J Korean Med Sci.
2017 Feb;32(2):257-263. 10.3346/jkms.2017.32.2.257.
Nutritional Status in Adults with Predialysis Chronic Kidney Disease: KNOW-CKD Study
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. kyubeck.lee@samsung.com
- 2Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Inje University Pusan Paik Hospital, Busan, Korea.
- 4Department of Internal Medicine, The Catholic University of Korea, Seoul St Mary's Hospital, Seoul, Korea.
- 5Department of Internal Medicine, Eulji General Hospital, Eulji University, Seoul, Korea.
- 6Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2364169
- DOI: http://doi.org/10.3346/jkms.2017.32.2.257
Abstract
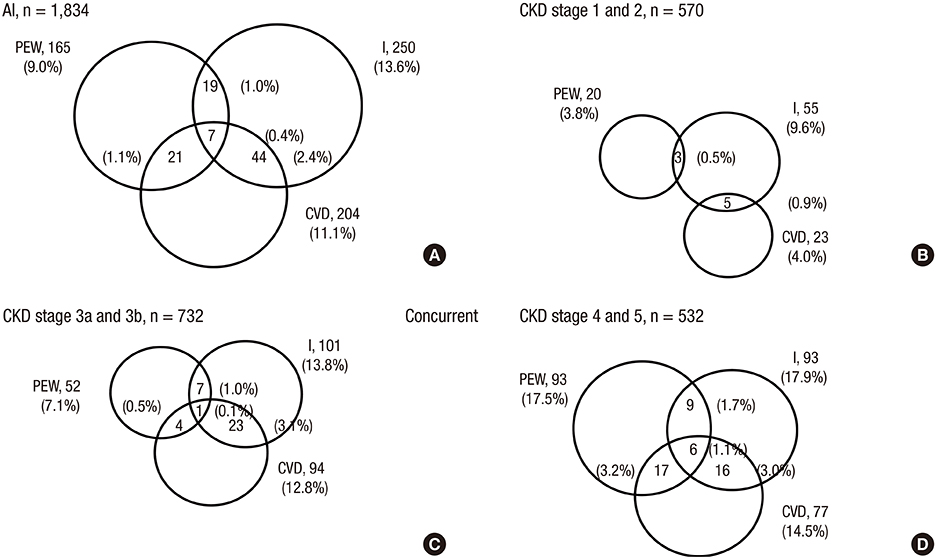
- Adverse changes in nutrition are prevalent and are strong indicators of adverse outcomes in patients with chronic kidney disease (CKD). The International Society of Renal Nutrition and Metabolism (ISRNM) proposed a common nomenclature and diagnostic criteria to identify protein-energy wasting (PEW) in CKD patients. We examined the nutritional status in 1,834 adults with predialysis CKD enrolled in the KoreaN cohort study for Outcome in patients With Chronic Kidney Disease (KNOW-CKD) study. As there was a need for further understanding of nutritional status and associated factors in CKD, we evaluated the prevalence and associated factors of PEW in adults with predialysis CKD. The prevalence of PEW was about 9.0% according to ISRNM criteria and tended to increase with advanced stage in predialysis CKD. Those who concurrently had PEW, inflammation, and CVD were a small proportion (0.4%). In multivariate logistic regression model, PEW was independently associated with estimated glomerular filtration rate (eGFR) (odds ratio [OR], 0.98; 95% confidence interval [CI], 0.96-0.99), total CO2 (OR, 0.93; 95% CI, 0.87-0.99), physical activity (OR, 0.43; 95% CI, 0.26-0.69), comorbid diabetes (OR, 1.68; 95% CI, 1.09-2.59), and high sensitivity C-reactive protein (hs-CRP) (OR, 1.03; 95% CI, 1.01-1.06). Our study suggests that PEW increases with advanced CKD stage. PEW is independently associated with renal function, low total CO2, low physical activity, comorbid diabetes, and increased hs-CRP in adults with predialysis CKD.
MeSH Terms
Figure
Cited by 1 articles
-
Hand Grip and Leg Muscle Strength in Hemodialysis Patients and Its Determinants
Ran-hui Cha, Geum Sil Lee, Ju Yeon Yoo, Oe Bog Rhee, Yong Duk Jeon
J Korean Med Sci. 2021;36(11):e76. doi: 10.3346/jkms.2021.36.e76.
