, Finlayson JS. The epsilon-(gamma-glutamyl)lysine crosslink and the catalytic role of transglutaminases. Adv Protein Chem. 1977; 31:1–133.9. Kim SY, Jeitner TM, Steinert PM. Transglutaminases in disease. Neurochem Int. 2002; 40:85–103.10. Kim SY. Transglutaminase 2 in inflammation. Front Biosci. 2006; 11:3026–3035.11. Lee J, Kim YS, Choi DH, Bang MS, Han TR, Joh TH, Kim SY. Transglutaminase 2 induces nuclear factor-kappaB activation via a novel pathway in BV-2 microglia. J Biol Chem. 2004; 279:53725–53735.12. Choi CM, Jang SJ, Park SY, Choi YB, Jeong JH, Kim DS, Kim HK, Park KS, Nam BH, Kim HR, et al. Transglutaminase 2 as an independent prognostic marker for survival of patients with non-adenocarcinoma subtype of non-small cell lung cancer. Mol Cancer. 2011; 10:119.13. Oh K, Park HB, Byoun OJ, Shin DM, Jeong EM, Kim YW, Kim YS, Melino G, Kim IG, Lee DS. Epithelial transglutaminase 2 is needed for T cell interleukin-17 production and subsequent pulmonary inflammation and fibrosis in bleomycin-treated mice. J Exp Med. 2011; 208:1707–1719.14. Kim DY, Park BS, Hong GU, Lee BJ, Park JW, Kim SY, Ro JY. Anti-inflammatory effects of the R2 peptide, an inhibitor of transglutaminase 2, in a mouse model of allergic asthma, induced by ovalbumin. Br J Pharmacol. 2011; 162:210–225.15. Kim JH. The role of transglutaminase-2 in fibroproliferation after lipopolysaccharide-induced acute lung injury. Tuberc Respir Dis. 2010; 69:337–347.16. Francis RC, Vaporidi K, Bloch KD, Ichinose F, Zapol WM. Protective and detrimental effects of sodium sulfide and hydrogen sulfide in murine ventilator-induced lung injury. Anesthesiology. 2011; 115:1012–1021.17. Huang CS, Kawamura T, Lee S, Tochigi N, Shigemura N, Buchholz BM, Kloke JD, Billiar TR, Toyoda Y, Nakao A. Hydrogen inhalation ameliorates ventilator-induced lung injury. Crit Care. 2010; 14:R234.18. Takahashi K, Saha D, Shattino I, Pavlov VI, Stahl GL, Finnegan P, Melo MF. Complement 3 is involved with ventilator-induced lung injury. Int Immunopharmacol. 2011; 11:2138–2143.19. Wilson MR, O'Dea KP, Zhang D, Shearman AD, van Rooijen N, Takata M. Role of lung-marginated monocytes in an in vivo mouse model of ventilator-induced lung injury. Am J Respir Crit Care Med. 2009; 179:914–922.20. Kim JH, Suk MH, Yoon DW, Kim HY, Jung KH, Kang EH, Lee SY, Lee SY, Suh IB, Shin C, et al. Inflammatory and transcriptional roles of poly (ADP-ribose) polymerase in ventilator-induced lung injury. Crit Care. 2008; 12:R108.21. Kwon MH, Jung SH, Kim YM, Ha KS. Simultaneous activity assay of two transglutaminase isozymes, blood coagulation factor XIII and transglutaminase 2, by use of fibrinogen arrays. Anal Chem. 2011; 83:8718–8724.22. Iismaa SE, Mearns BM, Lorand L, Graham RM. Transglutaminases and disease: lessons from genetically engineered mouse models and inherited disorders. Physiol Rev. 2009; 89:991–1023.23. Verderio EA, Johnson T, Griffin M. Tissue transglutaminase in normal and abnormal wound healing: review article. Amino Acids. 2004; 26:387–404.24. George MD, Vollberg TM, Floyd EE, Stein JP, Jetten AM. Regulation of transglutaminase type II by transforming growth factor-beta 1 in normal and transformed human epidermal keratinocytes. J Biol Chem. 1990; 265:11098–11104.25. Ikura K, Shinagawa R, Suto N, Sasaki R. Increase caused by interleukin-6 in promoter activity of guinea pig liver transglutaminase gene. Biosci Biotechnol Biochem. 1994; 58:1540–1541.26. Kuncio GS, Tsyganskaya M, Zhu J, Liu SL, Nagy L, Thomazy V, Davies PJ, Zern MA. TNF-alpha modulates expression of the tissue transglutaminase gene in liver cells. Am J Physiol. 1998; 274:G240–G245.27. Suto N, Ikura K, Sasaki R. Expression induced by interleukin-6 of tissue-type transglutaminase in human hepatoblastoma HepG2 cells. J Biol Chem. 1993; 268:7469–7473.28. Suh GY, Ham HS, Lee SH, Choi JC, Koh WJ, Kim SY, Lee J, Han J, Kim HP, Choi AM, et al. A peptide with anti-transglutaminase activity decreases lipopolysaccharide-induced lung inflammation in mice. Exp Lung Res. 2006; 32:43–53.29. Mirza A, Liu SL, Frizell E, Zhu J, Maddukuri S, Martinez J, Davies P, Schwarting R, Norton P, Zern MA. A role for tissue transglutaminase in hepatic injury and fibrogenesis, and its regulation by NF-kappaB. Am J Physiol. 1997; 272:G281–G288.30. Siegel M, Khosla C. Transglutaminase 2 inhibitors and their therapeutic role in disease states. Pharmacol Ther. 2007; 115:232–245.