J Pathol Transl Med.
2022 Jul;56(4):173-186. 10.4132/jptm.2022.05.16.
Lymphoproliferative disorder involving body fluid: diagnostic approaches and roles of ancillary studies
- Affiliations
-
- 1Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pathology, National Cancer Center, Goyang, Korea
- 3Cancer Research Institute, Seoul National University, Seoul, Korea
- KMID: 2531609
- DOI: http://doi.org/10.4132/jptm.2022.05.16
Abstract
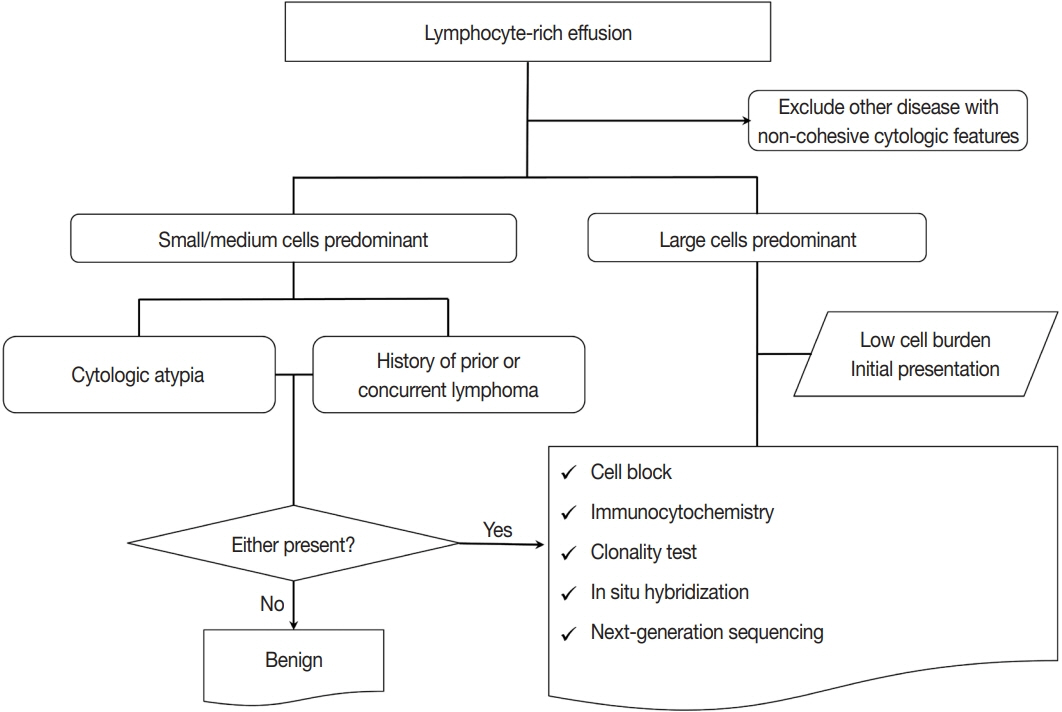
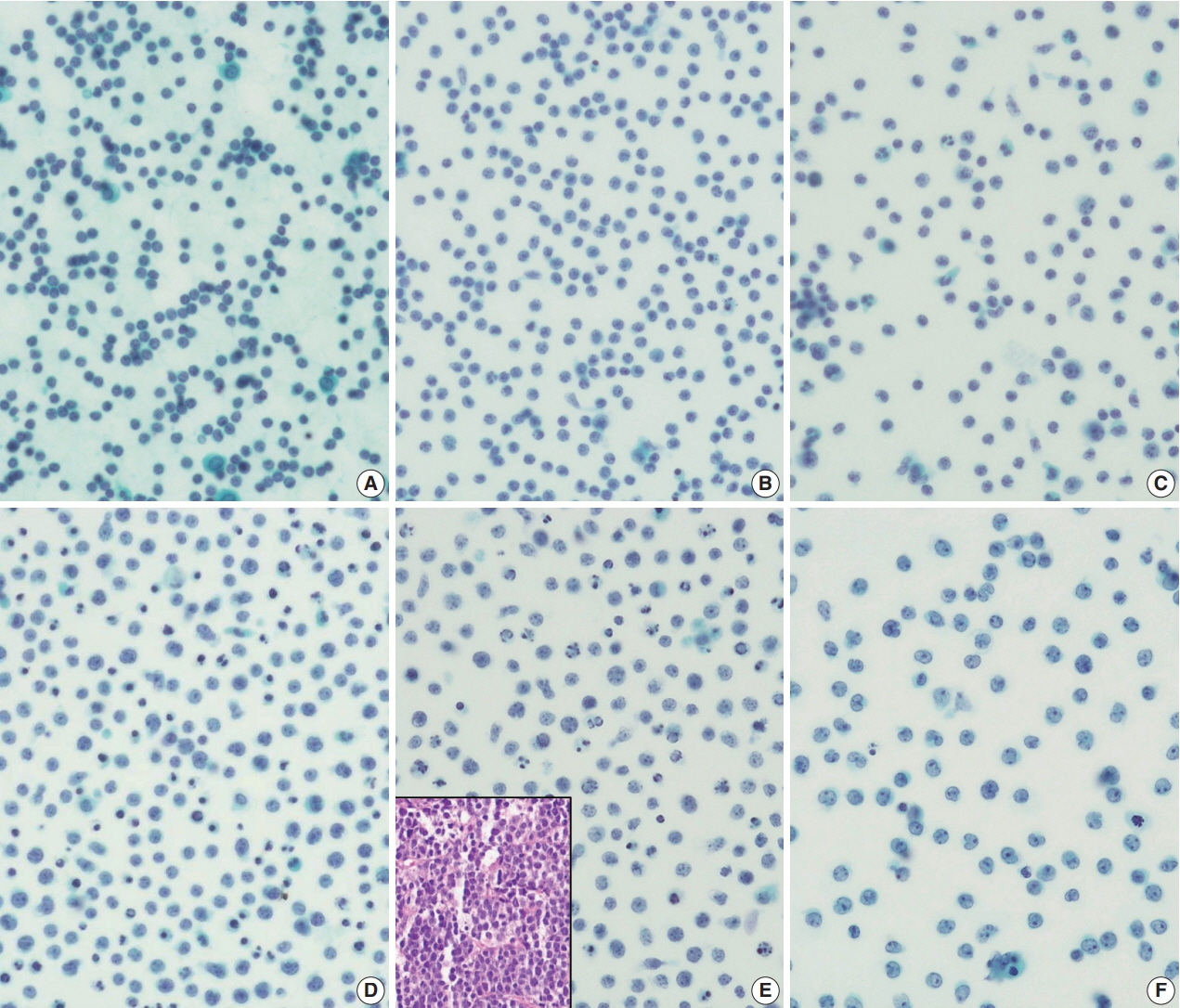
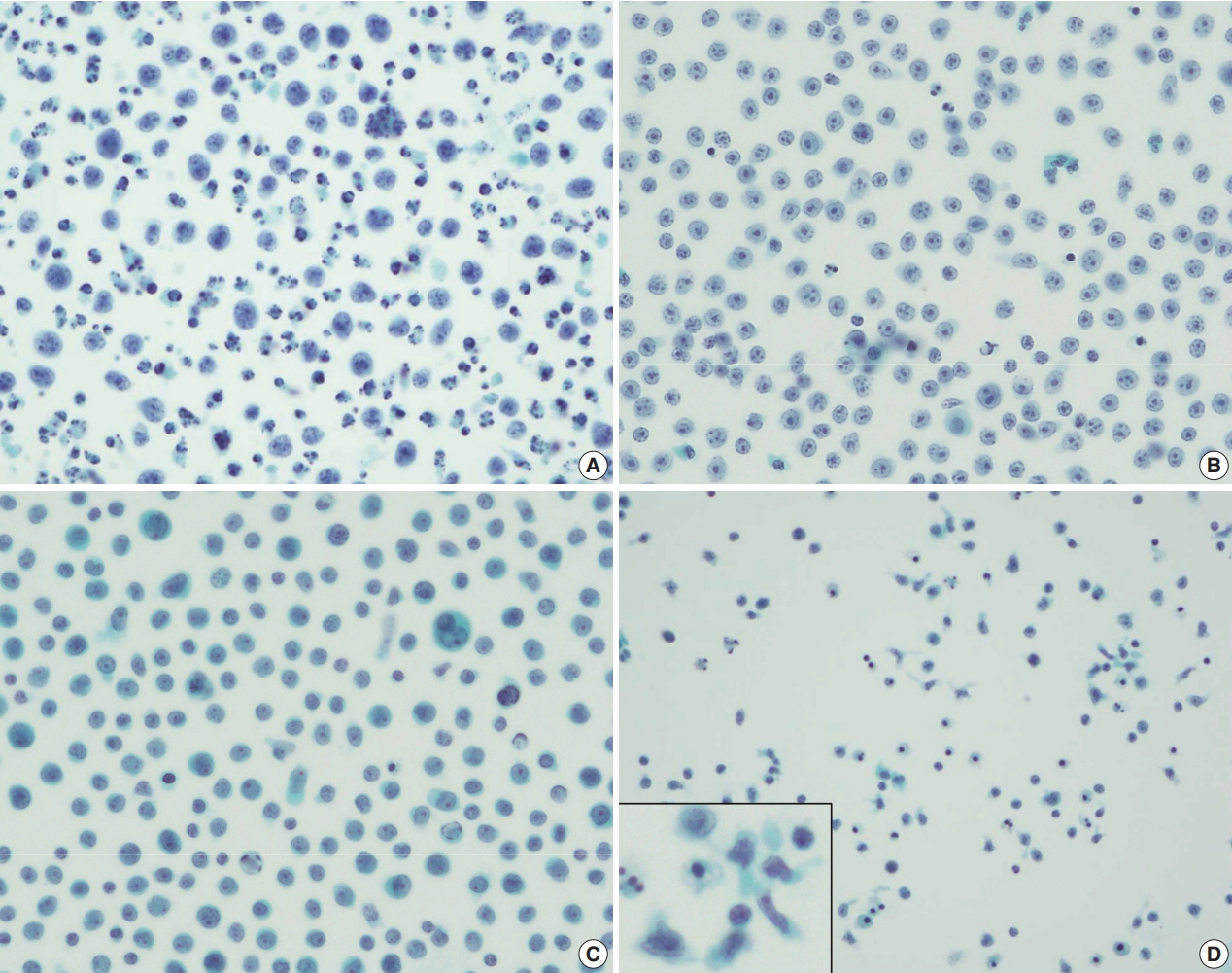
