Diabetes Metab J.
2017 Apr;41(2):113-120. 10.4093/dmj.2017.41.2.113.
Association between Blood Mercury Level and Visceral Adiposity in Adults
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Yonsei University College of Medicine, Seoul, Korea.
- 2Cardiovascular and Metabolic Disease Etiology Research Center, Ajou University School of Medicine, Suwon, Korea. djkim@ajou.ac.kr
- 3Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
- 4Department of Epidemiology and Biostatistics, Indiana University Bloomington School of Public Health, Bloomington, IN, USA.
- KMID: 2376773
- DOI: http://doi.org/10.4093/dmj.2017.41.2.113
Abstract
- BACKGROUND
Few studies have examined the association between mercury exposure and obesity. The aim of this study is to investigate the association between blood mercury concentrations and indices of obesity in adults.
METHODS
A total of 200 healthy subjects, aged 30 to 64 years, who had no history of cardiovascular or malignant disease, were examined. Anthropometric and various biochemical profiles were measured. Visceral adipose tissue (VAT) was measured using dual-energy X-ray absorptiometry (DXA).
RESULTS
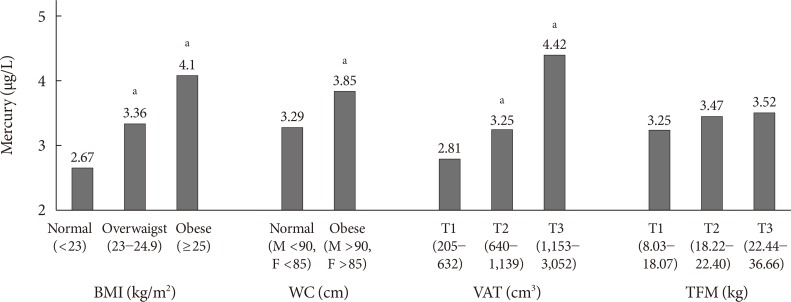
All subjects were divided into three groups according to blood mercury concentrations. Compared with the subjects in the lowest tertile of mercury, those in the highest tertile were more likely to be male; were current alcohol drinkers and smokers; had a higher body mass index (BMI), waist circumference (WC), and VAT; had higher levels of blood pressure, fasting glucose, and insulin resistance; and consumed more fish. The blood mercury concentration was significantly associated with anthropometric parameters, showing relationships with BMI, WC, and VAT. After adjusting for multiple risk factors, the odds ratios (ORs) for high mercury concentration was significantly higher in the highest VAT tertile than in the lowest VAT tertile (OR, 2.66; 95% confidence interval, 1.05 to 6.62; P<0.05).
CONCLUSION
The blood mercury concentration was significantly associated with VAT in healthy adults. Further studies are warranted to confirm our findings.
MeSH Terms
Figure
Cited by 1 articles
-
Cohort Profile: The Cardiovascular and Metabolic Diseases Etiology Research Center Cohort in Korea
Jee-Seon Shim, Bo Mi Song, Jung Hyun Lee, Seung Won Lee, Ji Hye Park, Dong Phil Choi, Myung Ha Lee, Kyoung Hwa Ha, Dae Jung Kim, Sungha Park, Won-Woo Lee, Yoosik Youm, Eui-Cheol Shin, Hyeon Chang Kim
Yonsei Med J. 2019;60(8):804-810. doi: 10.3349/ymj.2019.60.8.804.
Reference
-
1. Houston MC. Role of mercury toxicity in hypertension, cardiovascular disease, and stroke. J Clin Hypertens (Greenwich). 2011; 13:621–627. PMID: 21806773.
Article2. He K, Xun P, Liu K, Morris S, Reis J, Guallar E. Mercury exposure in young adulthood and incidence of diabetes later in life: the CARDIA Trace Element Study. Diabetes Care. 2013; 36:1584–1589. PMID: 23423697.3. Sargis RM. The hijacking of cellular signaling and the diabetes epidemic: mechanisms of environmental disruption of insulin action and glucose homeostasis. Diabetes Metab J. 2014; 38:13–24. PMID: 24627823.
Article4. Eom SY, Choi SH, Ahn SJ, Kim DK, Kim DW, Lim JA, Choi BS, Shin HJ, Yun SW, Yoon HJ, Kim YM, Hong YS, Yun YW, Sohn SJ, Kim H, Park KS, Pyo HS, Kim H, Oh SY, Kim J, Lee SA, Ha M, Kwon HJ, Park JD. Reference levels of blood mercury and association with metabolic syndrome in Korean adults. Int Arch Occup Environ Health. 2014; 87:501–513. PMID: 23824410.
Article5. Kim YN, Kim YA, Yang AR, Lee BH. Relationship between blood mercury level and risk of cardiovascular diseases: results from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV) 2008-2009. Prev Nutr Food Sci. 2014; 19:333–342. PMID: 25580399.
