Diabetes Metab J.
2018 Feb;42(1):63-73. 10.4093/dmj.2018.42.1.63.
Color Doppler Ultrasonography Is a Useful Tool for Diagnosis of Peripheral Artery Disease in Type 2 Diabetes Mellitus Patients with Ankle-Brachial Index 0.91 to 1.40
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Huh's Diabetes Center and 21st Century Diabetes and Vascular Research Institute, Seoul, Korea.
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
- 5Department of Internal Medicine, CHA University School of Medicine, Seongnam, Korea.
- 6Department of Epidemiology and Health Promotion, Institute for Health Promotion, Yonsei University Graduate School of Public Health, Seoul, Korea.
- 7Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. drshchoi@snu.ac.kr
- KMID: 2409187
- DOI: http://doi.org/10.4093/dmj.2018.42.1.63
Abstract
- BACKGROUND
The clinical utility of ankle-brachial index (ABI) is not clear in subjects with less severe or calcified vessel. Therefore, we investigated the usefulness of color Doppler ultrasonography for diagnosing peripheral artery disease (PAD) in type 2 diabetes mellitus (T2DM) subjects.
METHODS
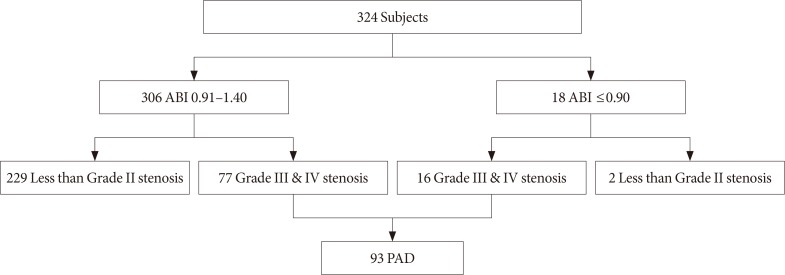
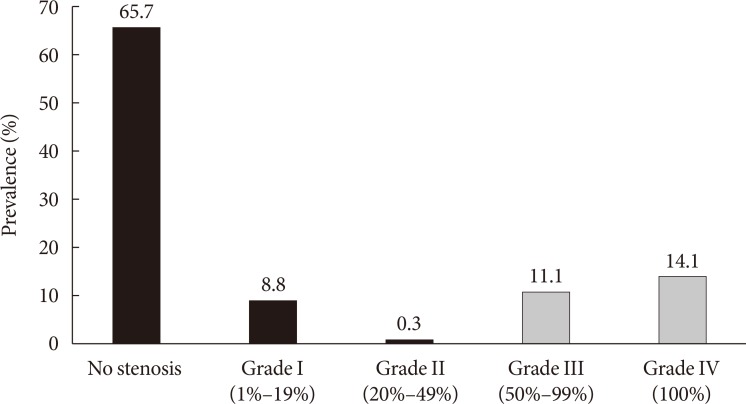
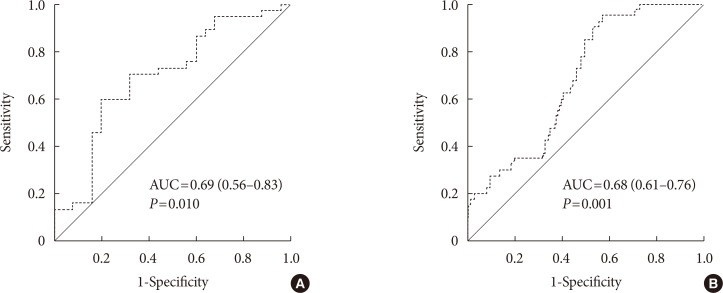
We analyzed 324 T2DM patients who concurrently underwent ABI and carotid intima-media thickness (CIMT) measurements and color Doppler ultrasonography from 2003 to 2006. The degree of stenosis in patients with PAD was determined according to Jager's criteria, and PAD was defined as grade III (50% to 99% stenosis) or IV stenosis (100% stenosis) by color Doppler ultrasonography. Logistic regression analysis and receiver operating characteristic curve analysis were performed to evaluate the risk factors for PAD in patients with ABI 0.91 to 1.40.
RESULTS
Among the 324 patients, 77 (23.8%) had ABI 0.91 to 1.40 but were diagnosed with PAD. Color Doppler ultrasonography demonstrated that suprapopliteal arterial stenosis, bilateral lesions, and multivessel involvement were less common in PAD patients with ABI 0.91 to 1.40 than in those with ABI ≤0.90. A multivariate logistic regression analysis demonstrated that older age, current smoking status, presence of leg symptoms, and high CIMT were significantly associated with the presence of PAD in patients with ABI 0.91 to 1.40 after adjusting for conventional risk factors. CIMT showed significant power in predicting the presence of PAD in patients with ABI 0.91 to 1.40.
CONCLUSION
Color Doppler ultrasonography is a useful tool for the detection of PAD in T2DM patients with ABI 0.91 to 1.40 but a high CIMT.
