J Korean Med Sci.
2014 Mar;29(3):320-327. 10.3346/jkms.2014.29.3.320.
Long Term Outcomes of Pediatric Liver Transplantation According to Age
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. gsleenj@hanmail.net
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1734916
- DOI: http://doi.org/10.3346/jkms.2014.29.3.320
Abstract
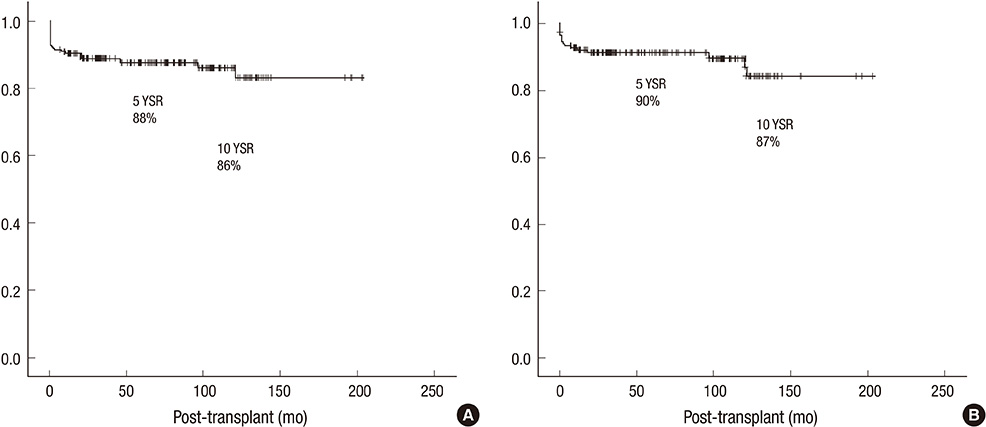
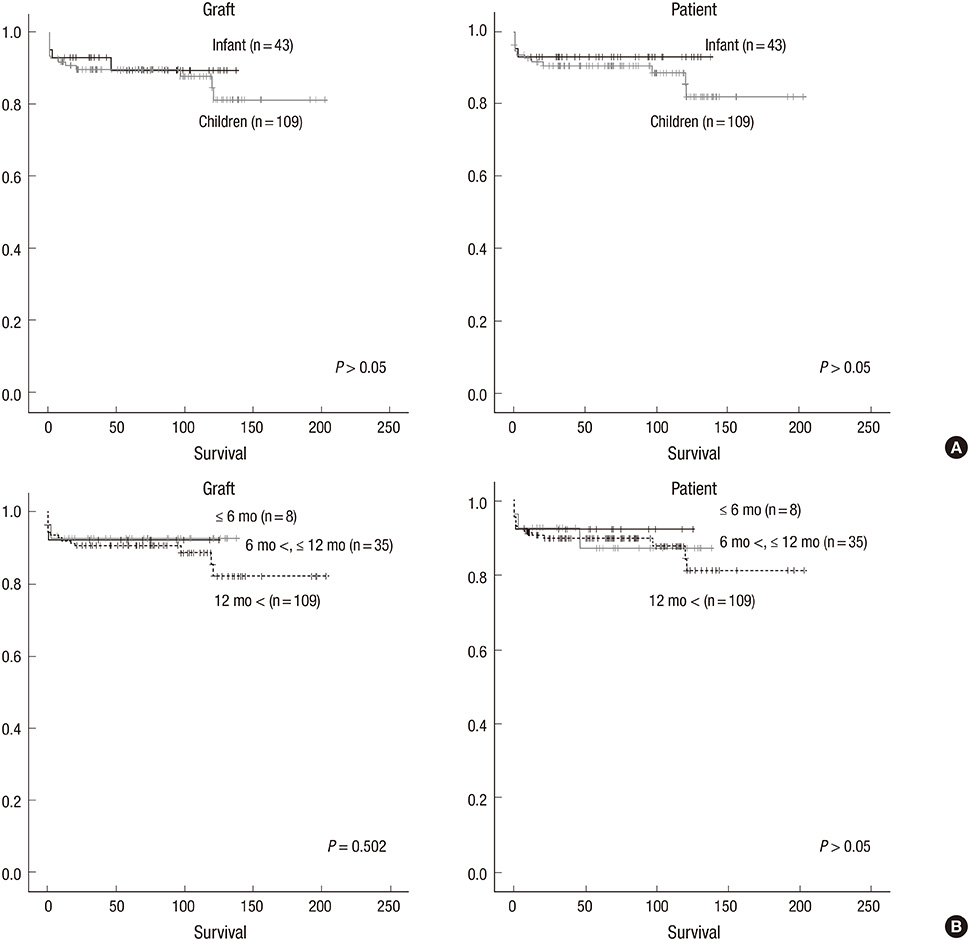
- Liver transplantation (LT) has been the key therapy for end stage liver diseases. However, LT in infancy is still understudied. From 1992 to 2010, 152 children had undergone LT in Seoul National University Hospital. Operations were performed on 43 patients aged less than 12 months (Group A) and 109 patients aged over 12 months (Group B). The mean age of the recipients was 7 months in Group A and 74 months in Group B. The patients' survival rates and post-LT complications were analyzed. The mean Pediatric End-stage Liver Disease score was higher in Group A (21.8) than in Group B (13.4) (P = 0.049). Fulminant hepatitis was less common in Group A (4.8%) than in Group B (13.8%) (P = 0.021). The post-transplant lymphoproliferative disorder and portal vein complication were more common in Group A (14.0%, 18.6%) than in Group B (1.8%, 3.7%) (P = 0.005). However, the 1, 5, and 10 yr patient survival rates were 93%, 93%, and 93%, in Group A and 92%, 90%, and 88% in Group B (P = 0.212). The survival outcome of pediatric LT is excellent and similar regardless of age. LTs in infancy are not riskier than those of children.