Article6. Futatsuka M, Kitano T, Wakamiya J. An epidemiological study on diabetes mellitus in the population living in a methyl mercury polluted area. J Epidemiol. 1996; 6:204–208. PMID: 9002387.
Article7. Yoshizawa K, Rimm EB, Morris JS, Spate VL, Hsieh CC, Spiegelman D, Stampfer MJ, Willett WC. Mercury and the risk of coronary heart disease in men. N Engl J Med. 2002; 347:1755–1760. PMID: 12456851.
Article8. Lee BK, Kim Y. Blood cadmium, mercury, and lead and metabolic syndrome in South Korea: 2005-2010 Korean National Health and Nutrition Examination Survey. Am J Ind Med. 2013; 56:682–692. PMID: 22911659.
Article9. Rhee SY, Hwang YC, Woo JT, Sinn DH, Chin SO, Chon S, Kim YS. Blood lead is significantly associated with metabolic syndrome in Korean adults: an analysis based on the Korea National Health and Nutrition Examination Survey (KNHANES), 2008. Cardiovasc Diabetol. 2013; 12:9. PMID: 23302150.
Article10. Moon SS. Additive effect of heavy metals on metabolic syndrome in the Korean population: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009-2010. Endocrine. 2014; 46:263–271. PMID: 24065312.
Article11. Vahter ME, Mottet NK, Friberg LT, Lind SB, Charleston JS, Burbacher TM. Demethylation of methyl mercury in different brain sites of Macaca fascicularis monkeys during long-term subclinical methyl mercury exposure. Toxicol Appl Pharmacol. 1995; 134:273–284. PMID: 7570604.12. Yamamoto M, Yanagisawa R, Motomura E, Nakamura M, Sakamoto M, Takeya M, Eto K. Increased methylmercury toxicity related to obesity in diabetic KK-Ay mice. J Appl Toxicol. 2014; 34:914–923. PMID: 24243536.
Article13. Rothenberg SE, Korrick SA, Fayad R. The influence of obesity on blood mercury levels for U.S. non-pregnant adults and children: NHANES 2007-2010. Environ Res. 2015; 138:173–180. PMID: 25721244.
Article14. Lin H, Yan H, Rao S, Xia M, Zhou Q, Xu H, Rothney MP, Xia Y, Wacker WK, Ergun DL, Zeng M, Gao X. Quantification of visceral adipose tissue using lunar dual-energy X-ray absorptiometry in Asian Chinese. Obesity (Silver Spring). 2013; 21:2112–2117. PMID: 23418061.
Article15. Rothney MP, Catapano AL, Xia J, Wacker WK, Tidone C, Grigore L, Xia Y, Ergun DL. Abdominal visceral fat measurement using dual-energy X-ray: association with cardiometabolic risk factors. Obesity (Silver Spring). 2013; 21:1798–1802. PMID: 23696250.
Article16. Kaul S, Rothney MP, Peters DM, Wacker WK, Davis CE, Shapiro MD, Ergun DL. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring). 2012; 20:1313–1318. PMID: 22282048.
Article17. Kim HJ, Kim YG, Park JS, Ahn YH, Ha KH, Kim DJ. Association between blood glucose level derived using the oral glucose tolerance test and glycated hemoglobin level. Korean J Intern Med. 2016; 31:535–542. PMID: 26898598.
Article18. Yun SH, Shim JS, Kweon S, Oh K. Development of a food frequency questionnaire for the Korea National Health and Nutrition Examination Survey: data from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV). Korean J Nutr. 2013; 46:186–196.
Article19. Lee S, Park HS, Kim SM, Kwon HS, Kim DY, Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, Oh SJ, Lee CB, Kim KS, Oh SW, Kim YS, Choi WH, Yoo HJ. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J Obes. 2006; 15:1–9.20. Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998; 21:2191–2192. PMID: 9839117.
Article21. Schulz C, Angerer J, Ewers U, Kolossa-Gehring M. The German human biomonitoring commission. Int J Hyg Environ Health. 2007; 210:373–382. PMID: 17337242.
Article22. Gallagher CM, Meliker JR. Blood and urine cadmium, blood pressure, and hypertension: a systematic review and meta-analysis. Environ Health Perspect. 2010; 118:1676–1684. PMID: 20716508.
Article23. Park S, Lee BK. Body fat percentage and hemoglobin levels are related to blood lead, cadmium, and mercury concentrations in a Korean adult population (KNHANES 2008-2010). Biol Trace Elem Res. 2013; 151:315–323. PMID: 23238610.
Article24. Mortensen ME, Caudill SP, Caldwell KL, Ward CD, Jones RL. Total and methyl mercury in whole blood measured for the first time in the U.S. population: NHANES 2011-2012. Environ Res. 2014; 134:257–264. PMID: 25173092.