Keyword
MeSH Terms
Figure
Reference
-
1. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004; 110:738–743. PMID: 15262830.
Article2. Eraso LH, Fukaya E, Mohler ER 3rd, Xie D, Sha D, Berger JS. Peripheral arterial disease, prevalence and cumulative risk factor profile analysis. Eur J Prev Cardiol. 2014; 21:704–711. PMID: 22739687.
Article3. Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015; 116:1509–1526. PMID: 25908725.
Article4. Sigvant B, Hasvold P, Kragsterman B, Falkenberg M, Johansson S, Thuresson M, Nordanstig J. Cardiovascular outcomes in patients with peripheral arterial disease as an initial or subsequent manifestation of atherosclerotic disease: results from a Swedish nationwide study. J Vasc Surg. 2017; 66:507–514. PMID: 28433332.5. Olin JW, Sealove BA. Peripheral artery disease: current insight into the disease and its diagnosis and management. Mayo Clin Proc. 2010; 85:678–692. PMID: 20592174.
Article6. Gregg EW, Sorlie P, Paulose-Ram R, Gu Q, Eberhardt MS, Wolz M, Burt V, Curtin L, Engelgau M, Geiss L. 1999-2000 national health and nutrition examination survey. Prevalence of lower-extremity disease in the US adult population >=40 years of age with and without diabetes: 1999-2000 national health and nutrition examination survey. Diabetes Care. 2004; 27:1591–1597. PMID: 15220233.7. Shammas AN, Jeon-Slaughter H, Tsai S, Khalili H, Ali M, Xu H, Rodriguez G, Cawich I, Armstrong EJ, Brilakis ES, Banerjee S. Major limb outcomes following lower extremity endovascular revascularization in patients with and without diabetes mellitus. J Endovasc Ther. 2017; 24:376–382. PMID: 28440113.
Article8. Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Rother J, Wilson PW. REACH Registry Investigators. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006; 295:180–189. PMID: 16403930.
Article9. American Diabetes Association. 10. Microvascular complications and foot care: standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S105–S118. PMID: 29222381.10. Dhaliwal G, Mukherjee D. Peripheral arterial disease: epidemiology, natural history, diagnosis and treatment. Int J Angiol. 2007; 16:36–44. PMID: 22477268.
Article11. American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003; 26:3333–3341. PMID: 14633825.12. Khan NA, Rahim SA, Anand SS, Simel DL, Panju A. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006; 295:536–546. PMID: 16449619.
Article13. Sibal L, Agarwal SC, Home PD. Carotid intima-media thickness as a surrogate marker of cardiovascular disease in diabetes. Diabetes Metab Syndr Obes. 2011; 4:23–34. PMID: 21448319.
Article14. Bots ML, Hofman A, Grobbee DE. Common carotid intima-media thickness and lower extremity arterial atherosclerosis. The Rotterdam Study. Arterioscler Thromb. 1994; 14:1885–1891. PMID: 7981175.
Article15. Poredos P, Golob M, Jensterle M. Interrelationship between peripheral arterial occlusive disease, carotid atherosclerosis and flow mediated dilation of the brachial artery. Int Angiol. 2003; 22:83–87. PMID: 12771862.16. Borssen B, Bergenheim T, Lithner F. The epidemiology of foot lesions in diabetic patients aged 15–50 years. Diabet Med. 1990; 7:438–444. PMID: 2142042.17. Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FG, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RA, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, Walsh ME. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017; 135:e686–e725. PMID: 27840332.
Article18. Jager KA, Phillips DJ, Martin RL, Hanson C, Roederer GO, Langlois YE, Ricketts HJ, Strandness DE Jr. Noninvasive mapping of lower limb arterial lesions. Ultrasound Med Biol. 1985; 11:515–521. PMID: 2931880.
Article19. Jun JE, Choi YJ, Lee YH, Kim DJ, Park SW, Huh BW, Lee EJ, Jee SH, Hur KY, Choi SH, Huh KB. ApoB/ApoA-I ratio is independently associated with carotid atherosclerosis in type 2 diabetes mellitus with well-controlled LDL cholesterol levels. Korean J Intern Med. 2018; 33:138–147. PMID: 29334727.
Article20. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, Csiba L, Desvarieux M, Ebrahim S, Hernandez Hernandez R, Jaff M, Kownator S, Naqvi T, Prati P, Rundek T, Sitzer M, Schminke U, Tardif JC, Taylor A, Vicaut E, Woo KS. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012; 34:290–296. PMID: 23128470.21. Park SW, Kim SK, Cho YW, Kim DJ, Song YD, Choi YJ, Huh BW, Choi SH, Jee SH, Cho MA, Lee EJ, Huh KB. Insulin resistance and carotid atherosclerosis in patients with type 2 diabetes. Atherosclerosis. 2009; 205:309–313. PMID: 19147142.
Article22. Walters DP, Gatling W, Mullee MA, Hill RD. The prevalence, detection, and epidemiological correlates of peripheral vascular disease: a comparison of diabetic and non-diabetic subjects in an English community. Diabet Med. 1992; 9:710–715. PMID: 1395462.
