World J Mens Health.
2018 May;36(2):153-160. 10.5534/wjmh.17010.
Improvement of Persistent Detrusor Overactivity through Treatment with a Phytotherapeutic Agent (WSY-1075) after Relief of Bladder Outlet Obstruction
- Affiliations
-
- 1Department of Urology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ksw1227@catholic.ac.kr
- 2Department of Urology, Institute of Biomedical Industry, The Catholic University of Korea, Seoul, Korea.
- 3Catholic Integrative Medicine Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Korea Biomedical Science Institute, Seoul, Korea.
- KMID: 2419314
- DOI: http://doi.org/10.5534/wjmh.17010
Abstract
- PURPOSE
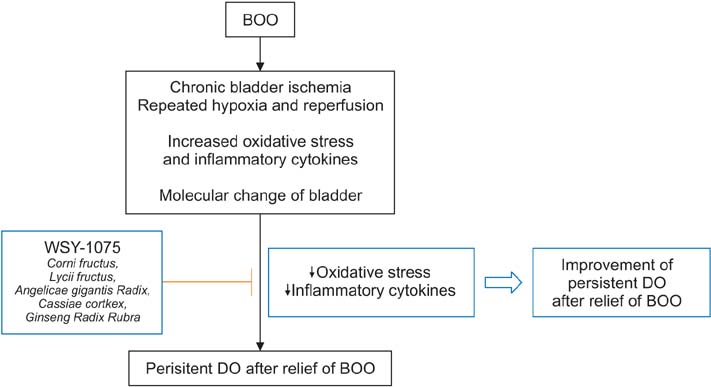
Many patients with benign prostatic hyperplasia need treatment for remaining storage symptoms after surgery. Therefore, we evaluated the effect of the phytotherapeutic agent WSY-1075 on persistent detrusor overactivity (DO) after the relief of bladder outlet obstruction (BOO).
MATERIALS AND METHODS
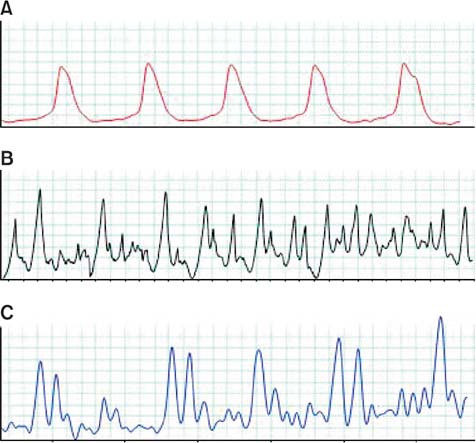
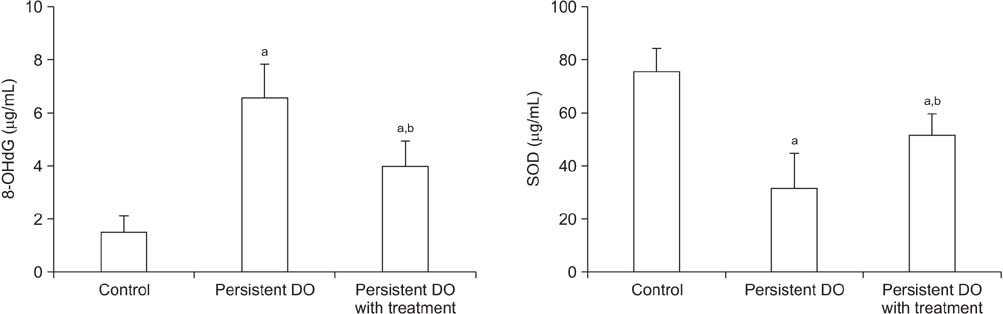
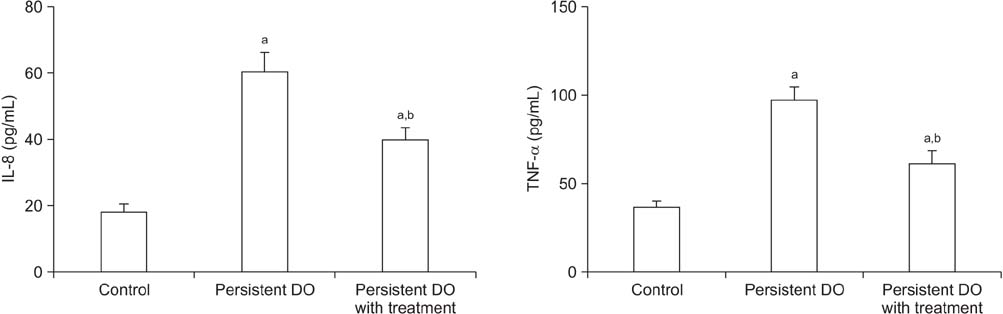
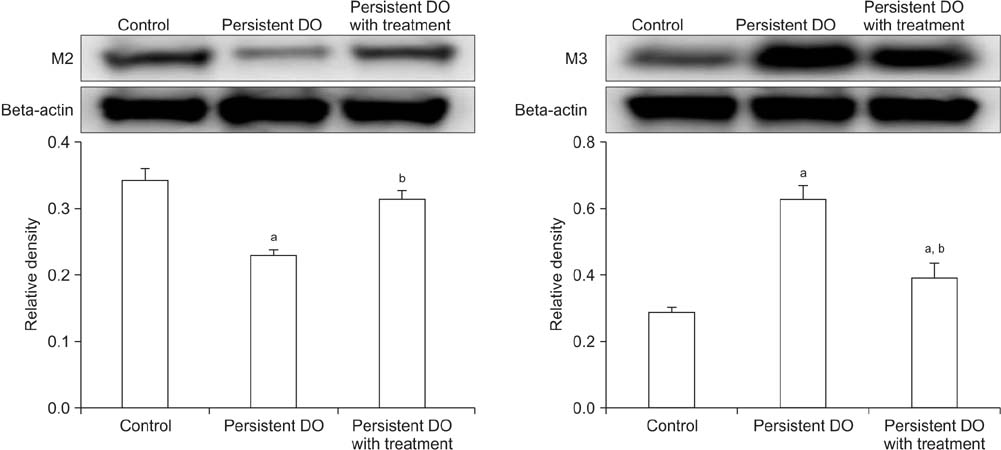
