J Korean Soc Transplant.
2010 Dec;24(4):298-305.
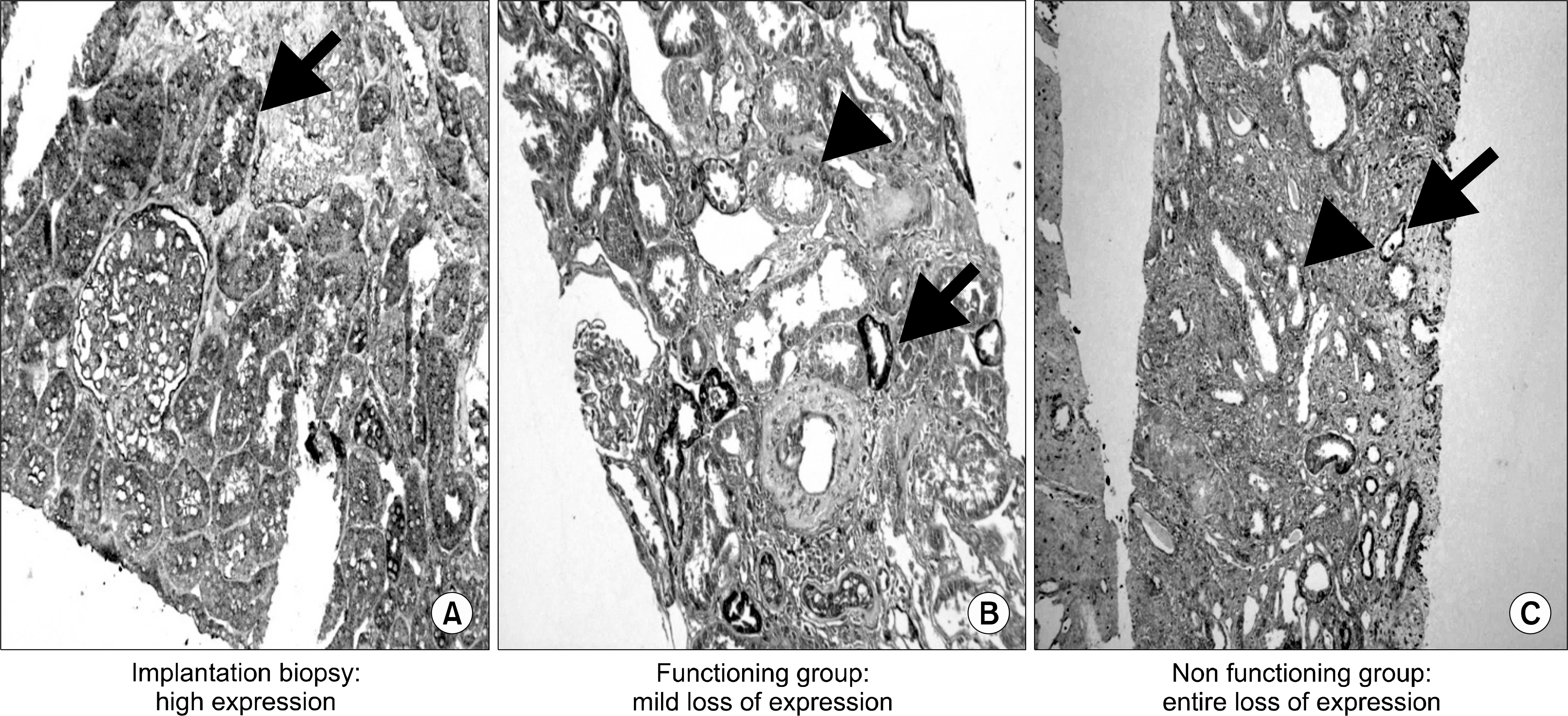
Expression of E-cadherin, Heat Shock Protein 47, Transforming Growth Factor beta1 and C4d in Chronic Allograft Nephropathy
- Affiliations
-
- 1Department of Surgery, Kang-dong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. slee@hallym.or.kr
- 2Department of Pathology, Kang-dong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Transplantation Center, Kang-dong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
Abstract
- BACKGROUND
Chronic allograft nephropathy (CAN), which causes graft failure, is related to tubular atrophy and interstitial fibrosis. E-cadherin is a well-known epithelial marker and heat shock protein (HSP)-47 is a collagen-specific molecular chaperone that regulates collagen synthesis. Transforming growth factor (TGF)-beta1, a profibrotic cytokine, downregulates E-cadherin and induces expression of mesenchymal markers in an in vitro model. C4d expression is considered a poor prognostic marker for graft survival. This study evaluated the relationship between the expression of E-cadherin, HSP47, TGF-beta1, and C4d with the prognosis for CAN.