Article23. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001; 286:1317–1324. PMID: 11560536.
Article24. Rhee SY, Guan H, Liu ZM, Cheng SW, Waspadji S, Palmes P, Tai TY, Suwanwalaikorn S, Kim YS. PAD-SEARCH Study Group. Multi-country study on the prevalence and clinical features of peripheral arterial disease in Asian type 2 diabetes patients at high risk of atherosclerosis. Diabetes Res Clin Pract. 2007; 76:82–92. PMID: 16950543.
Article25. Ghosh US, Datta S, Banerjee S. Asymptomatic peripheral arterial disease in type 2 diabetes mellitus: prevalence patterns and risk factor associations. Int J Diabetes Dev Ctries. 2011; 31:229–238.
Article26. Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, Sackett DL, Strandness DE Jr, Taylor LM. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a critical review. Circulation. 1996; 94:3026–3049. PMID: 8941154.
Article27. Antonopoulos S, Kokkoris S, Stasini F, Mylonopoulou M, Lepeniotis G, Mikros S, Korantzopoulos P, Giannoulis G. High prevalence of subclinical peripheral artery disease in Greek hospitalized patients. Eur J Intern Med. 2005; 16:187–191. PMID: 15967334.
Article28. Natsuaki C, Inoguchi T, Maeda Y, Yamada T, Sasaki S, Sonoda N, Shimabukuro M, Nawata H, Takayanagi R. Association of borderline ankle-brachial index with mortality and the incidence of peripheral artery disease in diabetic patients. Atherosclerosis. 2014; 234:360–365. PMID: 24732575.
Article29. Kajikawa M, Maruhashi T, Iwamoto Y, Iwamoto A, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Nakashima A, Goto C, Noma K, Higashi Y. Borderline ankle-brachial index value of 0.91–0.99 is associated with endothelial dysfunction. Circ J. 2014; 78:1740–1745. PMID: 24813179.
Article30. Tanaka S, Kaneko H, Kano H, Matsuno S, Suzuki S, Takai H, Otsuka T, Uejima T, Oikawa Y, Nagashima K, Kirigaya H, Sagara K, Yajima J, Sawada H, Aizawa T, Yamashita T. The predictive value of the borderline ankle-brachial index for long-term clinical outcomes: an observational cohort study. Atherosclerosis. 2016; 250:69–76. PMID: 27182960.
Article31. Ovbiagele B. Association of ankle-brachial index level with stroke. J Neurol Sci. 2009; 276:14–17. PMID: 18804220.
Article32. de Vries M, Ouwendijk R, Flobbe K, Nelemans PJ, Kessels AG, Schurink GH, van der Vliet JA, Heijstraten FM, Cuypers PW, Duijm LE, van Engelshoven JM, Hunink MG, de Haan MW. Peripheral arterial disease: clinical and cost comparisons between duplex US and contrast-enhanced MR angiography. A multicenter randomized trial. Radiology. 2006; 240:401–410. PMID: 16864668.33. Collins R, Burch J, Cranny G, Aguiar-Ibanez R, Craig D, Wright K, Berry E, Gough M, Kleijnen J, Westwood M. Duplex ultrasonography, magnetic resonance angiography, and computed tomography angiography for diagnosis and assessment of symptomatic, lower limb peripheral arterial disease: systematic review. BMJ. 2007; 334:1257. PMID: 17548364.
Article34. Bembi V, Singh S, Singh P, Aneja GK, Arya TV, Arora R. Prevalence of peripheral arterial disease in a cohort of diabetic patients. South Med J. 2006; 99:564–569. PMID: 16800410.
Article35. Lundberg C, Hansen T, Ahlstrom H, Lind L, Wikstrom J, Johansson L. The relationship between carotid intima-media thickness and global atherosclerosis. Clin Physiol Funct Imaging. 2014; 34:457–462. PMID: 24405735.
Article36. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007; 115:459–467. PMID: 17242284.37. Pradeepa R, Chella S, Surendar J, Indulekha K, Anjana RM, Mohan V. Prevalence of peripheral vascular disease and its association with carotid intima-media thickness and arterial stiffness in type 2 diabetes: the Chennai urban rural epidemiology study (CURES 111). Diab Vasc Dis Res. 2014; 11:190–200. PMID: 24627461.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Peripheral Artery Disease: Focus on the 2016 American Heart Association/American College of Cardiology and 2017 European Society of Cardiology Guidelines
- False Normalization of Ankle Brachial Index: A Case of Lower Extremity Peripheral Arterial Disease with Normal Ankle-Brachial Index
- Association between Aging and Changes in the Ankle-Brachial Index after Exercise in Patients with Chest Pain
- The Association between Albuminuria and Peripheral Arterial Disease in Patients with Type 2 Diabetes Mellitus
- Doppler ultrasonography of the lower extremity arteries: anatomy and scanning guidelines