Ann Pediatr Endocrinol Metab.
2018 Jun;23(2):88-93. 10.6065/apem.2018.23.2.88.
Thyroid dysfunction in patients with childhood-onset medulloblastoma or primitive neuroectodermal tumor
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. nina337@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2417765
- DOI: http://doi.org/10.6065/apem.2018.23.2.88
Abstract
- PURPOSE
We investigated the clinical characteristics of patients who developed thyroid dysfunction and evaluated the risk factors for hypothyroidism following radiotherapy and chemotherapy in pediatric patients with medulloblastoma or primitive neuroectodermal tumor (PNET).
METHODS
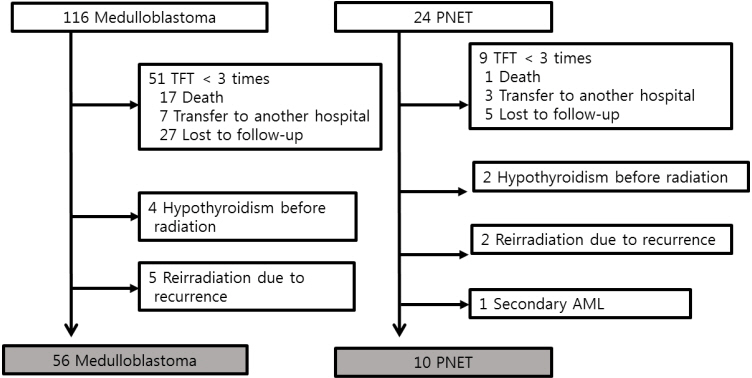
The medical records of 66 patients (42 males) treated for medulloblastoma (n=56) or PNET (n=10) in childhood between January 2000 and December 2014 at Seoul National University Children's Hospital were retrospectively reviewed. A total of 21 patients (18 high-risk medulloblastoma and 3 PNET) underwent high-dose chemotherapy and autologous stem cell rescue (HDCT/ASCR)
RESULTS
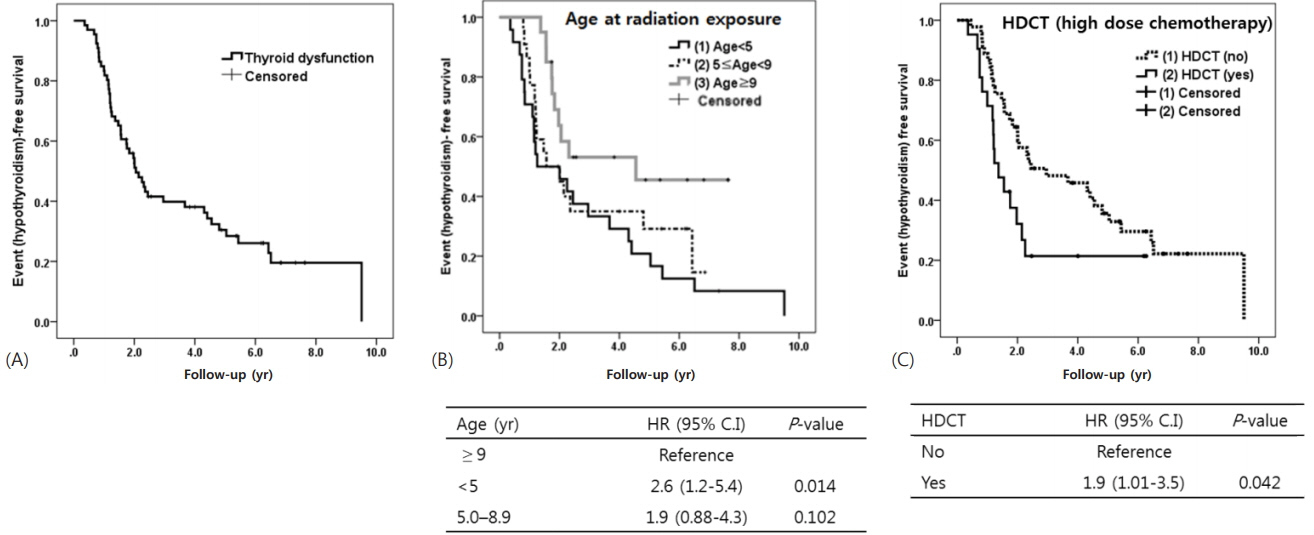
During the median 7.6 years of follow-up, 49 patients (74%) developed transient (n=12) or permanent (n=37) hypothyroidism at a median 3.8 years of follow-up (2.9-4.6 years). Younger age ( < 5 years) at radiation exposure (P=0.014 vs. ≥9 years) and HDCT (P=0.042) were significantly predictive for hypothyroidism based on log-rank test. However, sex, type of tumor, and dose of craniospinal irradiation (less vs. more than 23.4 Gy) were not significant predictors. Cox proportional hazard model showed that both younger age (< 5 years) at radiation exposure (hazard ratio [HR], 3.1; vs. ≥9 years; P=0.004) and HDCT (HR, 2.4; P=0.010) were significant predictors of hypothyroidism.
