Korean Circ J.
2017 Nov;47(6):918-928. 10.4070/kcj.2016.0443.
Prognostic Application of Thoracic Aortic Calcium Scoring for Adverse Clinical Outcome Risk in Elderly Patients with Left Ventricular Hypertrophy
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. hjchang@yuhs.ac
- 2Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2396485
- DOI: http://doi.org/10.4070/kcj.2016.0443
Abstract
- BACKGROUND AND OBJECTIVES
Left ventricular hypertrophy (LVH) is associated with poor cardiovascular outcomes. Heavy aortic calcification exacerbates arterial stiffness, which consequently heightens left ventricular (LV) afterload. We assessed the usefulness of aortic calcification for predicting adverse cardiovascular outcomes and to determine whether the relationship, if any, differed as a function of LVH.
METHODS
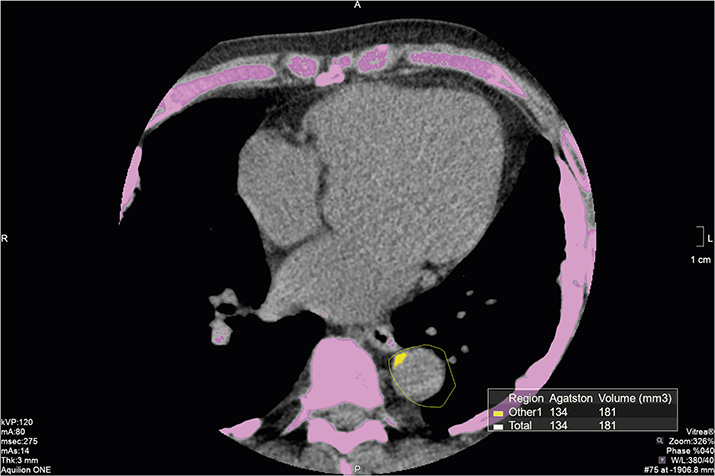
The analytic sample was comprised of a total of 487 individuals 65 years of age or older. Thoracic aorta calcium score (TACS) was measured by coronary computed tomography, and patients were stratified according to the median (TACS, 446 mm3). LVH obtained from echocardiography was defined as LV mass index >115 g/m2 for men and >95 g/m2 for women. Cox regression reporting hazard ratios (HRs) with 95% confidence intervals (CIs) was performed to predict the risk for the composite study endpoint, defined as cardiac death, admission for heart failure, obstructive coronary artery disease (CAD) requiring revascularization, or stroke.
RESULTS
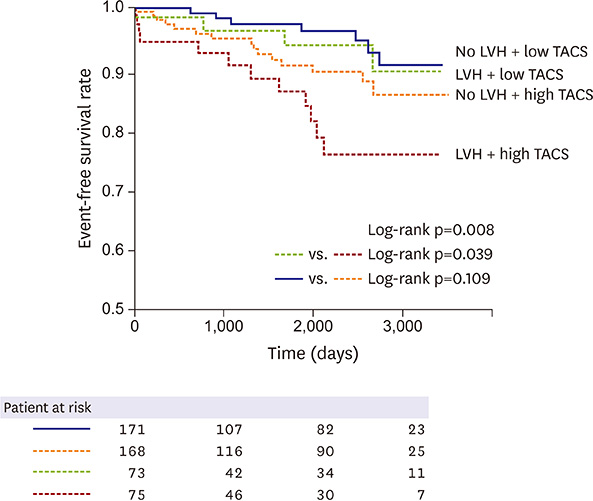
A total of 39 composite events (8.0%) occurred during a median follow-up of 65 months (interquartile range [IQR], 17-89 months). For those with LVH, the concurrent presence of high TACS appeared to be an independent predictor (HR, 4.51; 95% CI, 1.71-11.88; p=0.002) for the composite study endpoint. Other combined LVH and TACS subgroups were not associated with significant factors for predicting the composite study endpoint (p>0.050, all).
CONCLUSION
TACS provides robust predictive utility for a composite of cardiovascular events and cardiac death in persons with LVH. This finding was less pronounced in those with a relatively healthy myocardium, defined by the absence of LVH.
