Yonsei Med J.
2017 Jan;58(1):75-81. 10.3349/ymj.2017.58.1.75.
The Impact of Diabetes Mellitus on Vascular Biomarkers in Patients with End-Stage Renal Disease
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Gachon University of Medicine and Science, Incheon, Korea.
- 2Division of Cardiology, Severance Cardiovascular Hospital and Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea. shpark0530@yuhs.ac
- 3Division of Nephrology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. yoosy0316@yuhs.ac
- KMID: 2374191
- DOI: http://doi.org/10.3349/ymj.2017.58.1.75
Abstract
- PURPOSE
Diabetes mellitus (DM) is the most common cause of end-stage renal disease (ESRD) and an important risk factor for cardiovascular (CV) disease. We investigated the impact of DM on subclinical CV damage by comprehensive screening protocol in ESRD patients.
MATERIALS AND METHODS
Echocardiography, coronary computed tomography angiogram, 24-h ambulatory blood pressure monitoring, and central blood pressure with pulse wave velocity (PWV) were performed in 91 ESRD patients from the Cardiovascular and Metabolic disease Etiology Research Center-HIgh risk cohort.
RESULTS
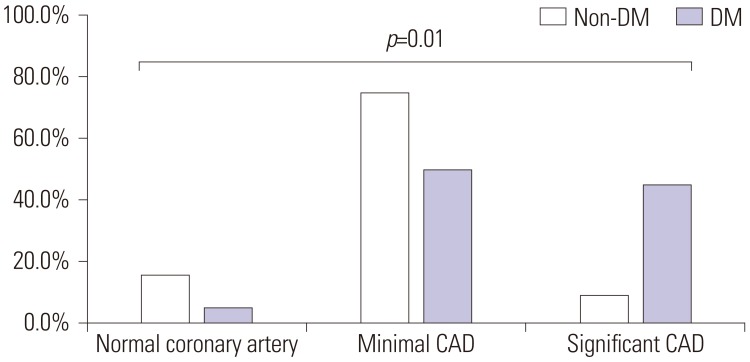
The DM group (n=38) had higher systolic blood pressure than the non-DM group (n=53), however, other clinical CV risk factors were not different between two groups. Central aortic systolic pressure (148.7±29.8 mm Hg vs. 133.7±27.0 mm Hg, p= 0.014), PWV (12.1±2.7 m/s vs. 9.4±2.1 m/s, p<0.001), and early mitral inflow to early mitral annulus velocity (16.7±6.4 vs. 13.7±5.9, p=0.026) were higher in the DM group. Although the prevalence of coronary artery disease (CAD) was not different between the DM and the non-DM group (95% vs. 84.4%, p=0.471), the severity of CAD was higher in the DM group (p=0.01). In multivariate regression analysis, DM was an independent determinant for central systolic pressure (p=0.011), PWV (p<0.001) and the prevalence of CAD (p=0.046).
CONCLUSION
Diabetic ESRD patients have higher central systolic pressure and more advanced arteriosclerosis than the non-DM control group. These findings suggest that screening for subclinical CV damage may be helpful for diabetic ESRD patients.
Keyword
MeSH Terms
-
Aged
Aorta
Biomarkers
Blood Pressure/physiology
Blood Pressure Monitoring, Ambulatory
Coronary Artery Disease/diagnostic imaging/*physiopathology
Diabetes Mellitus/*physiopathology
Diabetic Nephropathies/physiopathology
Echocardiography
Female
Humans
Kidney Failure, Chronic/*physiopathology
Male
Middle Aged
Pulse Wave Analysis
Regression Analysis
Risk Factors
Systole/physiology
Biomarkers
Figure
Reference
-
1. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004; 351:1296–1305. PMID: 15385656.
Article2. Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998; 339:799–805. PMID: 9738087.
Article3. Ritz E, Rychlík I, Locatelli F, Halimi S. End-stage renal failure in type 2 diabetes: a medical catastrophe of worldwide dimensions. Am J Kidney Dis. 1999; 34:795–808. PMID: 10561134.