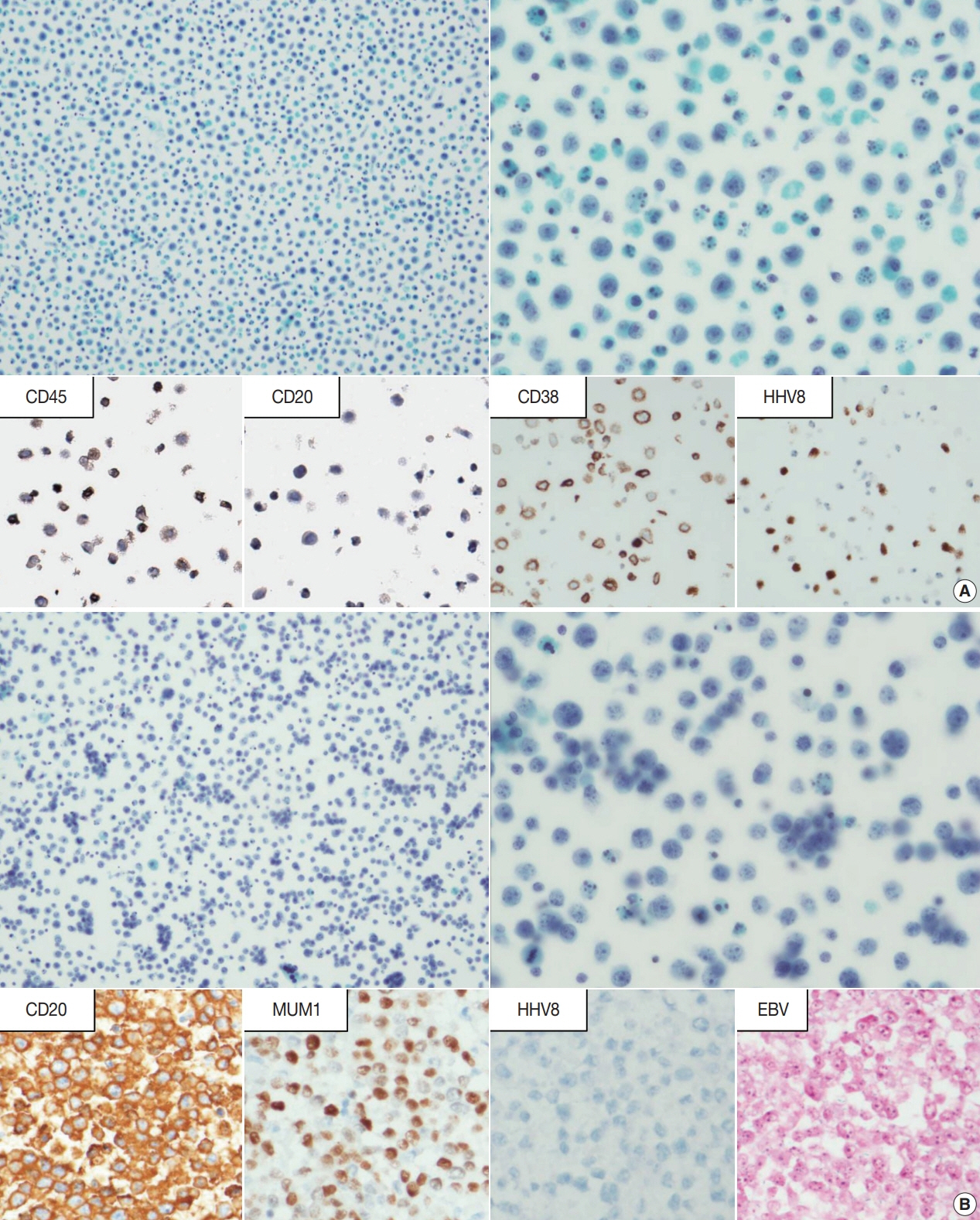
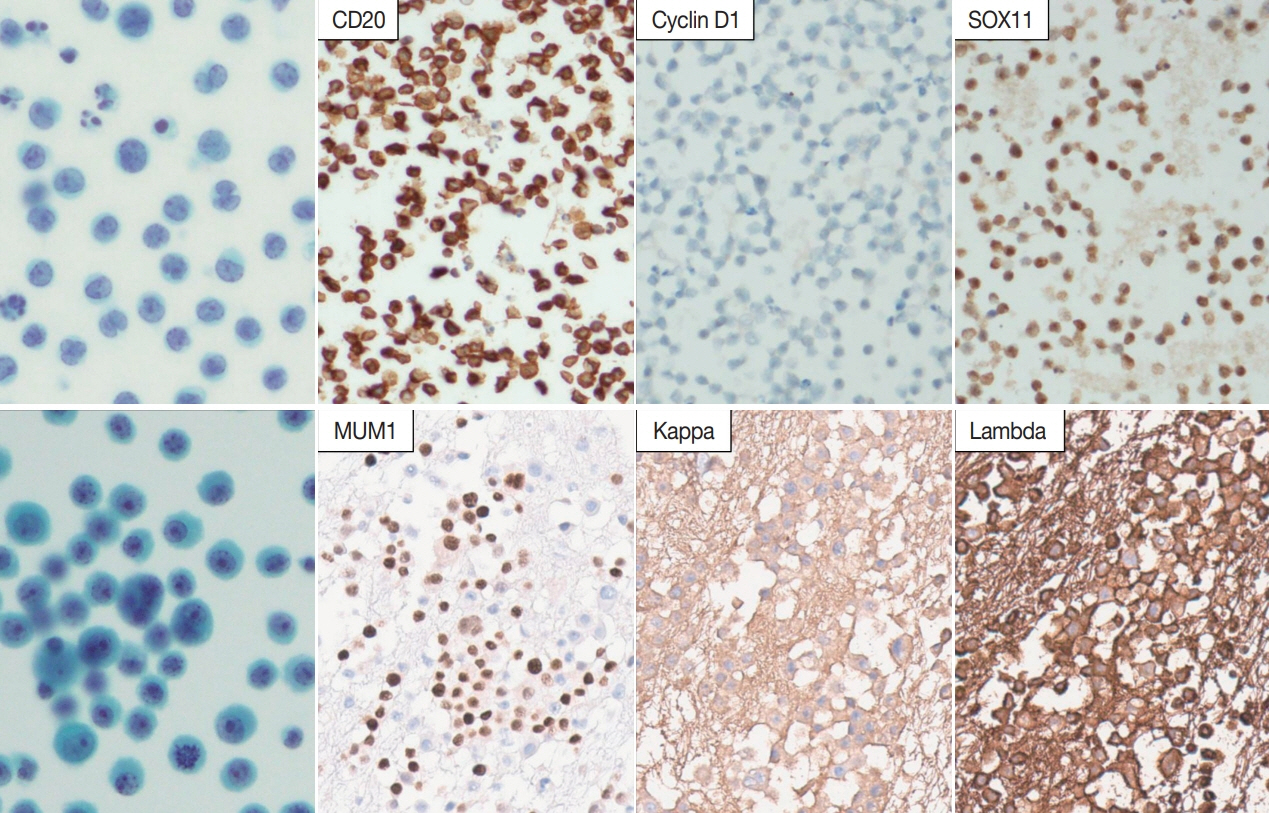
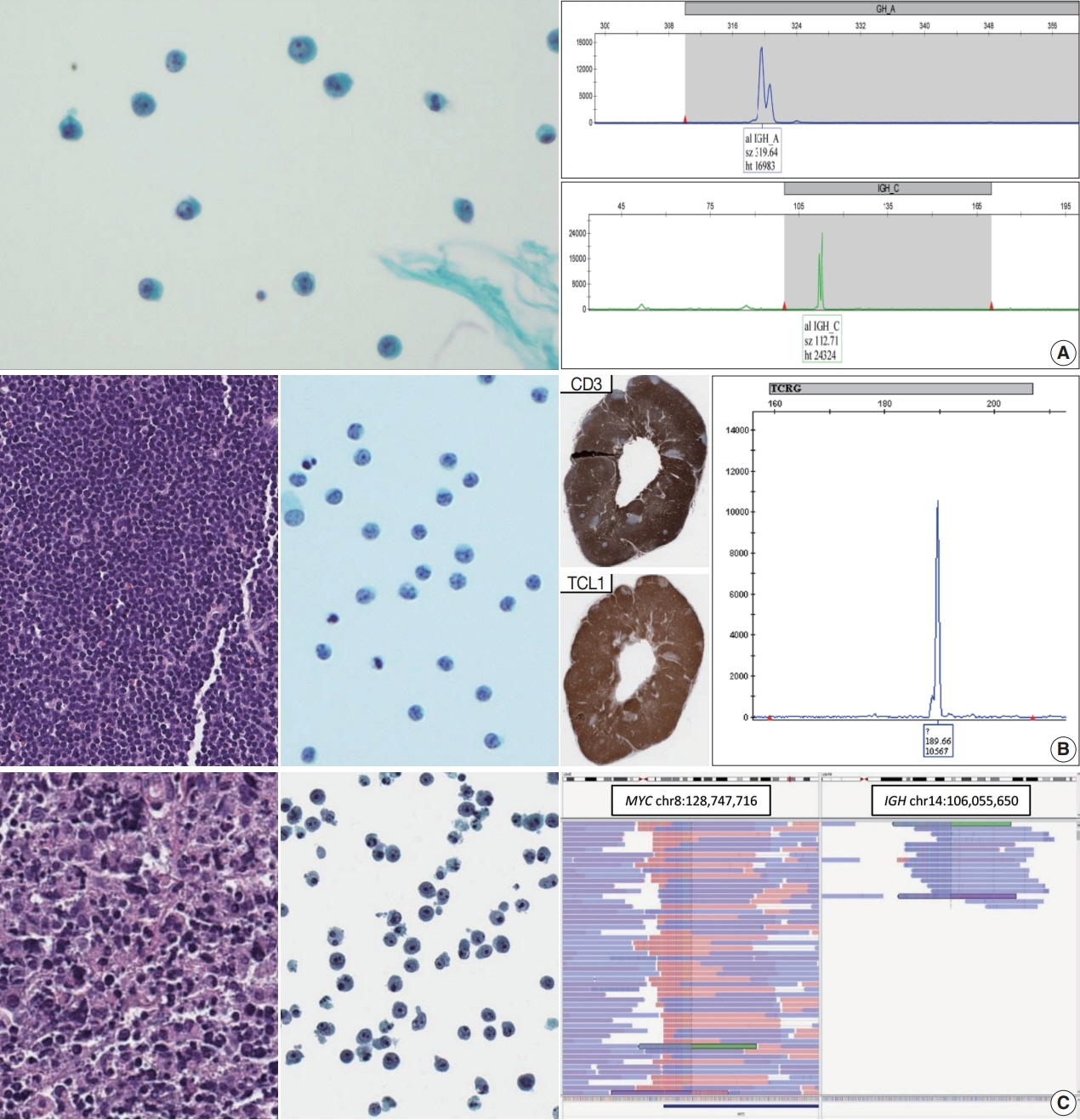
- Lymphocyte-rich effusions represent benign reactive process or neoplastic condition. Involvement of lymphoproliferative disease in body cavity is not uncommon, and it often causes diagnostic challenge. In this review, we suggest a practical diagnostic approach toward lymphocyte-rich effusions, share representative cases, and discuss the utility of ancillary tests. Cytomorphologic features favoring neoplastic condition include high cellularity, cellular atypia/pleomorphism, monomorphic cell population, and frequent apoptosis, whereas lack of atypia, polymorphic cell population, and predominance of small T cells usually represent benign reactive process. Involvement of non-hematolymphoid malignant cells in body fluid should be ruled out first, followed by categorization of the samples into either small/medium-sized cell dominant or large-sized cell dominant fluid. Small/medium-sized cell dominant effusions require ancillary tests when either cellular atypia or history/clinical suspicion of lymphoproliferative disease is present. Large-sized cell dominant effusions usually suggest neoplastic condition, however, in the settings of initial presentation or low overall cellularity, ancillary studies are helpful for more clarification. Ancillary tests including immunocytochemistry, in situ hybridization, clonality test, and next-generation sequencing can be performed using cytologic preparations. Throughout the diagnostic process, proper review of clinical history, cytomorphologic examination, and application of adequate ancillary tests are key elements for successful diagnosis.