MeSH Terms
Figure
Cited by 1 articles
-
Vascular Calcification in Chronic Kidney Disease: Distinct Features of Pathogenesis and Clinical Implication
Jin Sug Kim, Hyeon Seok Hwang
Korean Circ J. 2021;51(12):961-982. doi: 10.4070/kcj.2021.0995.
Reference
-
1. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990; 322:1561–1566.2. Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension. 2000; 35:580–586.3. Sundström J, Lind L, Arnlöv J, Zethelius B, Andrén B, Lithell HO. Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation. 2001; 103:2346–2351.4. Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000; 35:569–582.5. Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015; 29:1–6.6. Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013; 62:263–271.7. Eisen A, Tenenbaum A, Koren-Morag N, et al. Calcification of the thoracic aorta as detected by spiral computed tomography among stable angina pectoris patients: association with cardiovascular events and death. Circulation. 2008; 118:1328–1334.8. Wong ND, Gransar H, Shaw L, et al. Thoracic aortic calcium versus coronary artery calcium for the prediction of coronary heart disease and cardiovascular disease events. JACC Cardiovasc Imaging. 2009; 2:319–326.9. Cho IJ, Chang HJ, Park HB, et al. Aortic calcification is associated with arterial stiffening, left ventricular hypertrophy, and diastolic dysfunction in elderly male patients with hypertension. J Hypertens. 2015; 33:1633–1641.10. Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol. 2002; 40:1531–1540.11. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997; 30:260–311.12. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.13. Frohlich ED, Susic D. Pressure overload. Heart Fail Clin. 2012; 8:21–32.14. Ruilope LM, Schmieder RE. Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens. 2008; 21:500–508.15. Arnett DK, de las Fuentes L, Broeckel U. Genes for left ventricular hypertrophy. Curr Hypertens Rep. 2004; 6:36–41.16. de Simone G, Izzo R, De Luca N, Gerdts E. Left ventricular geometry in obesity: is it what we expect? Nutr Metab Cardiovasc Dis. 2013; 23:905–912.17. Cacciapuoti F. Molecular mechanisms of left ventricular hypertrophy (LVH) in systemic hypertension (SH)-possible therapeutic perspectives. J Am Soc Hypertens. 2011; 5:449–455.18. Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstitium. Fibrosis and renin-angiotensin-aldosterone system. Circulation. 1991; 83:1849–1865.19. Eren M, Gorgulu S, Uslu N, Celik S, Dagdeviren B, Tezel T. Relation between aortic stiffness and left ventricular diastolic function in patients with hypertension, diabetes, or both. Heart. 2004; 90:37–43.20. Tsioufis C, Chatzis D, Dimitriadis K, et al. Left ventricular diastolic dysfunction is accompanied by increased aortic stiffness in the early stages of essential hypertension: a TDI approach. J Hypertens. 2005; 23:1745–1750.21. Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation. 2003; 107:714–720.22. Kim J, Budoff MJ, Nasir K, et al. Thoracic aortic calcium, cardiovascular disease events, and all-cause mortality in asymptomatic individuals with zero coronary calcium: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2017; 257:1–8.23. Kim HK, Kim YJ, Hwang SJ, et al. Hemodynamic and prognostic implications of net atrioventricular compliance in patients with mitral stenosis. J Am Soc Echocardiogr. 2008; 21:482–486.24. Kim TJ, Han DH, Jin KN, Won Lee K. Lung cancer detected at cardiac CT: prevalence, clinicoradiologic features, and importance of full-field-of-view images. Radiology. 2010; 255:369–376.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abnormal Motion of Left Ventricular Posterior Wall and Aortic Root Posterior Wall in Patients with Left Ventricular Hypertrophy: An Echocardiographic Study
- Correlation of Complex Ventricular Arrhythmias with Left Ventricular Hypertrophy and Their Prognostic Significances
- Electrocardiographic Diagnosis of Left Ventricular Hypertrophy by Scoring System
- The Evaluation of Minnesota Code in Electrocardioraphic Diagnosis of Ventricular Hypertrophy
- Left ventricular muscle mass regression after aortic valve replacement