Keyword
MeSH Terms
-
Adolescent
Age Factors
Child
Child, Preschool
End Stage Liver Disease/mortality/*surgery
Female
Graft Rejection/epidemiology
Graft Survival
Herpesviridae Infections/etiology
Humans
Infant
Liver Transplantation/*adverse effects/*statistics & numerical data
Lymphoproliferative Disorders/*etiology
Male
Proportional Hazards Models
Risk Factors
Severity of Illness Index
Survival Rate
Treatment Outcome
Vascular Diseases/etiology
Figure
Reference
-
1. Kim ST, Kim SJ, Park KW, Suh KS, Jung SE, Ha J, Kim YH, Yun IJ, Lee KU. Early experience of liver transplantation at Seoul National University Hospital. Transplant Proc. 1996; 28:1695–1696.2. Kim JS, Grotelüschen R, Mueller T, Ganschow R, Bicak T, Wilms C, Mueller L, Helmke K, Burdelski M, Rogiers X, et al. Pediatric transplantation: the Hamburg experience. Transplantation. 2005; 79:1206–1209.3. Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, Venick RS, Feist S, Goldstein L, Saab S, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010; 252:652–661.4. Ueda M, Oike F, Ogura Y, Uryuhara K, Fujimoto Y, Kasahara M, Ogawa K, Kozaki K, Haga H, Tanaka K. Long-term outcomes of 600 living donor liver transplants for pediatric patients at a single center. Liver Transpl. 2006; 12:1326–1336.5. Jain A, Mazariegos G, Kashyap R, Kosmach-Park B, Starzl TE, Fung J, Reyes J. Pediatric liver transplantation: a single center experience spanning 20 years. Transplantation. 2002; 73:941–947.6. Oh SH, Kim KM, Kim DY, Lee YJ, Rhee KW, Jang JY, Chang SH, Lee SY, Kim JS, Choi BH, et al. Long-term outcomes of pediatric living donor liver transplantation at a single institution. Pediatr Transplant. 2010; 14:870–878.7. Korean Network for Organ Sharing. KONOS status system. accessed on 17 July 2013. Available at http://www.konos.go.kr/konosis.8. Sokal EM, Veyckemans F, de Ville de Goyet J, Moulin D, Van Hoorebeeck N, Alberti D, Buts JP, Rahier J, Van Obbergh L, Clapuyt P. Liver transplantation in children less than 1 year of age. J Pediatr. 1990; 117:205–210.9. Esquivel CO, Koneru B, Karrer F, Todo S, Iwatsuki S, Gordon RD, Makowka L, Marsh WJ Jr, Starzl TE. Liver transplantation before 1 year of age. J Pediatr. 1987; 110:545–548.10. Busuttil RW, Seu P, Millis JM, Olthoff KM, Hiatt JR, Milewicz A, Nuesse B, el-Khoury G, Raybould D, Nyerges A. Liver transplantation in children. Ann Surg. 1991; 213:48–57.11. Cox KL, Berquist WE, Castillo RO. Paediatric liver transplantation: indications, timing and medical complications. J Gastroenterol Hepatol. 1999; 14:S61–S66.12. Colombani PM, Dunn SP, Harmon WE, Magee JC, McDiarmid SV, Spray TL. Pediatric transplantation. Am J Transplant. 2003; 3:53–63.13. Cacciarelli TV, Esquivel CO, Moore DH, Cox KL, Berquist WE, Concepcion W, Hammer GB, So SK. Factors affecting survival after orthotopic liver transplantation in infants. Transplantation. 1997; 64:242–248.14. Woodle ES, Millis JM, So SK, McDiarmid SV, Busuttil RW, Esquivel CO, Whitington PF, Thistlethwaite JR. Liver transplantation in the first three months of life. Transplantation. 1998; 66:606–609.15. Noujaim HM, Mayer DA, Buckles JA, Beath SV, Kelly DA, McKiernan PJ, Mirza DF, de Ville De Goyet J. Techniques for and outcome of liver transplantation in neonates and infants weighing up to 5 kilograms. J Pediatr Surg. 2002; 37:159–164.16. Colombani PM, Cigarroa FG, Schwarz K, Wise B, Maley WE, Klein AS. Liver transplantation in infants younger than 1 year of age. Ann Surg. 1996; 223:658–662.17. Venick RS, Farmer DG, McDiarmid SV, Duffy JP, Gordon SA, Yersiz H, Hong JC, Vargas JH, Ament ME, Busuttil RW. Predictors of survival following liver transplantation in infants: a single-center analysis of more than 200 cases. Transplantation. 