CONCLUSIONS
Three-quarters of patients with pediatric medulloblastoma or PNET showed thyroid dysfunction, and over half had permanent thyroid dysfunction. Thus, frequent monitoring of thyroid function is mandatory in all patients treated for medulloblastoma or PNET, especially, in very young patients and/or high-risk patients recommended for HDCT/ASCR.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro Oncol. 2016; 18(suppl_5):v1–75.
Article2. Massimino M, Biassoni V, Gandola L, Garrè ML, Gatta G, Giangaspero F, et al. Childhood medulloblastoma. Crit Rev Oncol Hematol. 2016; 105:35–51.
Article3. Packer RJ, Gajjar A, Vezina G, Rorke-Adams L, Burger PC, Robertson PL, et al. Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol. 2006; 24:4202–8.
Article4. Jereczek-Fossa BA, Alterio D, Jassem J, Gibelli B, Tradati N, Orecchia R. Radiotherapy-induced thyroid disorders. Cancer Treat Rev. 2004; 30:369–84.
Article5. Constine LS, Donaldson SS, McDougall IR, Cox RS, Link MP, Kaplan HS. Thyroid dysfunction after radiotherapy in children with Hodgkin's disease. Cancer. 1984; 53:878–83.
Article6. Lee HJ, Hahn SM, Jin SL, Shin YJ, Kim SH, Lee YS, et al. Subclinical hypothyroidism in childhood cancer survivors. Yonsei Med J. 2016; 57:915–22.
Article7. Paulino AC. Hypothyroidism in children with medulloblastoma: a comparison of 3600 and 2340 cGy craniospinal radiotherapy. Int J Radiat Oncol Biol Phys. 2002; 53:543–7.
Article8. Hamnvik OP, Larsen PR, Marqusee E. Thyroid dysfunction from antineoplastic agents. J Natl Cancer Inst. 2011; 103:1572–87.
Article9. Yeung SC, Chiu AC, Vassilopoulou-Sellin R, Gagel RF. The endocrine effects of nonhormonal antineoplastic therapy. Endocr Rev. 1998; 19:144–72.
Article10. Sarkar C, Deb P, Sharma MC. Medulloblastomas: new directions in risk stratification. Neurol India. 2006; 54:16–23.
Article11. Kim H, Kang HJ, Lee JW, Park JD, Park KD, Shin HY, et al. Irinotecan, vincristine, cisplatin, cyclophosphamide, and etoposide for refractory or relapsed edulloblastoma/PNET in pediatric patients. Childs Nerv Syst. 2013; 29:1851–8.
Article12. Park JE, Kang J, Yoo KH, Sung KW, Koo HH, Lim DH, et al. Efficacy of high-dose chemotherapy and autologous stem cell transplantation in patients with relapsed medulloblastoma: a report on the Korean Society for Pediatric Neuro-Oncology (KSPNO)-S-053 study. J Korean Med Sci. 2010; 25:1160–6.
