The Cut-off Values of Triglycerides and Glucose Index for Metabolic Syndrome in American and Korean Adolescents
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Hanyang University, College of Medicine, Seoul, Korea. ahnyh1129@gmail.com
- KMID: 2366638
- DOI: http://doi.org/10.3346/jkms.2017.32.3.427
Abstract
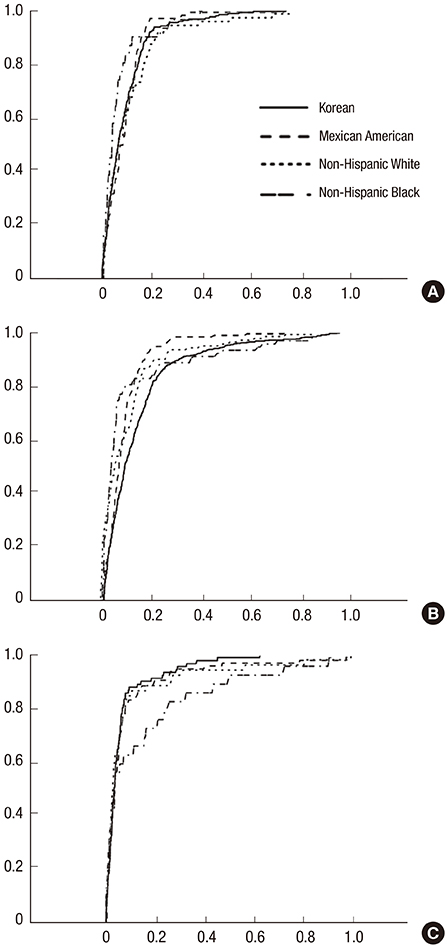
- The aim of this study was to establish ethnic- and gender-specific cut-off values of triglycerides and glucose index (TyG index) for clinical usefulness in a representative sample of Mexican American, Non-Hispanic White, Non-Hispanic Black, and Korean adolescents. The data were collected from datasets of the National Health and Nutrition Examination Survey between 1999 and 2012, and the Korean National Health and Nutrition Examination Survey between 2005 and 2013. Receiver operating characteristic curve analysis was used to find valid cut-off values of the TyG index for metabolic syndrome. The total number of eligible participants was 3,164 in the US and 4,873 in Korea. The optimal cut-off value with the Cook et al. definition revealed 8.55 in Mexican American, 8.55 in Non-Hispanic White, 8.35 in Non-Hispanic Black, and 8.45 in Korean, respectively. The cut-off value with the de Ferranti et al. definition was 8.45, 8.45, 8.15, and 8.35, and the cut-off value with the International Diabetes Federation definition was 8.65, 8.65, 8.15, and 8.55, respectively. These findings may be clinically useful for evaluating insulin resistance for determining metabolic abnormalities in adolescents.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Fasting and Non-Fasting Triglycerides in Patients With Acute Ischemic Stroke
Jun Yup Kim, Keon-Joo Lee, Jihoon Kang, Beom Joon Kim, Moon-Ku Han, Kyusik Kang, Jong-Moo Park, Tai Hwan Park, Hong-Kyun Park, Yong-Jin Cho, Keun-Sik Hong, Kyung Bok Lee, Myung Suk Jang, Ji Sung Lee, Juneyoung Lee, Hee-Joon Bae
J Korean Med Sci. 2022;37(13):e100. doi: 10.3346/jkms.2022.37.e100.Triglyceride and glucose index for identifying abnormal insulin sensitivity in women with polycystic ovary syndrome
Seeun Kwon, Aram Heo, Sungwook Chun
Obstet Gynecol Sci. 2023;66(4):307-315. doi: 10.5468/ogs.23103.Insulin resistance and type 2 diabetes in children
Valeria Castorani, Nella Polidori, Cosimo Giannini, Annalisa Blasetti, Francesco Chiarelli
Ann Pediatr Endocrinol Metab. 2020;25(4):217-226. doi: 10.6065/apem.2040090.045.The impacts of COVID-19 on childhood obesity: prevalence, contributing factors, and implications for management
Min-Ji Kim, Minji Kim, Ju Young Yoon, Chong Kun Cheon, Sukdong Yoo
Ann Pediatr Endocrinol Metab. 2024;29(3):174-181. doi: 10.6065/apem.2346094.047.