Article4. Weber T, Auer J, O’Rourke MF, Kvas E, Lassnig E, Berent R, et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004; 109:184–189. PMID: 14662706.
Article5. Weber T, O’Rourke MF, Ammer M, Kvas E, Punzengruber C, Eber B. Arterial stiffness and arterial wave reflections are associated with systolic and diastolic function in patients with normal ejection fraction. Am J Hypertens. 2008; 21:1194–1202. PMID: 18787521.
Article6. Rajzer MW, Wojciechowska W, Klocek M, Palka I, Brzozowska-Kiszka M, Kawecka-Jaszcz K. Comparison of aortic pulse wave velocity measured by three techniques: Complior, SphygmoCor and Arteriograph. J Hypertens. 2008; 26:2001–2007. PMID: 18806624.
Article7. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463. PMID: 16376782.
Article8. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133. PMID: 19187853.
Article9. Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006; 48:1475–1497. PMID: 17010819.10. American College of Cardiology Foundation Task Force on Expert Consensus Documents. Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010; 121:2509–2543. PMID: 20479158.11. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51(4 Suppl):5–40. PMID: 1116248.
Article12. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832. PMID: 2407762.
Article13. Nakazato R, Dey D, Gutstein A, Le Meunier L, Cheng VY, Pimentel R, et al. Coronary artery calcium scoring using a reduced tube voltage and radiation dose protocol with dual-source computed tomography. J Cardiovasc Comput Tomogr. 2009; 3:394–400. PMID: 20083060.
Article14. Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006; 113:1213–1225. PMID: 16476843.15. Tomiyama H, Hashimoto H, Hirayama Y, Yambe M, Yamada J, Koji Y, et al. Synergistic acceleration of arterial stiffening in the presence of raised blood pressure and raised plasma glucose. Hypertension. 2006; 47:180–188. PMID: 16380535.
Article16. Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005; 25:932–943. PMID: 15731494.
Article17. Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999; 99:2434–2439. PMID: 10318666.
Article18. Urbano-Moral JA, Rowin EJ, Maron MS, Crean A, Pandian NG. Investigation of global and regional myocardial mechanics with 3-dimensional speckle tracking echocardiography and relations to hypertrophy and fibrosis in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging. 2014; 7:11–19. PMID: 24275954.
Article19. Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG. Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care. 2001; 24:5–10. PMID: 11194240.20. Kim SA, Shim CY, Kim JM, Lee HJ, Choi DH, Choi EY, et al. Impact of left ventricular longitudinal diastolic functional reserve on clinical outcome in patients with type 2 diabetes mellitus. Heart. 2011; 97:1233–1238. PMID: 21653219.
Article21. Fang ZY, Prins JB, Marwick TH. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev. 2004; 25:543–567. PMID: 15294881.
Article22. Hayashi SY, Brodin LA, Alvestrand A, Lind B, Stenvinkel P, Mazza do Nascimento M, et al. Improvement of cardiac function after haemodialysis. Quantitative evaluation by colour tissue velocity imaging. Nephrol Dial Transplant. 2004; 19:1497–1506. PMID: 15034157.
Article23. Wang AY. Cardiovascular risk in diabetic end-stage renal disease patients. J Diabetes. 2011; 3:119–131. PMID: 21599866.
Article24. Meeus F, Kourilsky O, Guerin AP, Gaudry C, Marchais SJ, London GM. Pathophysiology of cardiovascular disease in hemodialysis patients. Kidney Int Suppl. 2000; 76:S140–S147. PMID: 10936811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Diabetic Nephropathy Progressed to End-Stage Renal Disease in an Adolescent with Type 1 Diabetes
- Transplantation Options in Type 1 Diabetes with End Stage Renal Disease
- Letter: Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus (Diabetes Metab J 2018;42:285-95)
- "Off-pump" Coronary Artery Bypass Graft in the Chronic Renal Failure Patients: 3 Cases Report
- Hemangioma Mistaken for Renal Cell Carcinoma in a Patient With End-Stage Renal Disease: A Case Report