Article13. Shih CS, Hale GA, Gronewold L, Tong X, Laningham FH, Gilger EA, et al. High-dose chemotherapy with autologous stem cell rescue for children with recurrent malignant brain tumors. Cancer. 2008; 112:1345–53.
Article14. Yoon JH, Park KD, Kang HJ, Kim H, Lee JW, Kim SK, et al. Treatment of pediatric average-risk medulloblastoma using craniospinal irradiation less than 2500 cGy and chemotherapy: single center experience in Korea. World J Pediatr. 2017; 13:367–73.
Article15. Clement SC, Schouten-van Meeteren AY, Boot AM, Claahsen-van der Grinten HL, Granzen B, Sen Han K, et al. Prevalence and risk factors of early endocrine disorders in childhood brain tumor survivors: a nationwide, multicenter study. J Clin Oncol. 2016; 34:4362–70.
Article16. Rose SR, Horne VE, Howell J, Lawson SA, Rutter MM, Trotman GE, et al. Late endocrine effects of childhood cancer. Nat Rev Endocrinol. 2016; 12:319–36.
Article17. Saha A, Salley CG, Saigal P, Rolnitzky L, Goldberg J, Scott S, et al. Late effects in survivors of childhood CNS tumors treated on Head Start I and II protocols. Pediatr Blood Cancer. 2014; 61:1644–52.
Article18. Chin D, Sklar C, Donahue B, Uli N, Geneiser N, Allen J, et al. Thyroid dysfunction as a late effect in survivors of pediatric medulloblastoma/primitive neuroectodermal tumors: a comparison of hyperfractionated versus conventional radiotherapy. Cancer. 1997; 80:798–804.
Article19. Yoon IS, Seo JY, Shin CH, Kim IH, Shin HY, Yang SW, Ahn HS. Endocrine dysfunction and growth in children with medulloblastoma. Korean Journal of Pediatrics. 2006; 49:292–7.
Article20. Sobol G, Musioł K, Kalina M, Kalina-Faska B, Mizia-Malarz A, Ficek K, et al. The evaluation of function and the ultrasonographic picture of thyroid in children treated for medulloblastoma. Childs Nerv Syst. 2012; 28:399–404.
Article21. Ogilvy-Stuart AL, Shalet SM, Gattamaneni HR. Thyroid function after treatment of brain tumors in children. J Pediatr. 1991; 119:733–7.
Article22. Massart C, Le Tellier C, Lucas C, Gibassier J, Leclech G, Nicol M. Effects of cisplatin on human thyrocytes in monolayer or follicle culture. J Mol Endocrinol. 1992; 8:243–8.
Article23. Stuart NS, Woodroffe CM, Grundy R, Cullen MH. Longterm toxicity of chemotherapy for testicular cancer--the cost of cure. Br J Cancer. 1990; 61:479–84.
Article24. Torino F, Barnabei A, Paragliola R, Baldelli R, Appetecchia M, Corsello SM. Thyroid dysfunction as an unintended side effect of anticancer drugs. Thyroid. 2013; 23:1345–66.
Article25. Massimino M, Gandola L, Collini P, Seregni E, Marchianò A, Serra A, et al. Thyroid-stimulating hormone suppression for protection against hypothyroidism due to craniospinal irradiation for childhood medulloblastoma/primitive neuroectodermal tumor. Int J Radiat Oncol Biol Phys. 2007; 69:404–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of the Primitive Neuroectodermal Tumors
- Imaging Findings of Atypical Teratoid/Rhabdoid Tumor of Infancy & Childhood in CNS: Report of Two Cases
- Primitive Neuroectodermal Tumor of Mediastinum in an Adult: A Case Report
- A Case of Primitive Neuroectodermal Tumor in the Nasal Cavity
- Primitive neuroectodermal tumor; CT findings