Rats were assigned to 3 groups: control (n=6), persistent DO (n=6), and persistent DO treated with the phytotherapeutic agent WSY-1075 (n=6). Persistent DO after relief of partial BOO was generated in the rat model, and 6 of the rats with this condition were orally administered WSY-1075. After 4 weeks of administration, cystometry was performed. Additionally, 8-hydroxy-2-deoxyguanosine and superoxide dismutase were measured to evaluate oxidative stress in the bladder. Pro-inflammatory cytokines, such as interleukin-8 and tumor necrosis factor-α, were analyzed, as were the M2 and M3 muscarinic receptors of the bladder.
RESULTS
Significantly increased contraction pressure and a decreased contraction interval were observed in the persistent DO group after relief of BOO. Moreover, oxidative stress, pro-inflammatory cytokines, and M3 muscarinic receptors were significantly increased. After treatment with WSY-1075, significantly reduced DO was observed by cystometry in comparison with the persistent DO group. Additionally, significantly decreased levels of oxidative stress, pro-inflammatory cytokines, and M3 muscarinic receptors in the bladder were observed after treatment with WSY-1075.
CONCLUSIONS
Treatment with WSY-1075 improved persistent DO after the relief of BOO mediated by antioxidative and anti-inflammatory effects. Further studies are necessary to identify the exact mechanism of the treatment effect of WSY-1075.
Keyword
MeSH Terms
-
Animals
Cytokines
Humans
Interleukin-8
Lower Urinary Tract Symptoms
Models, Animal
Necrosis
Oxidative Stress
Phytotherapy
Prostatic Hyperplasia
Rats
Receptors, Muscarinic
Superoxide Dismutase
Urinary Bladder Neck Obstruction*
Urinary Bladder*
Urinary Bladder, Overactive
Cytokines
Interleukin-8
Receptors, Muscarinic
Superoxide Dismutase
Figure
Reference
-
1. Sarma AV, Wei JT. Clinical practice. Benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med. 2012; 367:248–257.2. Lee YJ, Lee JW, Park J, Seo SI, Chung JI, Yoo TK, et al. Nationwide incidence and treatment pattern of benign prostatic hyperplasia in Korea. Investig Clin Urol. 2016; 57:424–430.
Article3. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109.
Article4. Barkin J, Diles D, Franks B, Berner T. Alpha blocker monotherapy versus combination therapy with antimuscarinics in men with persistent LUTS refractory to alpha-adrenergic treatment: patterns of persistence. Can J Urol. 2015; 22:7914–7923.5. Cho SY, Ro YK, Kim H, Son H. Preoperative urinary retention increased the risk of urinary retention after photoselective vaporization of the prostate. World J Mens Health. 2015; 33:182–187.
Article6. Shin YS, Zhang LT, You JH, Choi IS, Zhao C, Park JK. Efficacy and safety of tamsulosin hydrochloride 0.2 mg and combination of tamsulosin hydrochloride 0.2 mg plus solifenacin succinate 5 mg after transurethral resection of the prostate: a prospective, randomized controlled trial. Clin Interv Aging. 2016; 11:1301–1307.7. Pagano E, Laudato M, Griffo M, Capasso R. Phytotherapy of benign prostatic hyperplasia. A minireview. Phytother Res. 2014; 28:949–955.
Article8. Park JW, Jeong HC, Moon HW, Cho SJ, Yang JH, Kim WH, et al. Anti-inflammatory and antimicrobial effects of a novel herbal formulation (WSY-1075) in a chronic bacterial prostatitis rat model. World J Mens Health. 2016; 34:179–185.
Article9. Jin LH, Andersson KE, Han JU, Kwon YH, Park CS, Shin HY, et al. Persistent detrusor overactivity in rats after relief of partial urethral obstruction. Am J Physiol Regul Integr Comp Physiol. 2011; 301:R896–R904.
Article10. Nishiguchi J, Kwon DD, Kaiho Y, Chancellor MB, Kumon H, Snyder PB, et al. Suppression of detrusor overactivity in rats with bladder outlet obstruction by a type 4 phosphodiesterase inhibitor. BJU Int. 2007; 99:680–686.
Article11. Lin AT, Juan YS. Ischemia, hypoxia and oxidative stress in bladder outlet obstruction and bladder overdistention injury. Low Urin Tract Symptoms. 2012; 4:Suppl 1. 27–31.
Article12. Koritsiadis G, Stravodimos K, Koutalellis G, Agrogiannis G, Koritsiadis S, Lazaris A, et al. Immunohistochemical estimation of hypoxia in human obstructed bladder and correlation with clinical variables. BJU Int. 2008; 102:328–332.
Article13. Azadzoi KM, Tarcan T, Kozlowski R, Krane RJ, Siroky MB. Overactivity and structural changes in the chronically ischemic bladder. J Urol. 1999; 162:1768–1778.
Article14. Parsons BA, Drake MJ. Animal models in overactive bladder research. Handb Exp Pharmacol. 2011; (202):15–43.
Article15. Sasaki M, Joh T. Oxidative stress and ischemia-reperfusion injury in gastrointestinal tract and antioxidant, protective agents. J Clin Biochem Nutr. 2007; 40:1–12.
Article16. Matsui T, Oka M, Fukui T, Tanaka M, Oyama T, Sagawa K, et al. Suppression of bladder overactivity and oxidative stress by the phytotherapeutic agent, Eviprostat, in a rat model of atherosclerosis-induced chronic bladder ischemia. Int J Urol. 2012; 19:669–675.
Article17. Nomiya M, Andersson KE, Yamaguchi O. Chronic bladder ischemia and oxidative stress: new pharmacotherapeutic targets for lower urinary tract symptoms. Int J Urol. 2015; 22:40–46.
Article18. Juan YS, Chuang SM, Mannikarottu A, Huang CH, Li S, Schuler C, et al. Coenzyme Q10 diminishes ischemia-reperfusion induced apoptosis and nerve injury in rabbit urinary bladder. Neurourol Urodyn. 2009; 28:339–342.
Article19. Kim JW, Jang HA, Bae JH, Lee JG. Effects of coenzyme Q10 on bladder dysfunction induced by chronic bladder ischemia in a rat model. J Urol. 2013; 189:2371–2376.
Article20. Kawai Y, Oka M, Kyotani J, Oyama T, Matsumoto S, Kakizaki H. Effect of the phytotherapeutic agent eviprostat on the bladder in a rat model of bladder overdistension/emptying. Neurourol Urodyn. 2013; 32:1031–1037.
Article21. Oka M, Fukui T, Ueda M, Tagaya M, Oyama T, Tanaka M. Suppression of bladder oxidative stress and inflammation by a phytotherapeutic agent in a rat model of partial bladder outlet obstruction. J Urol. 2009; 182:382–390.
Article22. Parekh MH, Lobel R, O'Connor LJ, Leggett RE, Levin RM. Protective effect of vitamin E on the response of the rabbit bladder to partial outlet obstruction. J Urol. 2001; 166:341–346.
Article23. Ishigooka M, Hashimoto T, Hayami S, Tomaru M, Nakada T, Mitobe K. Clinical and retrospective evaluation of Eviprostat: a non-hormonal and non-neuropharmacological agent for benign prostatic hyperplasia. Int Urol Nephrol. 1995; 27:61–66.
Article24. Sugimoto M, Oka M, Tsunemori H, Yamashita M, Kakehi Y. Effect of a phytotherapeutic agent, Eviprostat®, on prostatic and urinary cytokines/chemokines in a rat model of nonbacterial prostatitis. Prostate. 2011; 71:438–444.
Article25. Che CT, Wang ZJ, Chow MS, Lam CW. Herb-herb combination for therapeutic enhancement and advancement: theory, practice and future perspectives. Molecules. 2013; 18:5125–5141.
Article26. Kim HJ, Kim BH, Kim YC. Antioxidative action of corni fructus aqueous extract on kidneys of diabetic mice. Toxicol Res. 2011; 27:37–41.
Article27. Park WH, Hong MY, Chung KH, Kim HM, Lee YC, Kim CH. Effects of traditional herbal medicine, Hwaotang, on atherosclerosis using the spontaneous familial hypercholesterolemia model, Kurosawa and Kusanagi-hypercholesterolemic rabbits and the venous thrombosis rats. Phytother Res. 2005; 19:846–853.
Article28. Lam P, Cheung F, Tan HY, Wang N, Yuen MF, Feng Y. Hepatoprotective effects of Chinese medicinal herbs: a focus on anti-inflammatory and anti-oxidative activities. Int J Mol Sci. 2016; 17:465.
Article29. Hegde SS. Muscarinic receptors in the bladder: from basic research to therapeutics. Br J Pharmacol. 2006; 147:Suppl 2. S80–S87.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Improvement of Persistent Detrusor Overactivity through Treatment with a Phytotherapeutic Agent (WSY-1075) after Relief of Bladder Outlet Obstruction
- Effects of Connexin Expression on Detrusor Overactivity in Male Patients with Bladder Outlet Obstruction Caused by Benign Prostatic Hyperplasia
- Effects of Relief of Bladder Outlet Obstruction on the Detrusor Contractility in Rat
- The Clinical Significance of Detrusor Contraction Duration as a Predicting Parameter for Evaluaing Bladder Outlet Obstruction with Lower Urinary Symptoms in Men
- Bladder Outlet Obstruction in the Female Overactive Bladder: Correct Diagnostic Criteria for Bladder Outlet Obstruction?