Cancer Res Treat.
2020 Jul;52(3):855-866. 10.4143/crt.2019.772.
Establishment and Validation of a Nomogram for Nasopharyngeal Carcinoma Patients Concerning the Prognostic Effect of Parotid Lymph Node Metastases
- Affiliations
-
- 1Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China
- 2Department of Nasopharyngeal Carcinoma, Sun Yat-sen University Cancer Center, Guangzhou, China
- 3Department of Radiology, Sun Yat-sen University Cancer Center, Guangzhou, China
- KMID: 2504465
- DOI: http://doi.org/10.4143/crt.2019.772
Abstract
- Purpose
The prognosis of nasopharyngeal carcinoma (NPC) patients with parotid lymph node (PLN) metastasis remains unclear. This study was performed to investigate the prognostic significance and optimal staging category of PLN metastasis and develop a nomogram for estimating individual risk.
Materials and Methods
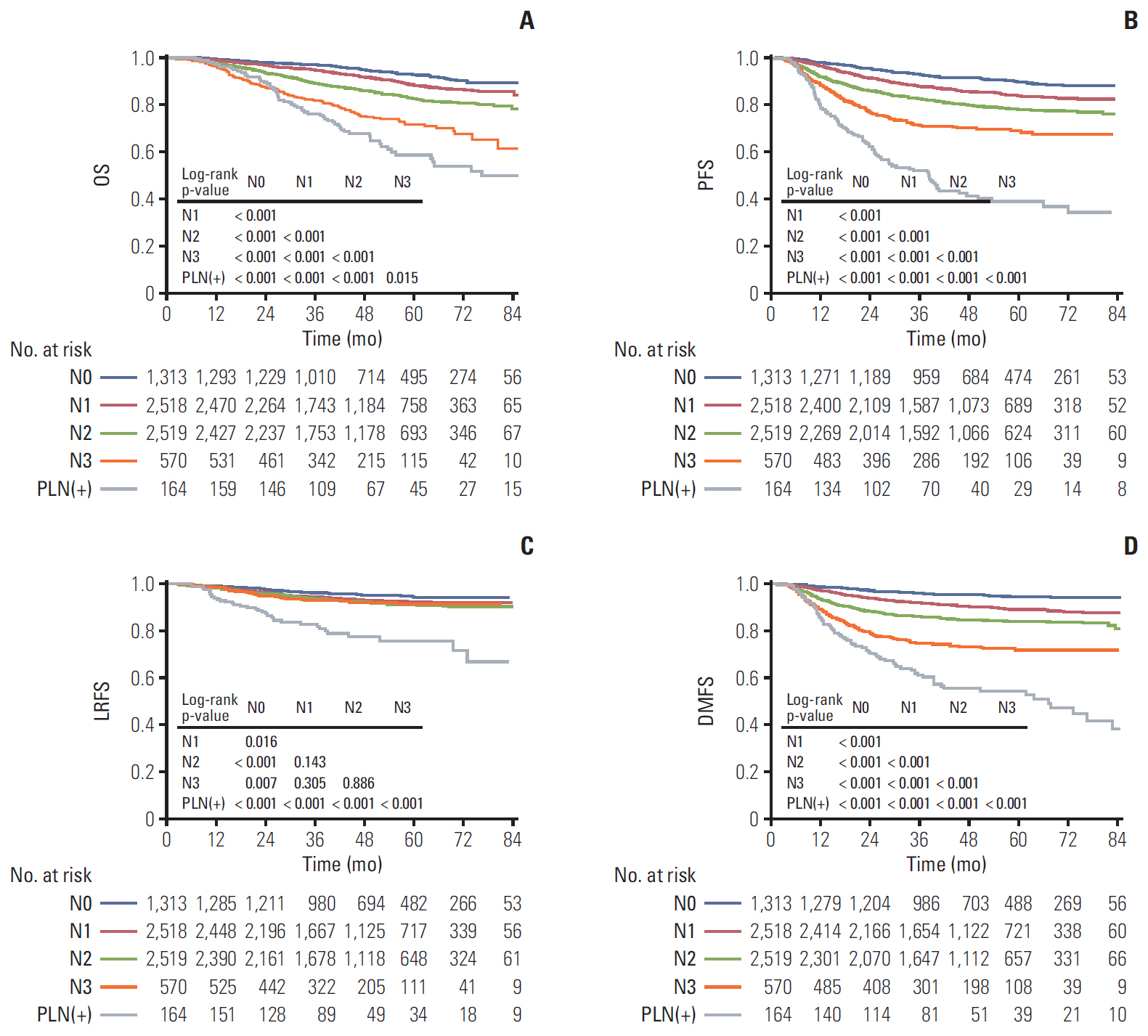
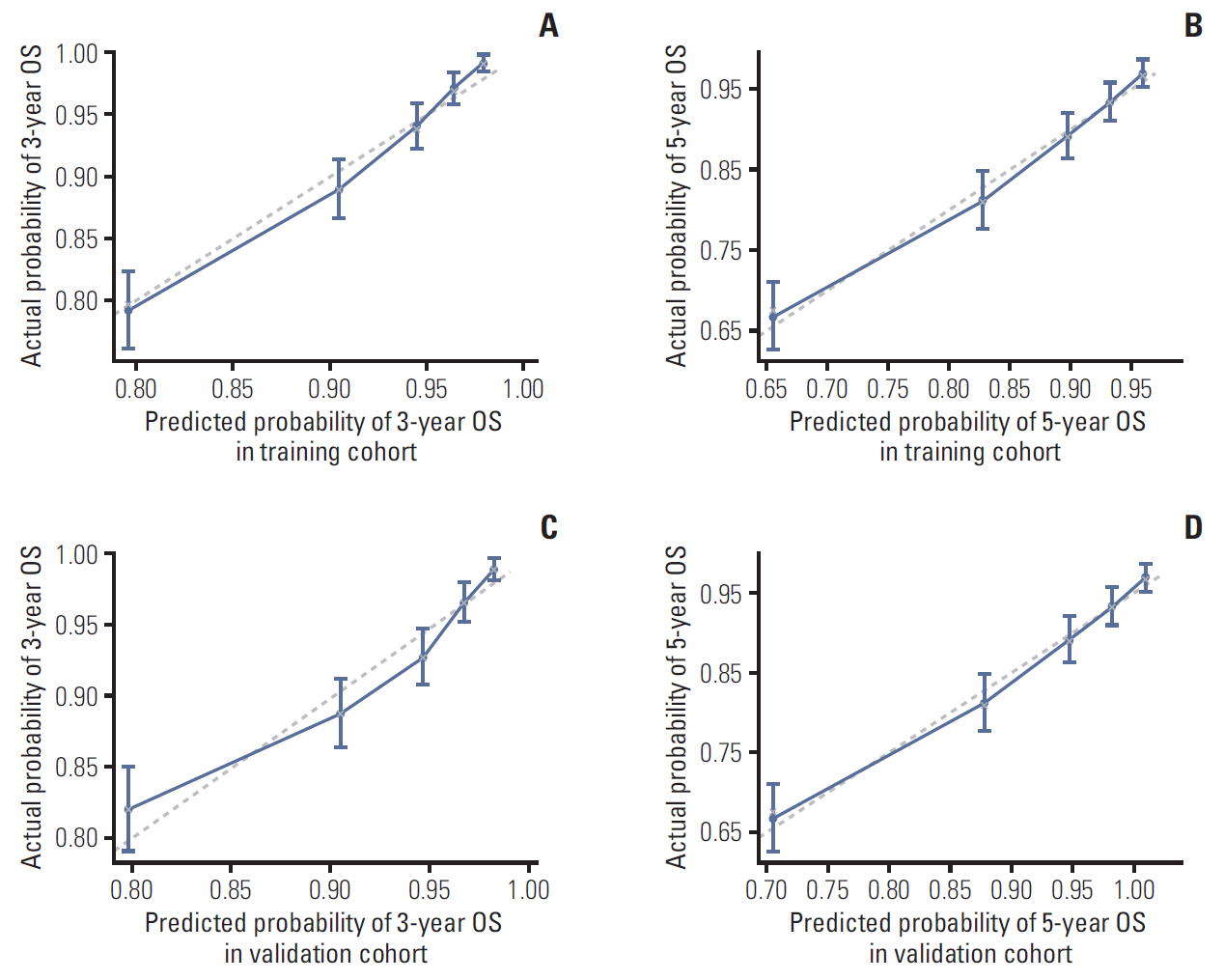
Clinical data of 7,084 non-metastatic NPC patients were retrospectively reviewed. Overall survival (OS) was the primary endpoint. A nomogram was established based on the Cox proportional hazards regression model. The accuracy and calibration ability of this nomogram was evaluated by C-index and calibration curves with bootstrap validation. Result Totally, 164/7,084 NPC patients (2.3%) presented with PLNs. Multivariate analyses showed that PLN metastasis was a negative prognostic factor for OS, progression-free survival (PFS), distant metastasis-free survival (DMFS), and locoregional relapse-free survival (LRFS). Patients with PLN metastasis had a worse prognosis than N3 disease. Five independent prognostic factors were included in the nomogram, which showed a C-index of 0.743. The calibration curves for probability of 3- and 5-year OS indicated satisfactory agreement between nomogram-based prediction and actual observation. All results were confirmed in the validation cohort.