METHODS
Between March 1991 and August 2007, we performed renal allograft biopsies on 42 recipients with deteriorating renal function. CAN was diagnosed according to the chronic allograft damage index (Banff classification). Renal allograft biopsies were examined for the expression of E-cadherin, HSP47, TGF-beta1, or C4d by immunohistochemistry. The HSP47, TGF-beta1, and E-cadherin staining was scored semiquantitatively by analyzing ten different fields of cortical interstitium and tubules. Biopsies with endothelial C4d staining in peri-tubular capillaries (> or =25%) were designated as C4d-positive.
RESULTS
Of 42 recipients, 17 (40.5%) were in the graft survival group (GS) and 25 (59.5%) were in the graft failure group (GF). E-cadherin expression in tubular cells of the GS was much higher than that of the GF (94.1% vs 52%, P=0.04). HSP47 expression in tubular cells and interstitium in the GF was much higher than that in the GS (84% vs 35.3%, P=0.001). TGF-beta1 expression in tubular cells and interstitium in the GF was much higher than that in the GS (72% vs 23.5%, P=0.02).
CONCLUSIONS
E-cadherin, HSP47, and TGF-beta1 expression was strongly correlated with the CAN prognosis.
Keyword
MeSH Terms
-
Atrophy
Biopsy
Cadherins
Capillaries
Collagen
Fibrosis
Graft Survival
Heat-Shock Proteins
Hot Temperature
HSP47 Heat-Shock Proteins
Immunohistochemistry
Molecular Chaperones
Prognosis
Transforming Growth Factor beta1
Transforming Growth Factors
Transplantation, Homologous
Transplants
Cadherins
Collagen
HSP47 Heat-Shock Proteins
Heat-Shock Proteins
Molecular Chaperones
Transforming Growth Factor beta1
Transforming Growth Factors
Figure
Reference
-
References
1). United States Renal Data System. USRDS 2003 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD.: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;2003. p. 1–560.2). In Danovitch GM. Handbook of kidney transplantation. 4th ed.Philadelphia: Lippincott Williams & Wilkins;2005. : 242.3). Kreis HA, Ponticelli C. Causes of late renal allograft loss: chronic allograft dysfunction, death, and other factors. Transplantation. 2001; 71(11 Suppl):SS5–9.4). Vongwiwatana A, Tasanarong A, Rayner DC, Melk A, Halloran PF. Epithelial to mesenchymal transition during late deterioration of human kidney transplants: the role of tubular cells infibrogenesis. Am J Transplant. 2005; 5:1367–74.5). Ohba K, Miyata Y, Koga S, Nishikido M, Kanetake H, Nazneen A, et al. Interstitial expression of heat-shock protein 47 correlates with capillary deposition of complement split product C4d in chronic allograft nephropathy. Clin Transplant. 2005; 19:810–6.
Article6). Razzaque MS, Kumatori A, Harada T, Taguchi T. Coexpression of collagens and collagen-binding heat shock protein 47 in human diabetic nephropathy and IgA nephropathy. Nephron. 1998; 80:434–43.
Article7). Zavadil J, Bottinger EP. TGF-beta and epithelial-to-mesenchymal transitions. Oncogene. 2005; 24:5764–74.8). Regele H, Bohmig GA, Habicht A, Gollowitzer D, Schillinger M, Rockenschaub S, et al. Capillary deposition of complement split product C4d in renal allografts is associated with basement membrane injury in peritubular and glomerular capillaries: a contribution of humoral immunity to chronic allograft rejection. J Am Soc Nephrol. 2002; 13:2371–80.
Article9). Solez K, Vincenti F, Filo RS. Histopathologic findings from 2-year protocol biopsies from a U.S. multicenter kidney transplant trial comparing tacrolimus versus cyclosporine: a report of the FK506 Kidney Transplant Study Group. Transplantation. 1998; 66:1736–40.10). Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999; 55:713–23.
Article11). Halloran PF. Call for revolution: a new approach to describing allograft deterioration. Am J Transplant. 2002; 2:195–200.
Article12). Freese P, Svalander CT, Molne J, Norden G, Nyberg G. Chronic allograft nephropathy-biopsy finding and outcome. Nephrol Dial Transplant. 2001; 16:2401–6.13). Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 2002; 110:341–50.
Article14). Liu Y. Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol. 2004; 15:1–12.
Article15). Hay ED, Zuk A. Transformations between epithelium and mesenchyme: normal, pathological and experimentally induced. Am J Kidney Dis. 1995; 26:678–90.
Article16). Birchmeier W, Birchmeier C. Epithelial-mesenchymal transitions in development and tumor progression. EXS. 1995; 74:1–15.
Article17). Rastaldi MP, Ferrario F, Giardino L, Dell'Antonio G, Grillo C, Grillo P, et al. Epithelial-mesenchymal transition of tubular epithelial cells in human renal biopsies. Kidney Int. 2002; 62:137–46.
Article18). Razzaque MS, Le VT, Taguchi T. Heat shock protein 47 and renal fibrogenesis. Contrib Nephrol. 2005; 148:57–69.
Article19). Abe K, Ozono Y, Miyazaki M, Koji T, Shioshita K, Furusu A, et al. Interstitial expression of heat shock protein 47 and alpha-smooth muscle actin in renal allograft failure. Nephrol Dial Transplant. 2000; 15:529–35.20). Zeisberg M, Bonner G, Maeshima Y, Colorado P, Muller GA, Strutz F, et al. Renal fibrosis: collagen composition and assembly regulates epithelial-mesenchymal transdifferentiation. Am J Pathol. 2001; 159:1313–21.21). Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and an-giotensin-converting enzyme inhibition: a patient-level metaanalysis. Ann Intern Med. 2003; 139:244–52.
Article22). Bijian K, Cybulsky AV. Stress proteins in glomerular epithelial cell injury. Contrib Nephrol. 2005; 148:8–20.
Article23). Zoja C, Corna D, Camozzi D, Cattaneo D, Rottoli D, Batani C, et al. How to fully protect the kidney in a severe model of progressive nephropathy: a multidrug approach. J Am Soc Nephrol. 2002; 13:2898–908.
Article24). Suthanthiran M, Khanna A, Cukran D, Adhikarla R, Sharma VK, Singh T, et al. Transforming growth factor-beta 1 hyperexpression in African American end-stage renal disease patients. Kidney Int. 1998; 53:639–44.25). Park MG, Joo SH, Park SK, Kim JS, Hyun SJ, Nam ES, et al. Correlation of hypoxia inducible factor-1α & transforming grwth factor-1β expression and progression of renal allograft. J Korean Soc Transplant. 2005; 19:131–6. (박민근, 주선형, 박성길, 김주섭, 현숙자, 남은숙, 등. 신생검에서의 Hypoxia Inducible Factor-1α, Transforming Growth Factor-β1 발현과 이식신 예후와의 연관성. 대한이식학회지 2005;19: 131–6.).26). Lorenz M, Regele H, Schillinger M, Exner M, Rasoul Rokenschaub S, Wahrmann M, et al. Risk factors for capillary C4d deposition in kidney allografts: evaluation of a large study cohort. Transplantation. 2004; 78:447–52.
Article27). Bohmig GA, Exner M, Habicht A, Schillinger M, Lang U, Kletzmayr J, et al. Capillary C4d deposition in kidney allografts: a specific marker of alloantibody-dependent graft injury. J Am Soc Nephrol. 2002; 13:1091–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expression of Transforming Growth Factor beta1 and Cadherins in Lung Adenocarcinoma
- Renal Expression and Usefulness of TGF-beta-inducible Gene-h3 in Human Type II Diabetic Nephropathy -Immunohistochemical Analysis-
- The Transforming Growth Factor-beta1 Expression in Normal Laryngeal Mucosa, Laryngeal Dysplasia and Laryngeal Carcinoma
- Oxidative Stress and Chronic Allograft Nephropathy
- Protective Effect of N-Acetylcysteine on Progression of Adriamycin-induced Nephropathy