Keyword
Figure
Reference
-
References
1. Johnston WW. The malignant pleural effusion. A review of cytopathologic diagnoses of 584 specimens from 472 consecutive patients. Cancer. 1985; 56:905–9.
Article2. Valdes L, Alvarez D, Valle JM, Pose A, San Jose E. The etiology of pleural effusions in an area with high incidence of tuberculosis. Chest. 1996; 109:158–62.
Article3. Das DK. Serous effusions in malignant lymphomas: a review. Diagn Cytopathol. 2006; 34:335–47.
Article4. Tong LC, Ko HM, Saieg MA, Boerner S, Geddie WR, da Cunha Santos G. Subclassification of lymphoproliferative disorders in serous effusions: a 10-year experience. Cancer Cytopathol. 2013; 121:261–70.5. Liu CY, Chuang SS. A simple and practical guide for triaging lymphocyte- rich effusions for ancillary studies. Adv Anat Pathol. 2021; 28:94–104.
Article6. Hunter BD, Dhakal S, Voci S, Goldstein NP, Constine LS. Pleural effusions in patients with Hodgkin lymphoma: clinical predictors and associations with outcome. Leuk Lymphoma. 2014; 55:1822–6.
Article7. Chen YP, Huang HY, Lin KP, Medeiros LJ, Chen TY, Chang KC. Malignant effusions correlate with poorer prognosis in patients with diffuse large B-cell lymphoma. Am J Clin Pathol. 2015; 143:707–15.
Article8. Yanamandra U, Deo P, Sahu KK, et al. Clinicopathological profile of myelomatous pleural effusion: single-center real-world experience and review of literature. Clin Lymphoma Myeloma Leuk. 2019; 19:183–9.
Article9. Weick JK, Kiely JM, Harrison EG Jr, Carr DT, Scanlon PW. Pleural effusion in lymphoma. Cancer. 1973; 31:848–53.
Article10. Alexandrakis MG, Passam FH, Kyriakou DS, Bouros D. Pleural effusions in hematologic malignancies. Chest. 2004; 125:1546–55.
Article11. Wang RC, Chen YH, Chen BJ, Chuang SS. The cytopathological spectrum of lymphomas in effusions in a tertiary center in Taiwan. Diagn Cytopathol. 2021; 49:232–40.
Article12. Chen L, Zhang JS, Liu DG, Cui D, Meng ZL. An algorithmic approach to diagnose haematolymphoid neoplasms in effusion by combining morphology, immunohistochemistry and molecular cytogenetics. Cytopathology. 2018; 29:10–21.
Article13. Gochhait D, Balakrishnan K, Venkatesan D, et al. The cytological evaluation of ascitic fluid led to the diagnosis of mediastinal T-lymphoblastic lymphoma: a simplified algorithmic approach to diagnosis of lymphoid cell-rich effusion. Cytopathology. 2020; 31:359–61.
Article14. Menet E, Becette V, Briffod M. Cytologic diagnosis of lobular carcinoma of the breast: experience with 555 patients in the Rene Huguenin Cancer Center. Cancer. 2008; 114:111–7.
Article15. Domagala-Kulawik J, Gornicka B, Krenke R, Mich S, Chazan R. The value of cytological diagnosis of small cell lung carcinoma. Pneumonol Alergol Pol. 2010; 78:203–10.16. Wang J, Katz RL, Stewart J, Landon G, Guo M, Gong Y. Fine-needle aspiration diagnosis of lymphomas with signet ring cell features: potential pitfalls and solutions. Cancer Cytopathol. 2013; 121:525–32.17. Ainechi S, Pambuccian SE, Wojcik EM, Barkan GA. Cytomorphologic features and differential diagnosis of neoplasms with small cell features in liquid-based urinary tract cytologic specimens. J Am Soc Cytopathol. 2015; 4:295–306.