Conclusion
NPC patient with PLN metastasis had poorer survival outcome (OS, PFS, DMFS, and LRFS) than N3 disease. We developed a nomogram to provide individual prediction of OS for patients with PLN metastasis.
Keyword
Figure
Reference
-
References
1. Cao SM, Simons MJ, Qian CN. The prevalence and prevention of nasopharyngeal carcinoma in China. Chin J Cancer. 2011; 30:114–9.
Article2. Simons MJ. The origin of genetic risk for nasopharyngeal carcinoma:a commentary on: is nasopharyngeal cancer really a "Cantonese cancer"? Chin J Cancer. 2010; 29:527–37.3. Ho FC, Tham IW, Earnest A, Lee KM, Lu JJ. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: a meta-analysis of clinical evidence. BMC Cancer. 2012; 12:98.
Article4. Tang L, Mao Y, Liu L, Liang S, Chen Y, Sun Y, et al. The volume to be irradiated during selective neck irradiation in nasopharyngeal carcinoma: analysis of the spread patterns in lymph nodes by magnetic resonance imaging. Cancer. 2009; 115:680–8.5. King AD, Ahuja AT, Leung SF, Lam WW, Teo P, Chan YL, et al. Neck node metastases from nasopharyngeal carcinoma: MR imaging of patterns of disease. Head Neck. 2000; 22:275–81.
Article6. Wang X, Li L, Hu C, Zhou Z, Ying H, Ding J, et al. Patterns of level II node metastasis in nasopharyngeal carcinoma. Radiother Oncol. 2008; 89:28–32.
Article7. Chong VF, Fan YF. Parotid gland involvement in nasopharyngeal carcinoma. J Comput Assist Tomogr. 1999; 23:524–8.
Article8. Kwong DL, Pow EH, Sham JS, McMillan AS, Leung LH, Leung WK, et al. Intensity-modulated radiotherapy for early-stage nasopharyngeal carcinoma: a prospective study on disease control and preservation of salivary function. Cancer. 2004; 101:1584–93.9. Kam MK, Leung SF, Zee B, Chau RM, Suen JJ, Mo F, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol. 2007; 25:4873–9.
Article10. Cannon DM, Lee NY. Recurrence in region of spared parotid gland after definitive intensity-modulated radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys. 2008; 70:660–5.
Article11. Cao CN, Luo JW, Gao L, Xu GZ, Li SY, Xiao JP. Recurrence of nasopharyngeal carcinoma in the parotid region after definitive intensity-modulated radiotherapy. J Oral Maxillofac Surg. 2013; 71:1993–7.
Article12. Lin DS, Jen YM, Lee JC, Liu SC, Lin YS. Recurrence of nasopharyngeal carcinoma in the parotid region after parotidgland-sparing radiotherapy. J Formos Med Assoc. 2011; 110:655–60.
Article13. Pan JJ, Ng WT, Zong JF, Chan LL, O'Sullivan B, Lin SJ, et al. Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer. 2016; 122:546–58.
Article14. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York, NY: Springer International Publishing;2017.15. Zhang Y, Li WF, Chen L, Mao YP, Guo R, Zhang F, et al. Prognostic value of parotid lymph node metastasis in patients with nasopharyngeal carcinoma receiving intensity-modulated radiotherapy. Sci Rep. 2015; 5:13919.
