Korean J Neurotrauma.
2019 Oct;15(2):150-158. 10.13004/kjnt.2019.15.e36.
Importance of Hemoglobin A1c Levels for the Detection of Post-Surgical Infection Following Single-Level Lumbar Posterior Fusion in Patients with Diabetes
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. md6576@naver.com
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2461120
- DOI: http://doi.org/10.13004/kjnt.2019.15.e36
Abstract
OBJECTIVE
Several studies have reported that patients with diabetes mellitus (DM) are vulnerable to infection. However, the mechanism underlying this remains unclear. We hypothesized that preoperative blood glucose levels in patients with DM may be a risk factor for surgical site infection (SSI). We aimed to investigate the relationship between hemoglobin A1c (HbA1c) level and SSI incidence following single-level spinal fusion surgery.
METHODS
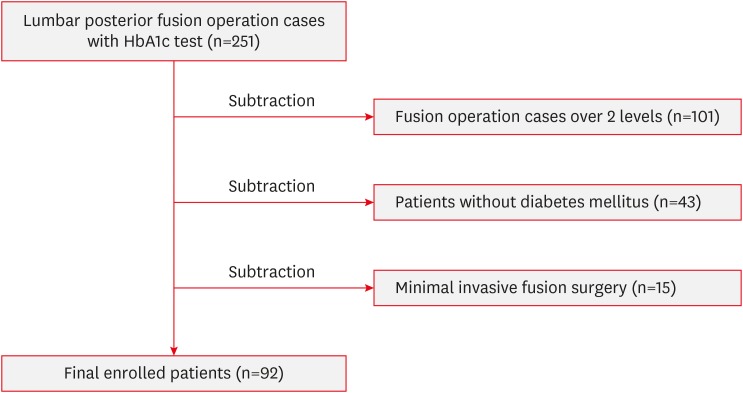
Patients with DM who underwent single-level lumbar posterior fusion surgery were retrospectively reviewed. Ninety-two patients were included and classified into the SSI and SSI-free groups. Clinical data with demographic findings were obtained and compared. The HbA1c cut-off value was defined using receiver operating characteristic (ROC) and area under the curve (AUC) analyses, which showed a significantly increased SSI risk. Potential variables were verified using multiple logistic regression analysis.
RESULTS
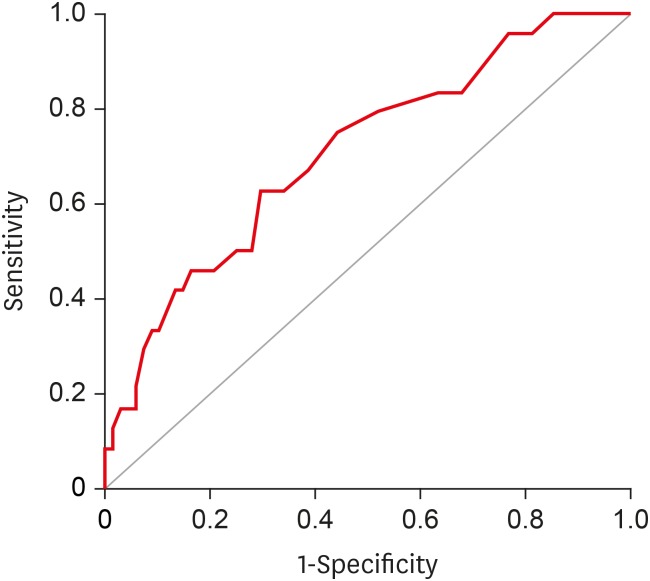
Among the enrolled patients, 24 had SSI and 68 did not within 1 year. The preoperative HbA1c level was higher in patients with SSI (6.8%) than in the non-infected patients (6.0%; p=0.008). ROC analysis showed that if the HbA1c level is higher than 6.9%, the risk of SSI significantly increases (p=0.003; AUC, 0.708; sensitivity, 62.5%; specificity, 70.6%). The preoperative HbA1c level was significantly correlated with SSI incidence, after adjusting for potential variables (p=0.008; odds ratio, 4.500; 95% confidence interval, 1.486-13.624).
CONCLUSION
The HbA1c level, indicating glycemic control, in patients with DM may be a risk factor for SSI in single-level lumbar spine posterior fusion.
MeSH Terms
Figure
Cited by 1 articles
-
Learning Curve and Complications Experience of Oblique Lateral Interbody Fusion : A Single-Center 143 Consecutive Cases
Bu Kwang Oh, Dong Wuk Son, Su Hun Lee, Jun Seok Lee, Soon Ki Sung, Sang Weon Lee, Geun Sung Song
J Korean Neurosurg Soc. 2021;64(3):447-459. doi: 10.3340/jkns.2020.0342.
Reference
-
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016; 387:1513–1530. PMID: 27061677.2. World Health Organization. Global report on diabetes. Geneva: World Health Organization;2016.3. Browne JA, Cook C, Pietrobon R, Bethel MA, Richardson WJ. Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976). 2007; 32:2214–2219. PMID: 17873813.
Article4. Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J. 2003; 3:496–501. PMID: 14609695.
Article5. Golinvaux NS, Varthi AG, Bohl DD, Basques BA, Grauer JN. Complication rates following elective lumbar fusion in patients with diabetes: insulin dependence makes the difference. Spine (Phila Pa 1976). 2014; 39:1809–1816. PMID: 25010098.6. Guzman JZ, Iatridis JC, Skovrlj B, Cutler HS, Hecht AC, Qureshi SA, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976). 2014; 39:1596–1604. PMID: 24983935.
