J Korean Soc Transplant.
2019 Mar;33(1):1-5. 10.4285/jkstn.2019.33.1.1.
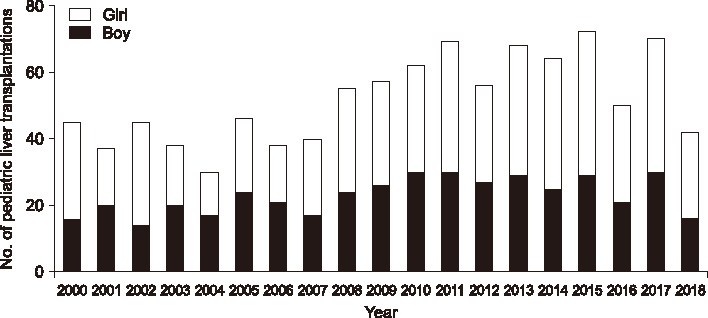
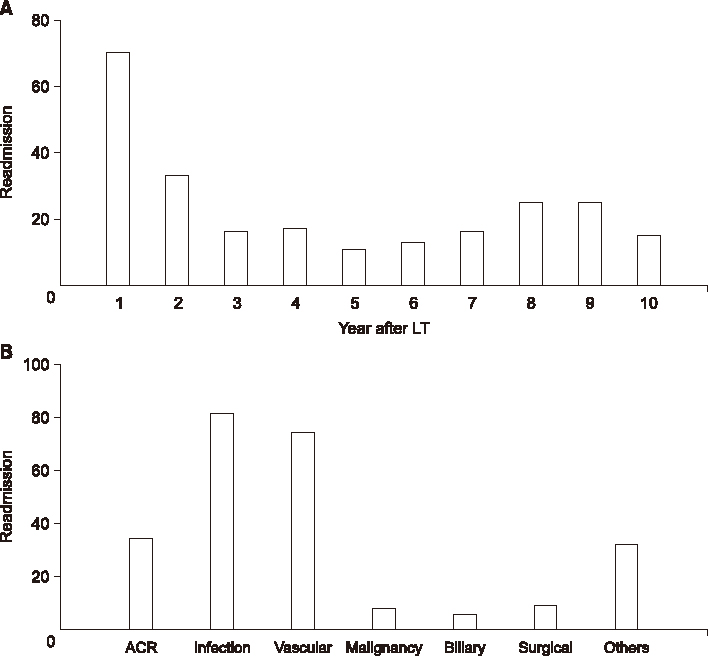
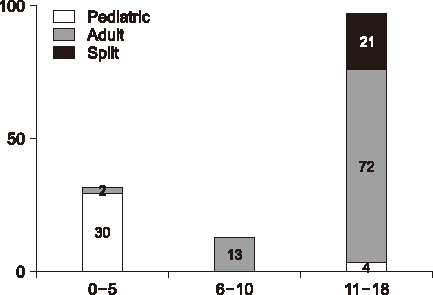
Pediatric liver transplantation in Korea: long-term outcomes and allocations
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sukkoo.lee@samsung.com
- KMID: 2442596
- DOI: http://doi.org/10.4285/jkstn.2019.33.1.1
Abstract
- Pediatric liver transplantation has evolved into an effective treatment for a variety of liver diseases in the pediatric population. Over the past 25 years, pediatric liver transplantation results in Korea have matched international standards, and Korea has become one of the most important leaders in living donor liver transplantation. This review presents the cumulative outcomes of pediatric liver transplants in Korea and highlights other concerns related to pediatric liver transplantation, particularly pediatric liver allocation policy and split liver transplantation.
Keyword
Figure
Cited by 2 articles
-
Korea-nationwide incidence of pediatric deceased donors and single-institutional status of liver transplantation using pediatric donor liver grafts
Jung-Man Namgung, Shin Hwang, Chul-Soo Ahn, Ki-Hun Kim, Deok-Bog Moon, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Dea-Yeon Kim, Kyung Mo Kim, Seak Hee Oh, Sung-Gyu Lee
Korean J Transplant. 2020;34(3):178-184. doi: 10.4285/kjt.2020.34.3.178.Whole liver deceased donor liver transplantation for pediatric recipients: single-center experience for 20 years
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh
Korean J Transplant. 2020;34(4):249-256. doi: 10.4285/kjt.20.0036.
Reference
-
1. Starzl TE, Koep LJ, Schröter GP, Halgrimson CG, Porter KA, Weil R 3rd. Liver replacement for pediatric patients. Pediatrics. 1979; 63:825–829.
Article2. Kim MJ, Choe YH. Indication of pediatric liver transplantation. J Korean Soc Transplant. 2011; 25:151–154.
Article3. Ryckman FC, Alonso MH, Bucuvalas JC, Balistreri WF. Biliary atresia: surgical management and treatment options as they relate to outcome. Liver Transpl Surg. 1998; 4:5 Suppl 1. S24–S33.4. Arnon R, Kerkar N, Davis MK, Anand R, Yin W, González-Peralta RP, et al. Liver transplantation in children with metabolic diseases: the studies of pediatric liver transplantation experience. Pediatr Transplant. 2010; 14:796–805.
Article5. Kim ST, Park YH, Lee KU, Yoon YK, Kim SW, Yang HK, et al. An experience of liver transplantation in Korea. J Korean Soc Transplant. 1988; 2:27–36.6. Busuttil RW, Klintmalm GB. General criteria for pediatric transplantation. In : Busuttil R, Klintmalm G, editors. Transplantation of the liver. 2nd ed. Philadelphia: Elsevier Saunders;2005. p. 288–291.7. Kim JM, Lee SK, Kwon CH, Joh JW, Choe YH, Park CK. Hepatocellular carcinoma in an infant with biliary atresia younger than 1 year. J Pediatr Surg. 2012; 47:819–821.
Article8. Kim JM, Kim KM, Yi NJ, Choe YH, Kim MS, Suh KS, et al. Pediatric liver transplantation outcomes in Korea. J Korean Med Sci. 2013; 28:42–47.
Article9. Lee S, Kim JM, Choi GS, Kwon CH, Choe YH, Joh JW, et al. Sustained linear growth and preserved renal function in 10-year survivors of pediatric liver transplantation. Transpl Int. 2015; 28:835–840.
Article10. Lee S, Lee SK. Pediatric liver transplantation. J Korean Assoc Pediatr Surg. 2013; 19:14–21.
Article11. Choi Y, Lee KW, Hong G, Kim H, Park MS, Suh S, et al. Status and current problems in the allocation system for pediatric liver transplantation in Korea. J Korean Soc Transplant. 2012; 26:196–201.
Article12. Korean Network for Organ Sharing (KONOS). Status of organ donation [Internet]. Seoul: KONOS;2014. cited 2019 Mar 20. Available from: https://www.konos.go.kr/konosis/index.jsp.13. United Network for Organ Sharing (UNOS). Organ distribution: allocation of livers [Internet]. Richmond, VA: UNOS;2011. cited 2019 Mar 20. Available from: https://optn.transplant.hrsa.gov.14. United Network for Organ Sharing (UNOS). Ethical principles of pediatric organ allocation [Internet]. Richmond, VA: UNOS;2011. cited 2019 Mar 20. Available from: https://optn.transplant.hrsa.gov.15. Korean Network for Organ Sharing (KONOS). Related legislature, guidelines, and regulations [Internet]. Seoul: KONOS;2014. cited 2019 Mar 20. Available from: https://www.konos.go.kr/konosis/index.jsp.