J Korean Diabetes.
2018 Dec;19(4):237-245. 10.4093/jkd.2018.19.4.237.
Blood Sugar Control and Low-Carbohydrate High-Fat Diet
- Affiliations
-
- 1Clinical Dietitian Health Screening Administration, Asan Medical Center, Seoul, Korea. ehkang@amc.seoul.kr
- KMID: 2442363
- DOI: http://doi.org/10.4093/jkd.2018.19.4.237
Abstract
- Diabetes patients and pre-diabetic patients are increasing worldwide. Type 2 diabetes starts with insulin resistance, and the long-term habit of stimulating insulin secretions causes insulin resistance and accumulates body fat to develop obesity and non-alcoholic fatty liver into diabetes. It also causes a variety of chronic diseases such as high blood pressure, polycystic ovary diseases, cancer and dementia. Insulin resistance is caused by an unbalanced lifestyle, and among other factors, the balance of the macronutrient is a very important factor. Koreans are characterized by high carbohydrate intake. Given the increasing prevalence of diabetes and the characteristics of Korean physical and eating habits, a more effective balance of diet education is needed. Therefore, it is very important for clinical dietitian to understand the carbohydrate and fat metabolism caused by insulin, and the concept of balanced diet for blood sugar control needs to be shifted from low-fat high-carbohydrate diet to low-carbohydrate high-fat diet.
Keyword
MeSH Terms
Figure
Reference
-
1. Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011; 378:31–40.
Article2. Crofts C, Schofield G, Zinn C, Wheldon M, Kraft J. Identifying hyperinsulinaemia in the absence of impaired glucose tolerance: an examination of the Kraft database. Diabetes Res Clin Pract. 2016; 118:50–57.
Article3. DiNicolantonio JJ, Bhutani J, OKeefe JH, Crofts C. Postprandial insulin assay as the earliest biomarker for diagnosing pre-diabetes, type 2 diabetes and increased cardiovascular risk. Open Heart. 2017; 4:e000656.
Article4. Kelly CT, Mansoor J, Dohm GL, Chapman WH 3rd, Pender JR 4th, Pories WJ. Hyperinsulinemic syndrome: the metabolic syndrome is broader than you think. Surgery. 2014; 156:405–411.
Article5. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016; 387:1377–1396.6. Kimura N, Keys A. Coronary heart disease in seven countries. X. Rural southern Japan. Circulation. 1970; 41:4 Suppl. I101–I112.7. United States. Congress. Senate. Select Committee on Nutrition and Human Needs. Dietary goals for the United States. 2nd ed. Washington: U.S. Government;1977.8. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003; 289:76–79.
Article9. Medina-Santillán R, López-Velázquez JA, Chávez-Tapia N, Torres-Villalobos G, Uribe M, Méndez-Sánchez N. Hepatic manifestations of metabolic syndrome. Diabetes Metab Res Rev. 2013; DOI: 10.1002/dmrr.2410. [Epub ahead of print].
Article10. Milman S, Crandall JP. Mechanisms of vascular complications in prediabetes. Med Clin North Am. 2011; 95:309–325. vii
Article11. Reaven GM. The role of insulin resistance and hyperinsulinemia in coronary heart disease. Metabolism. 1992; 41:5 Suppl 1. 16–19.
Article12. Yoon YS, Keum N, Zhang X, Cho E, Giovannucci EL. Hyperinsulinemia, insulin resistance and colorectal adenomas: a meta-analysis. Metabolism. 2015; 64:1324–1333.
Article13. Umegaki H. Insulin resistance in the brain: a new therapeutic target for Alzheimer's disease. J Diabetes Investig. 2013; 4:150–151.
Article14. Mu L, Zhao Y, Lai Y, Li R, Qiao J. Insulin resistance and β-cell dysfunction and the relationship with cardiometabolic disorders among women with polycystic ovary syndrome. Clin Endocrinol (Oxf). 2018; 89:779–788.
Article15. Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet. 2011; 378:169–181.