Article7. Hikata T, Iwanami A, Hosogane N, Watanabe K, Ishii K, Nakamura M, et al. High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J Orthop Sci. 2014; 19:223–228. PMID: 24368606.
Article8. Klemencsics I, Lazary A, Szoverfi Z, Bozsodi A, Eltes P, Varga PP. Risk factors for surgical site infection in elective routine degenerative lumbar surgeries. Spine J. 2016; 16:1377–1383. PMID: 27520077.
Article9. Koutsoumbelis S, Hughes AP, Girardi FP, Cammisa FP Jr, Finerty EA, Nguyen JT, et al. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am. 2011; 93:1627–1633. PMID: 21915578.
Article10. Simpson JM, Silveri CP, Balderston RA, Simeone FA, An HS. The results of operations on the lumbar spine in patients who have diabetes mellitus. J Bone Joint Surg Am. 1993; 75:1823–1829. PMID: 8258554.
Article11. Takahashi S, Suzuki A, Toyoda H, Terai H, Dohzono S, Yamada K, et al. Characteristics of diabetes associated with poor improvements in clinical outcomes after lumbar spine surgery. Spine (Phila Pa 1976). 2013; 38:516–522. PMID: 22976346.
Article12. Chaichana KL, Bydon M, Santiago-Dieppa DR, Hwang L, McLoughlin G, Sciubba DM, et al. Risk of infection following posterior instrumented lumbar fusion for degenerative spine disease in 817 consecutive cases. J Neurosurg Spine. 2014; 20:45–52. PMID: 24206038.
Article13. Chen S, Anderson MV, Cheng WK, Wongworawat MD. Diabetes associated with increased surgical site infections in spinal arthrodesis. Clin Orthop Relat Res. 2009; 467:1670–1673. PMID: 19225851.
Article14. Schimmel JJ, Horsting PP, de Kleuver M, Wonders G, van Limbeek J. Risk factors for deep surgical site infections after spinal fusion. Eur Spine J. 2010; 19:1711–1719. PMID: 20445999.
Article15. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 32:1327–1334. 2009; PMID: 19502545.16. O'Keeffe DT, Maraka S, Rizza RA. HbA1c in the evaluation of diabetes mellitus. JAMA. 2016; 315:605–606. PMID: 26864415.17. Cancienne JM, Werner BC, Chen DQ, Hassanzadeh H, Shimer AL. Perioperative hemoglobin A1c as a predictor of deep infection following single-level lumbar decompression in patients with diabetes. Spine J. 2017; 17:1100–1105. PMID: 28343046.
Article18. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999; 20:250–278. PMID: 10219875.19. Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016; 37:88–99. PMID: 26503187.
Article20. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004; 32:470–485. PMID: 15573054.21. Adams AL, Paxton EW, Wang JQ, Johnson ES, Bayliss EA, Ferrara A, et al. Surgical outcomes of total knee replacement according to diabetes status and glycemic control, 2001 to 2009. J Bone Joint Surg Am. 2013; 95:481–487. PMID: 23446446.
Article22. Chrastil J, Anderson MB, Stevens V, Anand R, Peters CL, Pelt CE. Is Hemoglobin A1c or perioperative hyperglycemia predictive of periprosthetic joint infection or death following primary total joint arthroplasty? J Arthroplasty. 2015; 30:1197–1202. PMID: 25697889.
Article23. Han HS, Kang SB. Relations between long-term glycemic control and postoperative wound and infectious complications after total knee arthroplasty in type 2 diabetics. Clin Orthop Surg. 2013; 5:118–123. PMID: 23730475.
Article24. Hwang JS, Kim SJ, Bamne AB, Na YG, Kim TK. Do glycemic markers predict occurrence of complications after total knee arthroplasty in patients with diabetes? Clin Orthop Relat Res. 2015; 473:1726–1731. PMID: 25404402.
Article25. Maradit Kremers H, Lewallen LW, Mabry TM, Berry DJ, Berbari EF, Osmon DR. Diabetes mellitus, hyperglycemia, hemoglobin A1C and the risk of prosthetic joint infections in total hip and knee arthroplasty. J Arthroplasty. 2015; 30:439–443. PMID: 25458090.
Article26. Stryker LS, Abdel MP, Morrey ME, Morrow MM, Kor DJ, Morrey BF. Elevated postoperative blood glucose and preoperative hemoglobin A1C are associated with increased wound complications following total joint arthroplasty. J Bone Joint Surg Am. 2013; 95:808–814. S1–S2. PMID: 23636187.
Article27. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011; 34(Suppl 1):S62–S69. PMID: 21193628.28. Handelsman Y, Mechanick JI, Blonde L, Grunberger G, Bloomgarden ZT, Bray GA, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011; 17(Suppl 2):1–53.
Article29. Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE. The national glycohemoglobin standardization program: a five-year progress report. Clin Chem. 2001; 47:1985–1992. PMID: 11673367.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Performance Evaluation of the ARKRAY ADAMS A1c HA-8180
- HbA1c for Diagnosis of Type 2 Diabetes in Korea
- Relationship between Glycemic Control and Diabetic Retinopathy
- Long-Term Follow-up of Posterior Pedicle Instrumentation and Anterior Lumbar Interbody Fusion using a Single Autogenous Tricortical Iliac Graft
- The Optimal Cutoff Value of Glycated Hemoglobin for Detection of Diabetic Retinopathy