Reference
-
1. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979; 237:E214–23.2. Bergman RN, Prager R, Volund A, Olefsky JM. Equivalence of the insulin sensitivity index in man derived by the minimal model method and the euglycemic glucose clamp. J Clin Invest. 1987; 79:790–800.3. Greenfield MS, Doberne L, Kraemer F, Tobey T, Reaven G. Assessment of insulin resistance with the insulin suppression test and the euglycemic clamp. Diabetes. 1981; 30:387–392.4. Lim MH, Oh TJ, Choi K, Lee JC, Cho YM, Kim S. Application of the oral minimal model to Korean subjects with normal glucose tolerance and type 2 diabetes mellitus. Diabetes Metab J. 2016; 40:308–317.5. Lee H. Methods for the assessment of insulin resistance. J Korean Diabetes. 2014; 15:7–11.6. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.7. Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000; 85:2402–2410.8. McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, Duncan AW. Diagnosing insulin resistance in the general population. Diabetes Care. 2001; 24:460–464.9. Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, Gude F, García F, De Francisco A, Quintela AG. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord. 2013; 13:47.10. Esteghamati A, Ashraf H, Esteghamati AR, Meysamie A, Khalilzadeh O, Nakhjavani M, Abbasi M. Optimal threshold of homeostasis model assessment for insulin resistance in an Iranian population: the implication of metabolic syndrome to detect insulin resistance. Diabetes Res Clin Pract. 2009; 84:279–287.11. Ascaso JF, Romero P, Real JT, Priego A, Valdecabres C, Carmena R. Insulin resistance quantification by fasting insulin plasma values and HOMA index in a non-diabetic population. Med Clin (Barc). 2001; 117:530–533.12. Tomé MA, Botana MA, Cadarso-Suárez C, Rego-Iraeta A, Fernández-Mariño A, Mato JA, Solache I, Perez-Fernandez R. Prevalence of metabolic syndrome in Galicia (NW Spain) on four alternative definitions and association with insulin resistance. J Endocrinol Invest. 2009; 32:505–511.13. Ryu S, Sung KC, Chang Y, Lee WY, Rhee EJ. Spectrum of insulin sensitivity in the Korean population. Metabolism. 2005; 54:1644–1651.14. Lee S, Choi S, Kim HJ, Chung YS, Lee KW, Lee HC, Huh KB, Kim DJ. Cutoff values of surrogate measures of insulin resistance for metabolic syndrome in Korean non-diabetic adults. J Korean Med Sci. 2006; 21:695–700.15. Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, Jacques-Camarena O, Rodríguez-Morán M. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010; 95:3347–3351.16. Centers for Disease Control and Prevention (US). National Health and Nutrition Examination Survey 2005-2006, data documentation, codebook, and frequencies: plasma fasting glucose and insulin (GLU_D) [Internet]. accessed on 13 September 2014. Available at https://wwwn.cdc.gov/nchs/nhanes/2005-2006/GLU_D.htm.17. Centers for Disease Control and Prevention (US). National Health and Nutrition Examination Survey 2007-2008, data documentation, codebook, and frequencies: plasma fasting glucose and insulin (GLU_E) [Internet]. accessed on 13 September 2014. Available at https://wwwn.cdc.gov/nchs/nhanes/2007-2008/GLU_E.htm.18. Centers for Disease Control and Prevention (US). National Health and Nutrition Examination Survey 2005-2006, data documentation: cholesterol - HDL (HDL_D) [Internet]. accessed on 13 September 2014. Available at https://wwwn.cdc.gov/nchs/nhanes/2005-2006/HDL_D.htm.19. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3). Cheongwon: Korea Centers for Disease Control and Prevention;2010.20. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2010: Korea National Health and Nutrition Examination Survey (KNHANES V-1). Cheongwon: Korea Centers for Disease Control and Prevention;2011.21. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003; 157:821–827.22. de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: findings from the third National Health and Nutrition Examination Survey. Circulation. 2004; 110:2494–2497.23. Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S. The metabolic syndrome in children and adolescents. Lancet. 2007; 369:2059–2061.24. Kim DH, Yoon JH, Kim HS, Kim DK, Cheong MY. Gender difference of insulin resistance in obese children and adolescents. J Korean Soc Pediatr Endocrinol. 2005; 10:84–89.25. Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008; 6:299–304.26. Vasques AC, Novaes FS, de Oliveira Mda S, Souza JR, Yamanaka A, Pareja JC, Tambascia MA, Saad MJ, Geloneze B. TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pract. 2011; 93:e98–100.27. Abbasi F, Reaven GM. Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides × glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism. 2011; 60:1673–1676.28. Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014; 13:146.29. Unger G, Benozzi SF, Perruzza F, Pennacchiotti GL. Triglycerides and glucose index: a useful indicator of insulin resistance. Endocrinol Nutr. 2014; 61:533–540.30. Lee SH, Han K, Yang HK, Kim MK, Yoon KH, Kwon HS, Park YM. Identifying subgroups of obesity using the product of triglycerides and glucose: the Korea National Health and Nutrition Examination Survey, 2008-2010. Clin Endocrinol (Oxf). 2015; 82:213–220.31. Lee SH, Kwon HS, Park YM, Ha HS, Jeong SH, Yang HK, Lee JH, Yim HW, Kang MI, Lee WC, et al. Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju Metabolic Disease Cohort (CMC) study. PLoS One. 2014; 9:e90430.32. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002; 287:356–359.33. Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008; 196:696–703.34. Sumner AE. Ethnic differences in triglyceride levels and high-density lipoprotein lead to underdiagnosis of the metabolic syndrome in black children and adults. J Pediatr. 2009; 155:S7.e7–S7.e11.35. Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006; 29:1263–1268.36. Ferdinand KC. Coronary artery disease in minority racial and ethnic groups in the United States. Am J Cardiol. 2006; 97:12A–9A.37. Haffner SM, D’Agostino R, Saad MF, Rewers M, Mykkänen L, Selby J, Howard G, Savage PJ, Hamman RF, Wagenknecht LE, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes. 1996; 45:742–748.38. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003; 290:199–206.39. Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004; 291:2847–2850.40. Agudelo GM, Bedoya G, Estrada A, Patiño FA, Muñoz AM, Velásquez CM. Variations in the prevalence of metabolic syndrome in adolescents according to different criteria used for diagnosis: which definition should be chosen for this age group? Metab Syndr Relat Disord. 2014; 12:202–209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of the Metabolic Syndrome among Outpatients with Schizophrenia or Schizoaffective Disorder
- Preliminary analysis of metabolic syndrome components in Korean adolescents by using Korean national health and nutrition examination Survey pooling data (1998, 2001, and 2005)
- The cutoff values of indirect indices for measuring insulin resistance for metabolic syndrome in Korean children and adolescents
- Waist-to-height Ratio, a Simple and Practical Index for Screening of Adolescent Metabolic Syndrome Aged 17~19 Years
- Metabolic Syndrome in Children