Article18. Murali R, Loughman NT, McKenzie PR, Watson GF, Thompson JF, Scolyer RA. Cytological features of melanoma in exfoliative fluid specimens. J Clin Pathol. 2009; 62:638–43.
Article19. Wong JW, Pitlik D, Abdul-Karim FW. Cytology of pleural, peritoneal and pericardial fluids in children: a 40-year summary. Acta Cytol. 1997; 41:467–73.20. Murro D, Slade JM, Gattuso P. Cytologic findings of hematologic malignancies in bronchoalveolar lavage fluid. J Am Soc Cytopathol. 2015; 4:267–75.
Article21. Kim Y, Park CJ, Roh J, Huh J. Current concepts in primary effusion lymphoma and other effusion-based lymphomas. Korean J Pathol. 2014; 48:81–90.
Article22. Jung HR, Huh J, Ko YH, et al. Classification of malignant lymphoma subtypes in Korean patients: a report of the 4th nationwide study. J Hematopathol. 2019; 12:173–81.
Article23. Chen BJ, Wang RC, Ho CH, et al. Primary effusion lymphoma in Taiwan shows two distinctive clinicopathological subtypes with rare human immunodeficiency virus association. Histopathology. 2018; 72:930–44.
Article24. Kim M, An J, Yoon SO, et al. Human herpesvirus 8-negative effusion- based lymphoma with indolent clinical behavior in an elderly patient: a case report and literature review. Oncol Lett. 2020; 20:343.25. Alexanian S, Said J, Lones M, Pullarkat ST. KSHV/HHV8-negative effusion-based lymphoma, a distinct entity associated with fluid overload states. Am J Surg Pathol. 2013; 37:241–9.
Article26. Paydas S. Dasatinib, large granular lymphocytosis, and pleural effusion: useful or adverse effect? Crit Rev Oncol Hematol. 2014; 89:242–7.
Article27. Cortes JE, Jimenez CA, Mauro MJ, Geyer A, Pinilla-Ibarz J, Smith BD. Pleural effusion in dasatinib-treated patients with chronic myeloid leukemia in chronic phase: identification and management. Clin Lymphoma Myeloma Leuk. 2017; 17:78–82.
Article28. Brixey AG, Light RW. Pleural effusions due to dasatinib. Curr Opin Pulm Med. 2010; 16:351–6.
Article29. Quesada AE, Medeiros LJ, Clemens MW, Ferrufino-Schmidt MC, Pina-Oviedo S, Miranda RN. Breast implant-associated anaplastic large cell lymphoma: a review. Mod Pathol. 2019; 32:166–88.
Article30. Leberfinger AN, Behar BJ, Williams NC, et al. Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMA Surg. 2017; 152:1161–8.
Article31. Chai SM, Kavangh S, Ooi SS, et al. Anaplastic large-cell lymphoma associated with breast implants: a unique entity within the spectrum of peri-implant effusions. Diagn Cytopathol. 2014; 42:929–38.
Article32. Granados R, Lumbreras EM, Delgado M, Aramburu JA, Tardio JC. Cytological diagnosis of bilateral breast implant-associated lymphoma of the ALK-negative anaplastic large-cell type: clinical implications of peri-implant breast seroma cytological reporting. Diagn Cytopathol. 2016; 44:623–7.
Article33. Barbe E, de Boer M, de Jong D. A practical cytological approach to the diagnosis of breast-implant associated anaplastic large cell lymphoma. Cytopathology. 2019; 30:363–9.
Article34. Gabriel C, Achten R, Drijkoningen M. Use of liquid-based cytology in serous fluids: a comparison with conventional cytopreparatory techniques. Acta Cytol. 2004; 48:825–35.35. Fetsch PA, Simsir A, Brosky K, Abati A. Comparison of three commonly used cytologic preparations in effusion immunocytochemistry. Diagn Cytopathol. 2002; 26:61–6.
Article36. Ylagan LR, Zhai J. The value of ThinPrep and cytospin preparation in pleural effusion cytological diagnosis of mesothelioma and adenocarcinoma. Diagn Cytopathol. 2005; 32:137–44.
Article37. Lee YM, Hwang JY, Son SM, et al. Comparison of diagnostic accuracy between CellprepPlus(R) and ThinPrep(R) liquid-based preparations in effusion cytology. Diagn Cytopathol. 2014; 42:384–90.38. Hoda RS. Non-gynecologic cytology on liquid-based preparations: a morphologic review of facts and artifacts. Diagn Cytopathol. 2007; 35:621–34.
Article39. Jain D, Mathur SR, Iyer VK. Cell blocks in cytopathology: a review of preparative methods, utility in diagnosis and role in ancillary studies. Cytopathology. 2014; 25:356–71.
Article40. Nambirajan A, Jain D. Cell blocks in cytopathology: an update. Cytopathology. 2018; 29:505–24.
Article41. Gupta P, Pandey T, Gautam U, et al. Lymphoreticular malignancies in serous effusions: cytomorphologic, flow cytometric and immunocytochemical analysis. Diagn Cytopathol. 2021; 49:647–56.
Article42. Zheng Y, Wan X, Gui X, et al. Value of multi-parameter flow cytometry immunophenotyping in T/NK-cell neoplasms in cytology specimens: a retrospective study in Chinese patients. Pathol Res Pract. 2020; 216:152921.
Article43. Kaur K, Patel T, Patra S, Trivedi P. Cytomorphology, Immunophenotype, and cytogenetic profile of leukemic serous effusions. Diagn Cytopathol. 2021; 49:948–58.