Article25. Kim NS, Lee BK. National estimates of blood lead, cadmium, and mercury levels in the Korean general adult population. Int Arch Occup Environ Health. 2011; 84:53–63. PMID: 20198383.
Article26. Cho S, Jacobs DR Jr, Park K. Population correlates of circulating mercury levels in Korean adults: the Korea National Health and Nutrition Examination Survey IV. BMC Public Health. 2014; 14:527. PMID: 24884916.
Article27. Mahaffey KR, Clickner RP, Bodurow CC. Blood organic mercury and dietary mercury intake: National Health and Nutrition Examination Survey, 1999 and 2000. Environ Health Perspect. 2004; 112:562–570. PMID: 15064162.
Article28. Caldwell KL, Mortensen ME, Jones RL, Caudill SP, Osterloh JD. Total blood mercury concentrations in the U.S. population: 1999-2006. Int J Hyg Environ Health. 2009; 212:588–598. PMID: 19481974.
Article29. Wong SL, Lye EJ. Lead, mercury and cadmium levels in Canadians. Health Rep. 2008; 19:31–36.30. Lincoln RA, Shine JP, Chesney EJ, Vorhees DJ, Grandjean P, Senn DB. Fish consumption and mercury exposure among Louisiana recreational anglers. Environ Health Perspect. 2011; 119:245–251. PMID: 20980220.
Article31. Mahaffey KR, Clickner RP, Jeffries RA. Adult women's blood mercury concentrations vary regionally in the United States: association with patterns of fish consumption (NHANES 1999-2004). Environ Health Perspect. 2009; 117:47–53. PMID: 19165386.
Article32. Smith KM, Barraj LM, Kantor M, Sahyoun NR. Relationship between fish intake, n-3 fatty acids, mercury and risk markers of CHD (National Health and Nutrition Examination Survey 1999-2002). Public Health Nutr. 2009; 12:1261–1269. PMID: 18986590.
Article33. You CH, Kim BG, Kim JM, Yu SD, Kim YM, Kim RB, Hong YS. Relationship between blood mercury concentration and waist-to-hip ratio in elderly Korean individuals living in coastal areas. J Prev Med Public Health. 2011; 44:218–225. PMID: 22020187.
Article34. Kim KN, Park SJ, Choi B, Joo NS. Blood mercury and insulin resistance in nondiabetic Koreans (KNHANES 2008-2010). Yonsei Med J. 2015; 56:944–950. PMID: 26069115.
Article35. Chang JW, Chen HL, Su HJ, Liao PC, Guo HR, Lee CC. Simultaneous exposure of non-diabetics to high levels of dioxins and mercury increases their risk of insulin resistance. J Hazard Mater. 2011; 185:749–755. PMID: 21087821.
Article36. Barbosa AC, Jardim W, Dórea JG, Fosberg B, Souza J. Hair mercury speciation as a function of gender, age, and body mass index in inhabitants of the Negro River basin, Amazon, Brazil. Arch Environ Contam Toxicol. 2001; 40:439–444. PMID: 11443378.37. Bae S, Park SJ, Yeum KJ, Choi B, Kim YS, Joo NS. Cut-off values of blood mercury concentration in relation to increased body mass index and waist circumference in Koreans. J Investig Med. 2016; 64:867–871.
Article38. Kawakami T, Hanao N, Nishiyama K, Kadota Y, Inoue M, Sato M, Suzuki S. Differential effects of cobalt and mercury on lipid metabolism in the white adipose tissue of high-fat diet-induced obesity mice. Toxicol Appl Pharmacol. 2012; 258:32–42. PMID: 22019852.
Article39. Xuehui C. Accumulation of heavy metals and organochlorine pesticides in human milk and adipose tissues, and its health concerns [master's thesis]. Hong Kong: Hong Kong Baptist University;2007.40. Qin YY, Leung CK, Leung AO, Wu SC, Zheng JS, Wong MH. Persistent organic pollutants and heavy metals in adipose tissues of patients with uterine leiomyomas and the association of these pollutants with seafood diet, BMI, and age. Environ Sci Pollut Res. 2010; 17:229–240.
Article41. Brzoska MM, Moniuszko-Jakoniuk J. Interactions between cadmium and zinc in the organism. Food Chem Toxicol. 2001; 39:967–980. PMID: 11524135.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Blood Mercury Level and Visceral Adiposity in Adults
- The Effect of Fish Consumption on Blood Mercury Levels of Pregnant Women
- Association between Low-level Mercury Exposure and Neurobehavioral Functions in Korean Adults Living in a Coastal City
- The effect of fish consumption on blood mercury level in pregnant women
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults