Cancer Res Treat.
2019 Oct;51(4):1259-1268. 10.4143/crt.2018.652.
Subdivision of Nasopharyngeal Carcinoma Patients with Bone-Only Metastasis at Diagnosis for Prediction of Survival and Treatment Guidance
- Affiliations
-
- 1Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China. maihq@mail.sysu.edu.cn, tanglq@sysucc.org.cn
- 2Department of Nasopharyngeal Carcinoma, Sun Yat-sen University Cancer Center, Guangzhou, China.
- KMID: 2460575
- DOI: http://doi.org/10.4143/crt.2018.652
Abstract
- PURPOSE
The purpose of this study was to subdivide M1 stage nasopharyngeal carcinoma (NPC) patients with bone-only metastases for prognosis prediction while identifying the treatment effect of locoregional radiotherapy (LRRT) and metastasis radiotherapy (MRT) among patients with different risk.
MATERIALS AND METHODS
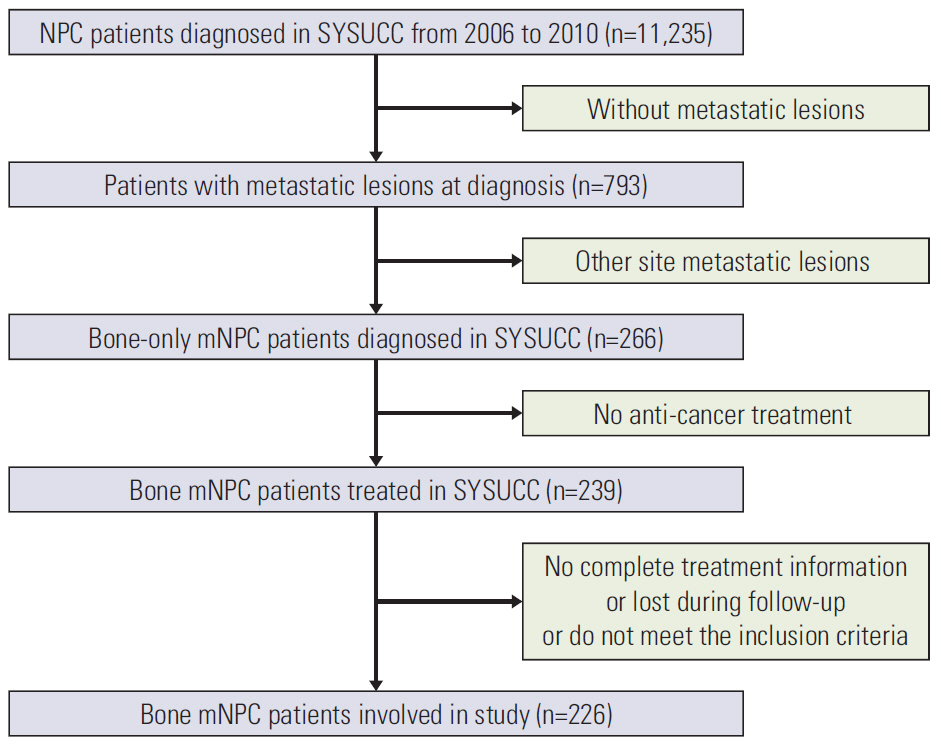
From November 2006 to October 2016, a total of 226 patients with bone-only metastasic NPC were retrospectively enrolled. All patients developed distant lesions before receiving treatment. All potential prognostic factors were considered and the correlation of the M1 subdivisions with overall survival (OS) was determined by Cox regression hazards model. Kaplan-Meier curves were used to appraise survival condition and log-rank testing was used to compare the differences.
RESULTS
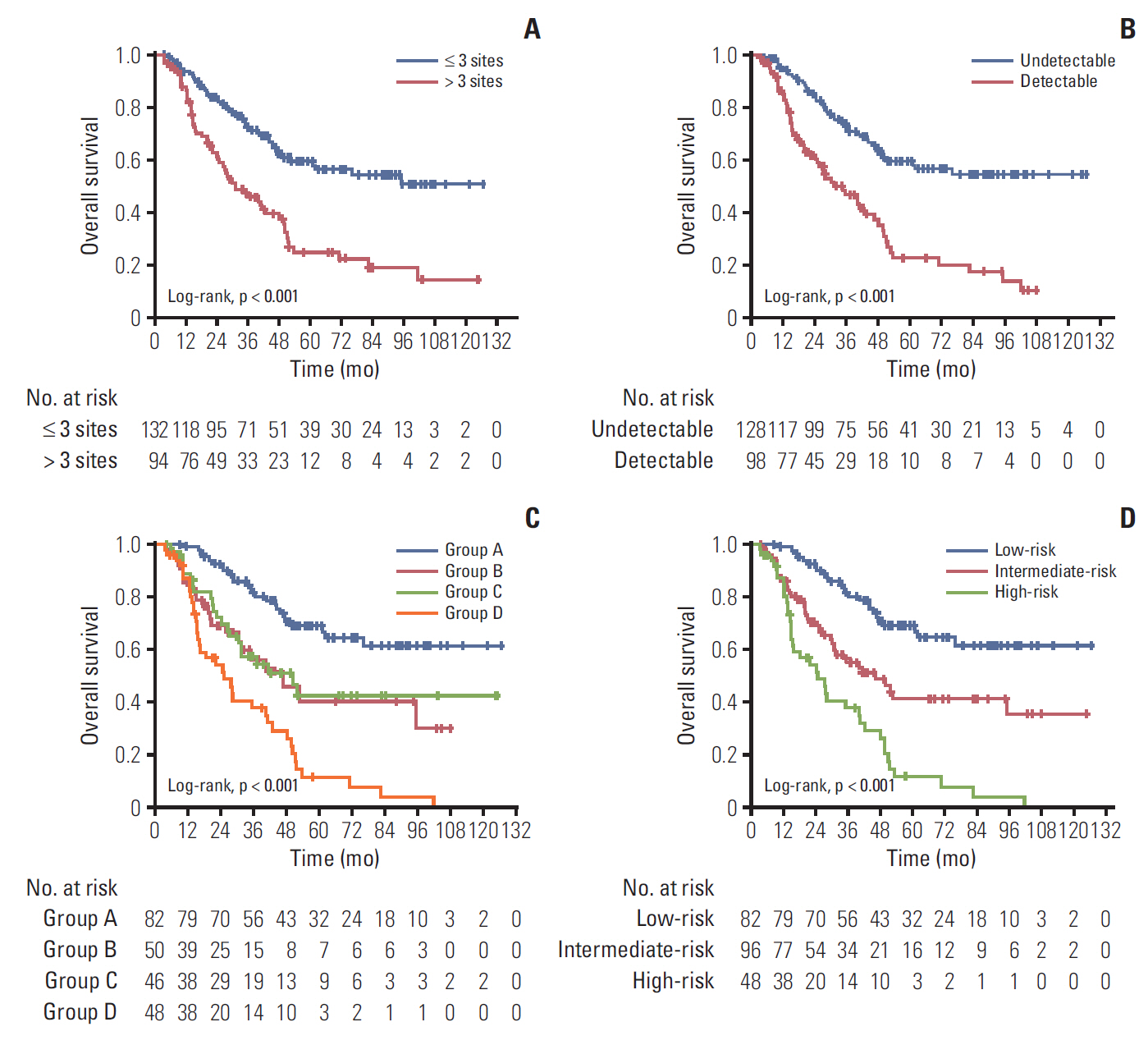
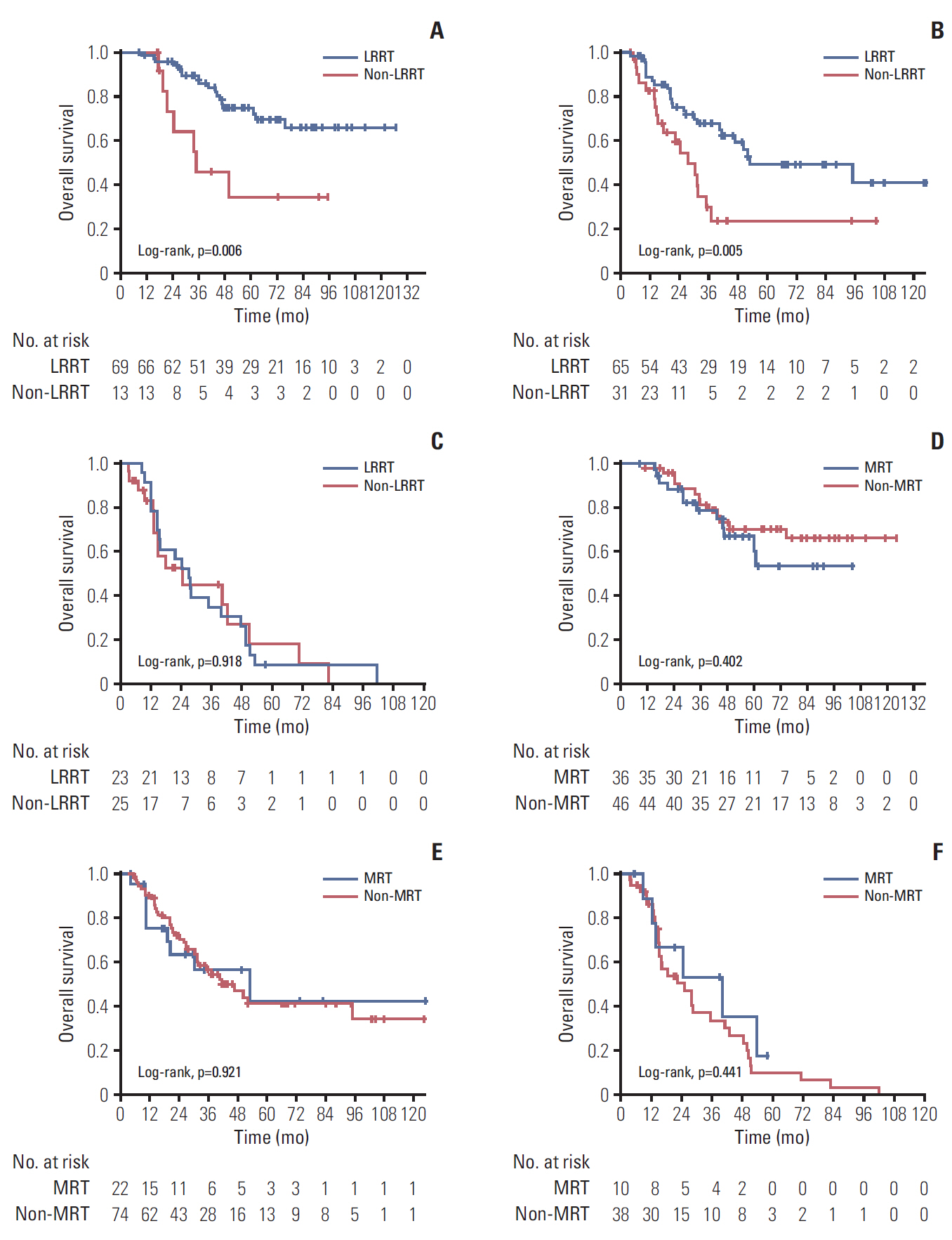
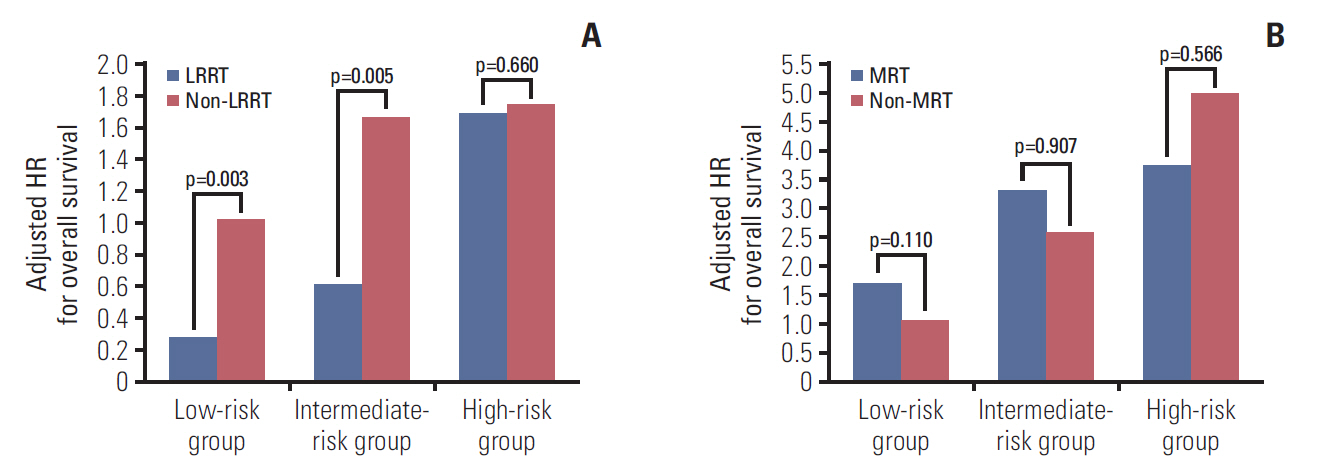
The median follow-up time was 33.9 months (range, 3 to 126 months). According to multivariate Cox proportional hazard analysis, the number of metastatic lesions and Epstein-Barr virus (EBV) DNA status after palliative chemotherapy (PCT) were independent prognostic factors for OS. Thus, we subdivided patients into three risk groups according to these two factors. Systemic chemotherapy combined with LRRT may benefit patients in low- and intermediate-risk groups but not in the high-risk group. Further aggressive MRT based on systemic chemotherapy showed no survival benefit in any risk group.
CONCLUSION
The stratification of NPC patients with bone-only metastasis based on EBV DNA after PCT and the number of metastatic lesions provided promising prognostic value and could aid clinicians in person-specific treatment.
MeSH Terms
Figure
Reference
-
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article2. Lee AW, Lin JC, Ng WT. Current management of nasopharyngeal cancer. Semin Radiat Oncol. 2012; 22:233–44.
Article3. Tang LQ, Chen QY, Fan W, Liu H, Zhang L, Guo L, et al. Prospective study of tailoring whole-body dual-modality [18F]fluorodeoxyglucose positron emission tomography/computed tomography with plasma Epstein-Barr virus DNA for detecting distant metastasis in endemic nasopharyngeal carcinoma at initial staging. J Clin Oncol. 2013; 31:2861–9.
Article4. Chen MY, Jiang R, Guo L, Zou X, Liu Q, Sun R, et al. Locoregional radiotherapy in patients with distant metastases of nasopharyngeal carcinoma at diagnosis. Chin J Cancer. 2013; 32:604–13.
Article5. Shen L, Dong J, Li S, Wang Y, Dong A, Shu W, et al. M1 stage subdivision and treatment outcome of patients with bone-only metastasis of nasopharyngeal carcinoma. Oncologist. 2015; 20:291–8.
Article6. Pan CC, Lu J, Yu JR, Chen P, Li W, Huang ZL, et al. Challenges in the modification of the M1 stage of the TNM staging system for nasopharyngeal carcinoma: a study of 1027 cases and review of the literature. Exp Ther Med. 2012; 4:334–8.
Article7. Ong YK, Heng DM, Chung B, Leong SS, Wee J, Fong KW, et al. Design of a prognostic index score for metastatic nasopharyngeal carcinoma. Eur J Cancer. 2003; 39:1535–41.
Article8. Leung SF, Teo PM, Shiu WW, Tsao SY, Leung TW. Clinical features and management of distant metastases of nasopharyngeal carcinoma. J Otolaryngol. 1991; 20:27–9.9. Bensouda Y, Kaikani W, Ahbeddou N, Rahhali R, Jabri M, Mrabti H, et al. Treatment for metastatic nasopharyngeal carcinoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2011; 128:79–85.
Article10. Chen C, Wu JB, Jiang H, Gao J, Chen JX, Pan CC, et al. A prognostic score for nasopharyngeal Carcinoma with bone metastasis: development and validation from multicenter. J Cancer. 2018; 9:797–806.
Article11. He S, Wang Y, Peng H, Yang L, Chen H, Liang S, et al. Pretreatment alkaline phosphatase and Epstein-Barr virus DNA predict poor prognosis and response to salvage radiotherapy in patients with nasopharyngeal carcinoma and metachronous bone-only metastasis. J Cancer. 2017; 8:417–24.
Article12. Pfister DG, Ang KK, Brizel DM, Burtness BA, Busse PM, Caudell JJ, et al. Head and neck cancers, version 2.2013. Featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2013; 11:917–23.13. Sun Y, Yu XL, Luo W, Lee AW, Wee JT, Lee N, et al. Recommendation for a contouring method and atlas of organs at risk in nasopharyngeal carcinoma patients receiving intensity-modulated radiotherapy. Radiother Oncol. 2014; 110:390–7.
Article14. Lo YM, Chan LY, Lo KW, Leung SF, Zhang J, Chan AT, et al. Quantitative analysis of cell-free Epstein-Barr virus DNA in plasma of patients with nasopharyngeal carcinoma. Cancer Res. 1999; 59:1188–91.15. Lin JC, Wang WY, Chen KY, Wei YH, Liang WM, Jan JS, et al. Quantification of plasma Epstein-Barr virus DNA in patients with advanced nasopharyngeal carcinoma. N Engl J Med. 2004; 350:2461–70.
Article16. Chan AT, Lo YM, Zee B, Chan LY, Ma BB, Leung SF, et al. Plasma Epstein-Barr virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinoma. J Natl Cancer Inst. 2002; 94:1614–9.
Article17. Liu LT, Tang LQ, Chen QY, Zhang L, Guo SS, Guo L, et al. The prognostic value of plasma Epstein-Barr viral DNA and tumor response to neoadjuvant chemotherapy in advanced-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2015; 93:862–9.
Article18. An X, Wang FH, Ding PR, Deng L, Jiang WQ, Zhang L, et al. Plasma Epstein-Barr virus DNA level strongly predicts survival in metastatic/recurrent nasopharyngeal carcinoma treated with palliative chemotherapy. Cancer. 2011; 117:3750–7.
Article19. Zou X, You R, Liu H, He YX, Xie GF, Xie ZH, et al. Establishment and validation of M1 stage subdivisions for de novo metastatic nasopharyngeal carcinoma to better predict prognosis and guide treatment. Eur J Cancer. 2017; 77:117–26.
Article20. Zeng L, Tian YM, Huang Y, Sun XM, Wang FH, Deng XW, et al. Retrospective analysis of 234 nasopharyngeal carcinoma patients with distant metastasis at initial diagnosis: therapeutic approaches and prognostic factors. PLoS One. 2014; 9:e108070.
Article21. Bhandari V, Jain RK. A retrospective study of incidence of bone metastasis in head and neck cancer. J Cancer Res Ther. 2013; 9:90–3.
Article22. Knudson G, Grinis G, Lopez-Majano V, Sansi P, Targonski P, Rubenstein M, et al. Bone scan as a stratification variable in advanced prostate cancer. Cancer. 1991; 68:316–20.
Article23. Yoon A, Choi CH, Kim TH, Choi JK, Park JY, Lee YY, et al. Bone metastasis in primary endometrial carcinoma: features, outcomes, and predictors. Int J Gynecol Cancer. 2014; 24:107–12.
Article24. Fandi A, Bachouchi M, Azli N, Taamma A, Boussen H, Wibault P, et al. Long-term disease-free survivors in metastatic undifferentiated carcinoma of nasopharyngeal type. J Clin Oncol. 2000; 18:1324–30.
Article25. Ji JH; Korean Cancer Study Group (KCSG), Yun T, Kim SB, Kang JH, Park JC, et al. A prospective multicentre phase II study of cisplatin and weekly docetaxel as first-line treatment for recurrent or metastatic nasopharyngeal cancer (KCSG HN07-01). Eur J Cancer. 2012; 48:3198–204.
Article26. Chen C, Wang FH, An X, Luo HY, Wang ZQ, Liang Y, et al. Triplet combination with paclitaxel, cisplatin and 5-FU is effective in metastatic and/or recurrent nasopharyngeal carcinoma. Cancer Chemother Pharmacol. 2013; 71:371–8.
Article27. Yeh SA, Tang Y, Lui CC, Huang EY. Treatment outcomes of patients with AJCC stage IVC nasopharyngeal carcinoma: benefits of primary radiotherapy. Jpn J Clin Oncol. 2006; 36:132–6.
Article28. Trilling GM, Cho H, Ugas MA, Saeed S, Katunda A, Jerjes W, et al. Spinal metastasis in head and neck cancer. Head Neck Oncol. 2012; 4:36.
Article29. Khot A, Love C, Garg MK, Haigentz M Jr. Long-term disease control in a patient with recurrent bone-only oligometastatic nasopharyngeal carcinoma. J Clin Oncol. 2016; 34:e25–6.
Article30. Lim A, Corry J, Lau E, Rischin D. Prolonged remission in a patient with nasopharyngeal carcinoma with a solitary bone metastasis. J Clin Oncol. 2011; 29:e135–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Establishment and Validation of a Nomogram for Nasopharyngeal Carcinoma Patients Concerning the Prognostic Effect of Parotid Lymph Node Metastases
- A Case of Cutaneous Metastasis of Nasopharyngeal Carcinoma on the Face
- Four Cases of Metastasectomy for Pulmonary Metastasis of Nasopharyngeal Carcinoma
- The Radiotherapy Result of the Nasopharyngeal Carcinoma
- A Case of Hypertrophic Osteoarthropathy Associated with Nasopharyngeal Carcinoma in a Child