2010; 89:600–605.18. Chan KL, Fan ST, Saing H, Wei W, Lo CM, Ng I, Tsoi NS, Chan J, Tso WK, Yuen KY, et al. Liver transplantation is not contraindicated in infancy. Transplant Proc. 2000; 32:2142–2143.19. Van der Werf WJ, D'Alessandro AM, Knechtle SJ, Pilli G, Hoffmann RM, Judd RH, Odorico JS, Kirk AD, Rayhill SC, Sollinger HW, et al. Infant pediatric liver transplantation results equal those for older pediatric patients. J Pediatr Surg. 1998; 33:20–23.20. Deshpande RR, Bowles MJ, Vilca-Melendez H, Srinivasan P, Girlanda R, Dhawan A, Mieli-Vergani G, Muiesan P, Heaton ND, Rela M. Results of split liver transplantation in children. Ann Surg. 2002; 236:248–253.21. Wallot MA, Mathot M, Janssen M, Hölter T, Paul K, Buts JP, Reding R, Otte JB, Sokal EM. Long-term survival and late graft loss in pediatric liver transplant recipients: a 15-year single-center experience. Liver Transpl. 2002; 8:615–622.22. Horslen S, Barr ML, Christensen LL, Ettenger R, Magee JC. Pediatric transplantation in the United States, 1996-2005. Am J Transplant. 2007; 7:1339–1358.23. Magee JC, Krishnan SM, Benfield MR, Hsu DT, Shneider BL. Pediatric transplantation in the United States, 1997-2006. Am J Transplant. 2008; 8:935–945.24. McDiarmid SV, Anand R, Lindblad AS. SPLIT Research Group. Studies of Pediatric Liver Transplantation: 2002 update: an overview of demographics, indications, timing, and immunosuppressive practices in pediatric liver transplantation in the United States and Canada. Pediatr Transplant. 2004; 8:284–294.25. Fouquet V, Alves A, Branchereau S, Grabar S, Debray D, Jacquemin E, Devictor D, Durand P, Baujard C, Fabre M, et al. Long-term outcome of pediatric liver transplantation for biliary atresia: a 10-year follow-up in a single center. Liver Transpl. 2005; 11:152–160.26. Farmer DG, Venick RS, McDiarmid SV, Ghobrial RM, Gordon SA, Yersiz H, Hong J, Candell L, Cholakians A, Wozniak L, et al. Predictors of outcomes after pediatric liver transplantation: an analysis of more than 800 cases performed at a single institution. J Am Coll Surg. 2007; 204:904–914.27. Mekeel KL, Langham MR Jr, Gonzalez-Peralta RP, Hemming AW. Liver transplantation in very small infants. Pediatr Transplant. 2007; 11:66–72.28. Kasahara M, Umeshita K, Inomata Y, Uemoto S. Japanese Liver Transplantation Society. Long-term outcomes of pediatric living donor liver transplantation in Japan: an analysis of more than 2200 cases listed in the registry of the Japanese Liver Transplantation Society. Am J Transplant. 2013; 13:1830–1839.29. Kim JM, Kim KM, Yi NJ, Choe YH, Kim MS, Suh KS, Kim SI, Lee SK, Lee SG. Pediatric liver transplantation outcomes in Korea. J Korean Med Sci. 2013; 28:42–47.30. Guthery SL, Heubi JE, Bucuvalas JC, Gross TG, Ryckman FC, Alonso MH, Balistreri WF, Hornung RW. Determination of risk factors for Epstein-Barr virus-associated posttransplant lymphoproliferative disorder in pediatric liver transplant recipients using objective case ascertainment. Transplantation. 2003; 75:987–993.31. Narkewicz MR, Green M, Dunn S, Millis M, McDiarmid S, Mazariegos G, Anand R, Yin W. Studies of Pediatric Liver Transplantation Research Group. Decreasing incidence of symptomatic Epstein-Barr virus disease and posttransplant lymphoproliferative disorder in pediatric liver transplant recipients: report of the studies of pediatric liver transplantation experience. Liver Transpl. 2013; 19:730–740.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric liver transplantation in Korea: long-term outcomes and allocations
- Long Term Outcomes after Pediatric Liver Transplantation
- Issues on Long-term Management after Liver Transplantation in Children
- Pediatric Liver Transplantation
- Pediatric heart transplantation: how to manage problems affecting long-term outcomes?