Article16. Xu Y, Chen X, Zhang M, Xiao Y, Zong J, Guo Q, et al. Prognostic effect of parotid area lymph node metastases after preliminary diagnosis of nasopharyngeal carcinoma: a propensity score matching study. Cancer Med. 2017; 6:2213–21.
Article17. Gregoire V, Ang K, Budach W, Grau C, Hamoir M, Langendijk JA, et al. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol. 2014; 110:172–81.18. van den Brekel MW, Stel HV, Castelijns JA, Nauta JJ, van der Waal I, Valk J, et al. Cervical lymph node metastasis: assessment of radiologic criteria. Radiology. 1990; 177:379–84.
Article19. Tang L, Li L, Mao Y, Liu L, Liang S, Chen Y, et al. Retropharyngeal lymph node metastasis in nasopharyngeal carcinoma detected by magnetic resonance imaging : prognostic value and staging categories. Cancer. 2008; 113:347–54.20. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–47.
Article21. Lee AW, Lau KY, Hung WM, Ng WT, Lee MC, Choi CW, et al. Potential improvement of tumor control probability by induction chemotherapy for advanced nasopharyngeal carcinoma. Radiother Oncol. 2008; 87:204–10.
Article22. Lin S, Lu JJ, Han L, Chen Q, Pan J. Sequential chemotherapy and intensity-modulated radiation therapy in the management of locoregionally advanced nasopharyngeal carcinoma: experience of 370 consecutive cases. BMC Cancer. 2010; 10:39.
Article23. Yu Z, Luo W, Zhou QC, Zhang QH, Kang DH, Liu MZ. Impact of changing gross tumor volume delineation of intensity-modulated radiotherapy on the dose distribution and clinical treatment outcome after induction chemotherapy for the primary locoregionally advanced nasopharyngeal carcinoma. Ai Zheng. 2009; 28:1132–7.
Article24. Tang LL, Chen YP, Mao YP, Wang ZX, Guo R, Chen L, et al. Validation of the 8th edition of the UICC/AJCC staging system for nasopharyngeal carcinoma from endemic areas in the intensity-modulated radiotherapy era. J Natl Compr Canc Netw. 2017; 15:913–9.
Article25. Cho JK, Lee GJ, Yi KI, Cho KS, Choi N, Kim JS, et al. Development and external validation of nomograms predictive of response to radiation therapy and overall survival in nasopharyngeal cancer patients. Eur J Cancer. 2015; 51:1303–11.
Article26. Tang LQ, Li CF, Li J, Chen WH, Chen QY, Yuan LX, et al. Establishment and validation of prognostic nomograms for endemic nasopharyngeal carcinoma. J Natl Cancer Inst. 2016; 108:djv291.
Article27. Song C, Yang S. A meta-analysis on the EBV DNA and VCA-IgA in diagnosis of Nasopharyngeal Carcinoma. Pak J Med Sci. 2013; 29:885–90.
Article28. Lin JC, Wang WY, Chen KY, Wei YH, Liang WM, Jan JS, et al. Quantification of plasma Epstein-Barr virus DNA in patients with advanced nasopharyngeal carcinoma. N Engl J Med. 2004; 350:2461–70.
Article29. Chan AT, Lo YM, Zee B, Chan LY, Ma BB, Leung SF, et al. Plasma Epstein-Barr virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinoma. J Natl Cancer Inst. 2002; 94:1614–9.
Article30. Wang WY, Twu CW, Chen HH, Jan JS, Jiang RS, Chao JY, et al. Plasma EBV DNA clearance rate as a novel prognostic marker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010; 16:1016–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nomogram for Predicting Central Lymph Node Metastasis in Papillary Thyroid Cancer: A Retrospective Cohort Study of Two Clinical Centers
- Prognostic Factors For Survival in Patients with Lymph Node Metastasis Identified at the Time of Surgery for Cervical Carcinoma
- Surgical Treatment of Cancer of the Orbit with Lymph Node Metastasis of Parotid Gland
- Mode of Parotid Invasion and Parotid Lymph Node Metastasis in External Auditory Canal Carcinoma
- Predictors of Axillary Node Metastases in Patients with T1 Breast Carcinoma