Reference
-
1. Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, Saran R, Wang AY, Yang CW. Chronic kidney disease: global dimension and perspectives. Lancet. 2013; 382:260–272.2. Fouque D, Pelletier S, Mafra D, Chauveau P. Nutrition and chronic kidney disease. Kidney Int. 2011; 80:348–357.3. Carrero JJ, Stenvinkel P, Cuppari L, Ikizler TA, Kalantar-Zadeh K, Kaysen G, Mitch WE, Price SR, Wanner C, Wang AY, et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Ren Nutr. 2013; 23:77–90.4. Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008; 73:391–398.5. Stenvinkel P, Heimbürger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999; 55:1899–1911.6. Qureshi AR, Alvestrand A, Divino-Filho JC, Gutierrez A, Heimbürger O, Lindholm B, Bergström J. Inflammation, malnutrition, and cardiac disease as predictors of mortality in hemodialysis patients. J Am Soc Nephrol. 2002; 13:Suppl 1. S28–36.7. de Mutsert R, Grootendorst DC, Axelsson J, Boeschoten EW, Krediet RT, Dekker FW; NECOSAD Study Group. Excess mortality due to interaction between protein-energy wasting, inflammation and cardiovascular disease in chronic dialysis patients. Nephrol Dial Transplant. 2008; 23:2957–2964.8. Han SS, Shin N, Lee SM, Lee H, Kim DK, Kim YS. Correlation between periodontitis and chronic kidney disease in Korean adults. Kidney Res Clin Pract. 2013; 32:164–170.9. Oh KH, Park SK, Park HC, Chin HJ, Chae DW, Choi KH, Han SH, Yoo TH, Lee K, Kim YS, et al. KNOW-CKD (Korean cohort study for outcome in patients with chronic kidney disease): design and methods. BMC Nephrol. 2014; 15:80.10. Masud T, Manatunga A, Cotsonis G, Mitch WE. The precision of estimating protein intake of patients with chronic renal failure. Kidney Int. 2002; 62:1750–1756.11. Kovesdy CP, Kopple JD, Kalantar-Zadeh K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: reconciling low protein intake with nutritional therapy. Am J Clin Nutr. 2013; 97:1163–1177.12. Chapter 1: definition and classification of CKD. Kidney Int Suppl. 2011; 2013:19–62.13. Myers GL, Christenson RH, Cushman M, Ballantyne CM, Cooper GR, Pfeiffer CM, Grundy SM, Labarthe DR, Levy D, Rifai N, et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice guidelines: emerging biomarkers for primary prevention of cardiovascular disease. Clin Chem. 2009; 55:378–384.14. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization;2010.15. Pupim LB, Caglar K, Hakim RM, Shyr Y, Ikizler TA. Uremic malnutrition is a predictor of death independent of inflammatory status. Kidney Int. 2004; 66:2054–2060.16. Pecoits-Filho R, Lindholm B, Stenvinkel P. The malnutrition, inflammation, and atherosclerosis (MIA) syndrome -- the heart of the matter. Nephrol Dial Transplant. 2002; 17:Suppl 11. 28–31.17. Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD. Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis. 2003; 42:864–881.18. Di Micco L, Quinn RR, Ronksley PE, Bellizzi V, Lewin AM, Cianciaruso B, Ravani P; Alberta Kidney Disease Network (AKDN). Urine creatinine excretion and clinical outcomes in CKD. Clin J Am Soc Nephrol. 2013; 8:1877–1883.19. Wilson FP, Xie D, Anderson AH, Leonard MB, Reese PP, Delafontaine P, Horwitz E, Kallem R, Navaneethan S, Ojo A, et al. Urinary creatinine excretion, bioelectrical impedance analysis, and clinical outcomes in patients with CKD: the CRIC study. Clin J Am Soc Nephrol. 2014; 9:2095–2103.20. Tynkevich E, Flamant M, Haymann JP, Metzger M, Thervet E, Boffa JJ, Vrtovsnik F, Houillier P, Froissart M, Stengel B. NephroTest Study Group. Urinary creatinine excretion, measured glomerular filtration rate and CKD outcomes. Nephrol Dial Transplant. 2015; 30:1386–1394.21. Franch HA, Raissi S, Wang X, Zheng B, Bailey JL, Price SR. Acidosis impairs insulin receptor substrate-1-associated phosphoinositide 3-kinase signaling in muscle cells: consequences on proteolysis. Am J Physiol Renal Physiol. 2004; 287:F700–6.22. Lee SW, Dai G, Hu Z, Wang X, Du J, Mitch WE. Regulation of muscle protein degradation: coordinated control of apoptotic and ubiquitin-proteasome systems by phosphatidylinositol 3 kinase. J Am Soc Nephrol. 2004; 15:1537–1545.23. Johansen KL, Painter P. Exercise in individuals with CKD. Am J Kidney Dis. 2012; 59:126–134.24. LeBrasseur NK, Walsh K, Arany Z. Metabolic benefits of resistance training and fast glycolytic skeletal muscle. Am J Physiol Endocrinol Metab. 2011; 300:E3–10.25. Lertdumrongluk P, Kovesdy CP, Norris KC, Kalantar-Zadeh K. Nutritional and inflammatory axis of racial survival disparities. Semin Dial. 2013; 26:36–39.26. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:S49–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Bicarbonate Supplementation on Renal Function and Nutritional Indices in Predialysis Advanced Chronic Kidney Disease
- Personalized nutritional management in the transition from non-dialysis dependent chronic kidney disease to dialysis
- Osteoporosis in Patients with Chronic Kidney Disease
- Proinflammatory CD14+CD16+ monocytes are associated with vascular stiffness in predialysis patients with chronic kidney disease
- Anemia in children with chronic kidney disease