Article44. Bhardwaj N, Gupta N, Gupta P, Malhotra P. Flow cytometric immunophenotyping in a liquid-based cytology sample of pleural fluid: connecting the dots. Cytopathology. 2022; 33:269–72.
Article45. Jeon YK, Yoon SO, Paik JH, et al. Molecular testing of lymphoproliferative disorders: current status and perspectives. J Pathol Transl Med. 2017; 51:224–41.
Article46. van Dongen JJ, Langerak AW, Bruggemann M, et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia. 2003; 17:2257–317.
Article47. Alkan S, Lehman C, Sarago C, Sidawy MK, Karcher DS, Garrett CT. Polymerase chain reaction detection of immunoglobulin gene rearrangement and bcl-2 translocation in archival glass slides of cytologic material. Diagn Mol Pathol. 1995; 4:25–31.
Article48. Mihaescu A, Gebhard S, Chaubert P, et al. Application of molecular genetics to the diagnosis of lymphoid-rich effusions: study of 95 cases with concomitant immunophenotyping. Diagn Cytopathol. 2002; 27:90–5.
Article49. Li J, Zhang W, Wang W, et al. Forty-nine cases of acute lymphoblastic leukaemia/lymphoma in pleural and pericardial effusions: a cytological- histological correlation. Cytopathology. 2018; 29:172–8.
Article50. Murphy M, Signoretti S, Nasser I, Sherburne B, Loda M. Detection of concurrent/recurrent non-Hodgkin’s lymphoma in effusions by PCR. Hum Pathol. 1999; 30:1361–6.
Article51. Pinto D, Schmitt F. Current applications of molecular testing on body cavity fluids. Diagn Cytopathol. 2020; 48:840–51.
Article52. Bode-Lesniewska B. Flow cytometry and effusions in lymphoproliferative processes and other hematologic neoplasias. Acta Cytol. 2016; 60:354–64.
Article53. Chen X, Cherian S. Immunophenotypic characterization of T-cell prolymphocytic leukemia. Am J Clin Pathol. 2013; 140:727–35.
Article54. Garady C, Saieg MA, Ko HM, Geddie WR, Boerner SL, da Cunha Santos G. Epstein-Barr virus encoded RNA detected by in situ hybridization using cytological preparations. Cytopathology. 2014; 25:101–7.
Article55. Minca EC, Lanigan CP, Reynolds JP, et al. ALK status testing in nonsmall- cell lung carcinoma by FISH on ThinPrep slides with cytology material. J Thorac Oncol. 2014; 9:464–8.56. Sundling KE, Cibas ES. Ancillary studies in pleural, pericardial, and peritoneal effusion cytology. Cancer Cytopathol. 2018; 126 Suppl 8:590–8.
Article57. Walts AE, Hiroshima K, McGregor SM, Wu D, Husain AN, Marchevsky AM. BAP1 immunostain and CDKN2A (p16) FISH analysis: clinical applicability for the diagnosis of malignant mesothelioma in effusions. Diagn Cytopathol. 2016; 44:599–606.58. Wang W, Tang Y, Li J, Jiang L, Jiang Y, Su X. Detection of ALK rearrangements in malignant pleural effusion cell blocks from patients with advanced non-small cell lung cancer: a comparison of Ventana immunohistochemistry and fluorescence in situ hybridization. Cancer Cytopathol. 2015; 123:117–22.59. Chen Z, Wang DD, Peier A, Stone JF, Sandberg AA. FISH in the evaluation of pleural and ascitic fluids. Cancer Genet Cytogenet. 1995; 84:116–9.
Article60. Savic S, Franco N, Grilli B, et al. Fluorescence in situ hybridization in the definitive diagnosis of malignant mesothelioma in effusion cytology. Chest. 2010; 138:137–44.
Article61. Matsumoto S, Nabeshima K, Kamei T, et al. Morphology of 9p21 homozygous deletion-positive pleural mesothelioma cells analyzed using fluorescence in situ hybridization and virtual microscope system in effusion cytology. Cancer Cytopathol. 2013; 121:415–22.
Article62. Betz BL, Dixon CA, Weigelin HC, Knoepp SM, Roh MH. The use of stained cytologic direct smears for ALK gene rearrangement analysis of lung adenocarcinoma. Cancer Cytopathol. 2013; 121:489–99.63. Tsai TH, Wu SG, Hsieh MS, Yu CJ, Yang JC, Shih JY. Clinical and prognostic implications of RET rearrangements in metastatic lung adenocarcinoma patients with malignant pleural effusion. Lung Cancer. 2015; 88:208–14.
Article64. Jardin F, Jais JP, Molina TJ, et al. Diffuse large B-cell lymphomas with CDKN2A deletion have a distinct gene expression signature and a poor prognosis under R-CHOP treatment: a GELA study. Blood. 2010; 116:1092–104.
Article65. Cai G, Wong R, Chhieng D, et al. Identification of EGFR mutation, KRAS mutation, and ALK gene rearrangement in cytological specimens of primary and metastatic lung adenocarcinoma. Cancer Cytopathol. 2013; 121:500–7.66. Lozano MD, Zulueta JJ, Echeveste JI, et al. Assessment of epidermal growth factor receptor and K-ras mutation status in cytological stained smears of non-small cell lung cancer patients: correlation with clinical outcomes. Oncologist. 2011; 16:877–85.
Article67. Bellevicine C, Malapelle U, Vigliar E, de Luca C, Troncone G. Epidermal growth factor receptor test performed on liquid-based cytology lung samples: experience of an academic referral center. Acta Cytol. 2014; 58:589–94.
Article68. Scarpa A, Sikora K, Fassan M, et al. Molecular typing of lung adenocarcinoma on cytological samples using a multigene next generation sequencing panel. PLoS One. 2013; 8:e80478.
Article69. Gailey MP, Stence AA, Jensen CS, Ma D. Multiplatform comparison of molecular oncology tests performed on cytology specimens and formalin-fixed, paraffin-embedded tissue. Cancer Cytopathol. 2015; 123:30–9.
Article70. Lindeman NI, Cagle PT, Aisner DL, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. Arch Pathol Lab Med. 2018; 142:321–46.
Article71. Moffitt AB, Dave SS. Clinical Applications of the genomic landscape of aggressive non-Hodgkin lymphoma. J Clin Oncol. 2017; 35:955–62.
Article72. Pan ST, Wang RC, Kuo CC, Hsieh YC, Su YZ, Chuang SS. MYD88 L265P mutation analysis is a useful diagnostic adjunct for lymphoplasmacytic lymphoma with pleural effusion. Pathol Int. 2019; 69:601–7.
Article73. Varettoni M, Arcaini L, Zibellini S, et al. Prevalence and clinical significance of the MYD88 (L265P) somatic mutation in Waldenstrom’s macroglobulinemia and related lymphoid neoplasms. Blood. 2013; 121:2522–8.74. Hiemcke-Jiwa LS, Ten Dam-van Loon NH, Leguit RJ, et al. Potential diagnosis of vitreoretinal lymphoma by detection of MYD88 mutation in aqueous humor with ultrasensitive droplet digital polymerase chain reaction. JAMA Ophthalmol. 2018; 136:1098–104.
Article75. Bonzheim I, Giese S, Deuter C, et al. High frequency of MYD88 mutations in vitreoretinal B-cell lymphoma: a valuable tool to improve diagnostic yield of vitreous aspirates. Blood. 2015; 126:76–9.
Article76. Tanaka R, Kaburaki T, Taoka K, et al. More accurate diagnosis of vitreoretinal lymphoma using a combination of diagnostic test results: a prospective observational study. Ocul Immunol Inflamm. 2021; Apr. 1. [Epub]. https://doi.org/10.1080/09273948.2021.1873394.
Article77. Roy-Chowdhuri S, Goswami RS, Chen H, et al. Factors affecting the success of next-generation sequencing in cytology specimens. Cancer Cytopathol. 2015; 123:659–68.
Article78. Roy-Chowdhuri S, Chen H, Singh RR, et al. Concurrent fine needle aspirations and core needle biopsies: a comparative study of substrates for next-generation sequencing in solid organ malignancies. Mod Pathol. 2017; 30:499–508.
Article79. Williams C, Ponten F, Moberg C, et al. A high frequency of sequence alterations is due to formalin fixation of archival specimens. Am J Pathol. 1999; 155:1467–71.
Article80. Srinivasan M, Sedmak D, Jewell S. Effect of fixatives and tissue processing on the content and integrity of nucleic acids. Am J Pathol. 2002; 161:1961–71.
Article81. Bellevicine C, Malapelle U, Vigliar E, Pisapia P, Vita G, Troncone G. How to prepare cytological samples for molecular testing. J Clin Pathol. 2017; 70:819–26.
Article82. Navrkalova V, Plevova K, Hynst J, et al. LYmphoid NeXt-Generation Sequencing (LYNX) panel: a comprehensive capture-based sequencing tool for the analysis of prognostic and predictive markers in lymphoid malignancies. J Mol Diagn. 2021; 23:959–74.83. Bastos-Oreiro M, Suarez-Gonzalez J, Andres-Zayas C, et al. Incorporation of next-generation sequencing in clinical practice using solid and liquid biopsy for patients with non-Hodgkin’s lymphoma. Sci Rep. 2021; 11:22815.
Article84. Allahyar A, Pieterse M, Swennenhuis J, et al. Robust detection of translocations in lymphoma FFPE samples using targeted locus capture-based sequencing. Nat Commun. 2021; 12:3361.
Article85. Pillonel V, Juskevicius D, Bihl M, et al. Routine next generation sequencing of lymphoid malignancies: clinical utility and challenges from a 3-year practical experience. Leuk Lymphoma. 2020; 61:2568–83.
Article86. Tan B, Martin B, Fernandez-Pol S. Angioimmunoblastic T-cell lymphoma diagnosed from pleural fluid by integration of morphologic, immunophenotypic, and molecular findings. Diagn Cytopathol. 2021; 49:E462–6.
Article87. Martini M, Capodimonti S, Cenci T, et al. To obtain more with less: cytologic samples with ancillary molecular techniques: the useful role of liquid-based cytology. Arch Pathol Lab Med. 2018; 142:299–307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Post-Transplant Lymphoproliferative Disorder Occurring after Renal Transplantation: A Case Report
- Posttransplantation lymphoproliferative disorder involving liver after renal transplantation
- Post-transplantation Lymphoproliferative Disorder in Transplanted Liver: A Case Report
- The Cytopathology of Body Cavity Fluid
- A Case of Primary Cutaneous CD4-positive Small/Medium T-cell Lymphoproliferative Disorder