Article16. Mehran AE, Templeman NM, Brigidi GS, Lim GE, Chu KY, Hu X, Botezelli JD, Asadi A, Hoffman BG, Kieffer TJ, Bamji SX, Clee SM, Johnson JD. Hyperinsulinemia drives diet-induced obesity independently of brain insulin production. Cell Metab. 2012; 16:723–737.
Article17. Ludwig DS, Friedman MI. Increasing adiposity: consequence or cause of overeating? JAMA. 2014; 311:2167–2168.18. Flannery C, Dufour S, Rabøl R, Shulman GI, Petersen KF. Skeletal muscle insulin resistance promotes increased hepatic de novo lipogenesis, hyperlipidemia, and hepatic steatosis in the elderly. Diabetes. 2012; 61:2711–2717.
Article19. Perry RJ, Samuel VT, Petersen KF, Shulman GI. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature. 2014; 510:84–91.
Article20. Petersen KF, Dufour S, Savage DB, Bilz S, Solomon G, Yonemitsu S, Cline GW, Befroy D, Zemany L, Kahn BB, Papademetris X, Rothman DL, Shulman GI. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci U S A. 2007; 104:12587–12594.
Article21. Hayashi T, Boyko EJ, Sato KK, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Patterns of insulin concentration during the OGTT predict the risk of type 2 diabetes in Japanese Americans. Diabetes Care. 2013; 36:1229–1235.
Article22. Facchini FS, Hua N, Abbasi F, Reaven GM. Insulin resistance as a predictor of age-related diseases. J Clin Endocrinol Metab. 2001; 86:3574–3578.
Article23. Frayn KN. Metabolic regulation: a human perspective. 3rd ed. Chichester: Wiley-Blackwell;2010. p. 108. p. 131.24. Jensen MD, Caruso M, Heiling V, Miles JM. Insulin regulation of lipolysis in nondiabetic and IDDM subjects. Diabetes. 1989; 38:1595–1601.
Article25. Bell GI, Fukumoto H, Burant CF, Seino S, Sivitz WI, Pessin JE. Facilitative glucose transport proteins: structure and regulation of expression in adipose tissue. Int J Obes. 1991; 15:Suppl 2. 127–132.26. Burant CF, Sivitz WI, Fukumoto H, Kayano T, Nagamatsu S, Seino S, Pessin JE, Bell GI. Mammalian glucose transporters: structure and molecular regulation. Recent Prog Horm Res. 1991; 47:349–387. discussion 387-8.
Article27. DeFronzo RA, Jacot E, Jequier E, Maeder E, Wahren J, Felber JP. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes. 1981; 30:1000–1007.
Article28. Taylor R, Price TB, Katz LD, Shulman RG, Shulman GI. Direct measurement of change in muscle glycogen concentration after a mixed meal in normal subjects. Am J Physiol. 1993; 265:E224–E229.
Article29. Bugianesi E, McCullough AJ, Marchesini G. Insulin resistance: a metabolic pathway to chronic liver disease. Hepatology. 2005; 42:987–1000.
Article30. Taylor R, Magnusson I, Rothman DL, Cline GW, Caumo A, Cobelli C, Shulman GI. Direct assessment of liver glycogen storage by 13C nuclear magnetic resonance spectroscopy and regulation of glucose homeostasis after a mixed meal in normal subjects. J Clin Invest. 1996; 97:126–132.
Article31. Avramoglu RK, Basciano H, Adeli K. Lipid and lipoprotein dysregulation in insulin resistant states. Clin Chim Acta. 2006; 368:1–19.
Article32. Chang JH, Lee HS, Kang EH. A study on dietary habits, nutrient intakes and dietary quality in adults of a health screening and promotion center according to nonalcoholic fatty liver disease. J Nutr Health. 2014; 47:330–341.
Article33. Delarue J, Normand S, Couet C, Pachiaudi C, Urbain C, Lamisse F, Riou JP. Effects of free fatty acids on the metabolic response to oral fructose in lean healthy humans. Int J Obes Relat Metab Disord. 1996; 20:130–136.34. Zhang C, Chen X, Zhu RM, Zhang Y, Yu T, Wang H, Zhao H, Zhao M, Ji YL, Chen YH, Meng XH, Wei W, Xu DX. Endoplasmic reticulum stress is involved in hepatic SREBP-1c activation and lipid accumulation in fructose-fed mice. Toxicol Lett. 2012; 212:229–240.
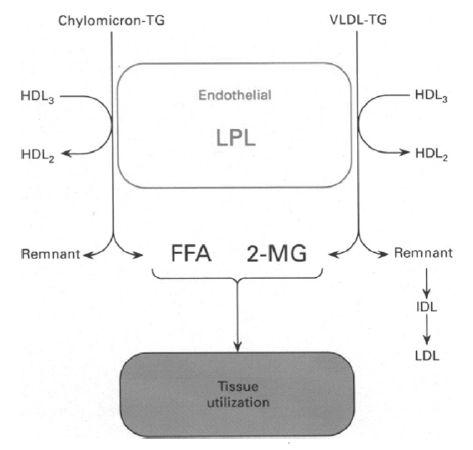
Article35. Olivecrona T, Hultin M, Bergö M, Olivecrona G. Lipoprotein lipase: regulation and role in lipoprotein metabolism. Proc Nutr Soc. 1997; 56:723–729.
Article36. Braun JE, Severson DL. Regulation of the synthesis, processing and translocation of lipoprotein lipase. Biochem J. 1992; 287:337–347.
Article37. Hashim SA. Dietary fats and adipose tissue fatty acid composition. Prev Med. 1983; 12:854–867.
Article38. Silveira LR, Fiamoncini J, Hirabara SM, Procópio J, Cambiaghi TD, Pinheiro CH, Lopes LR, Curi R. Updating the effects of fatty acids on skeletal muscle. J Cell Physiol. 2008; 217:1–12.
Article39. Arora S, McFarlane SI. Review on “Atkins Diabetes Revolution: The Groundbreaking Approach to Preventing and Controlling Type 2 Diabetes” by Mary C. Vernon and Jacqueline A. Eberstein. Nutr Metab (Lond). 2004; 1:14.40. Khazrai YM, Defeudis G, Pozzilli P. Effect of diet on type 2 diabetes mellitus: a review. Diabetes Metab Res Rev. 2014; 30:Suppl 1. 24–33.
Article41. Korsmo-Haugen HK, Brurberg KG, Mann J, Aas AM. Carbohydrate quantity in the dietary management of type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2019; 21:15–27.
Article42. Dyson P. Low carbohydrate diets and type 2 diabetes: what is the latest evidence? Diabetes Ther. 2015; 6:411–424.
Article43. Lee YJ, Song S, Song Y. High-carbohydrate diets and food patterns and their associations with metabolic disease in the Korean population. Yonsei Med J. 2018; 59:834–842.
Article44. Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr. 2013; 97:848–853.45. Yun S, Kim HJ, Oh K. Trends in energy intake among Korean adults, 1998-2015: results from the Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2017; 11:147–154.
Article46. Lee JR, Yeh HC. Trends in the prevalence of type 2 diabetes and its association with mortality rates in Asians vs. Whites: results from the United States National Health Interview Survey from 2000 to 2014. J Diabetes Complications. 2018; 32:539–544.
Article47. Roh E, Kim KM, Park KS, Kim YJ, Chun EJ, Choi SH, Park KS, Jang HC, Lim S. Comparison of pancreatic volume and fat amount linked with glucose homeostasis between healthy Caucasians and Koreans. Diabetes Obes Metab. 2018; 20:2642–2652.
Article48. Gadgil MD, Appel LJ, Yeung E, Anderson CA, Sacks FM, Miller ER 3rd. The effects of carbohydrate, unsaturated fat, and protein intake on measures of insulin sensitivity: results from the OmniHeart trial. Diabetes Care. 2013; 36:1132–1137.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a Low-carbohydrate, High-fat Diet
- Corrigendum: Text Correction: Blood Sugar Control and Low-Carbohydrate High-Fat Diet
- Development and Application of Low-Carbohydrates and Low-Simple Sugar Nutrition Education Materials for Non-Alcoholic Fatty Liver Disease Patients
- Ketogenic Diet and Glucose Control
- Low-Carbohydrate Diets in Korea: Why Does It Matter, and What Is Next?