Tuberc Respir Dis.
2012 Jan;72(1):15-23.
Prognostic Factors and Scoring Systems for Non-Small Cell Lung Cancer Patients Harboring Brain Metastases Treated with Gamma Knife Radiosurgery
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. leemk@pusan.ac.kr
- 2Departments of Neurosurgery, Pusan National University School of Medicine, Busan, Korea.
Abstract
- BACKGROUND
The survival of non-small cell lung cancer (NSCLC) patients with brain metastases is reported to be 3~6 months even with aggressive treatment. Some patients have very short survival after aggressive treatment and reliable prognostic scoring systems for patients with cancer have a strong correlation with outcome, often supporting decision making and treatment recommendations.
METHODS
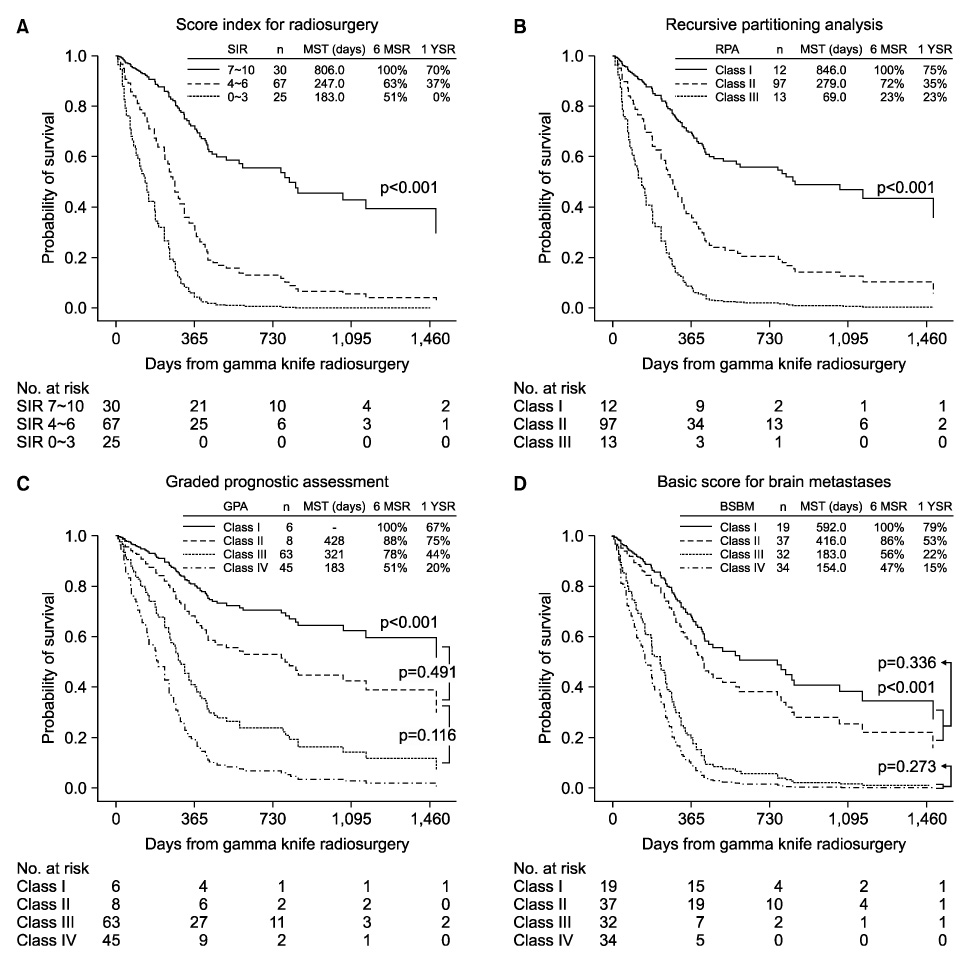
A total of one hundred twenty two NSCLC patients with brain metastases who received gamma knife radiosurgery (GKRS) were analyzed. Survival analysis was calculated in all patients for thirteen available prognostic factors and four prognostic scoring systems: score index for radiosurgery (SIR), recursive partitioning analysis (RPA), graded prognostic assessment (GPA), and basic score for brain metastases (BSBM).
RESULTS
Age, Karnofsky performance status, largest brain lesion volume, systemic chemotherapy, primary tumor control, and medication of epidermal growth factor receptor tyrosine kinase inhibitor were statistically independent prognostic factors for survival. A multivariate model of SIR and RPA identified significant differences between each group of scores. We found that three-tiered indices such as SIR and RPA are more useful than four-tiered scoring systems (GPA and BSBM).
CONCLUSION
There is little value of RPA class III (most unfavorable group) for the same results of 6-month and 1-year survival rate. Thus, SIR is the most useful index to sort out patients with poorer prognosis. Further prospective trials should be performed to develop a new molecular- and gene-based prognostic index model.
MeSH Terms
Figure
Reference
-
1. Pizzocaro G, Ravasi GL. Surgical treatment of carcinoma of the esophagus and of the cardia: evaluation of the immediate and remote results. Tumori. 1970. 56:279–289.2. Flannery TW, Suntharalingam M, Kwok Y, Koffman BH, Amin PP, Chin LS, et al. Gamma knife stereotactic radiosurgery for synchronous versus metachronous solitary brain metastases from non-small cell lung cancer. Lung Cancer. 2003. 42:327–333.3. Komaki R, Cox JD, Stark R. Frequency of brain metastasis in adenocarcinoma and large cell carcinoma of the lung: correlation with survival. Int J Radiat Oncol Biol Phys. 1983. 9:1467–1470.4. Jacot W, Quantin X, Boher JM, Andre F, Moreau L, Gainet M, et al. Brain metastases at the time of presentation of non-small cell lung cancer: a multi-centric AERIO analysis of prognostic factors. Br J Cancer. 2001. 84:903–909.5. Nieder C, Thamm R, Astner ST, Molls M. Prediction of very short survival in patients with brain metastases from non-small cell lung cancer. Cancer Ther. 2008. 6:163–166.6. Pan HC, Sheehan J, Stroila M, Steiner M, Steiner L. Gamma knife surgery for brain metastases from lung cancer. J Neurosurg. 2005. 102:Suppl. 128–133.7. Nieder C, Bremnes RM, Andratschke NH. Prognostic scores in patients with brain metastases from non-small cell lung cancer. J Thorac Oncol. 2009. 4:1337–1341.8. Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997. 37:745–751.9. Weltman E, Salvajoli JV, Brandt RA, de Morais Hanriot R, Prisco FE, Cruz JC, et al. Radiosurgery for brain metastases: a score index for predicting prognosis. Int J Radiat Oncol Biol Phys. 2000. 46:1155–1161.10. Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W. A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys. 2008. 70:510–514.11. Lorenzoni J, Devriendt D, Massager N, David P, Ruíz S, Vanderlinden B, et al. Radiosurgery for treatment of brain metastases: estimation of patient eligibility using three stratification systems. Int J Radiat Oncol Biol Phys. 2004. 60:218–224.12. Vallières E, Shepherd FA, Crowley J, Van Houtte P, Postmus PE, Carney D, et al. The IASLC Lung Cancer Staging Project: proposals regarding the relevance of TNM in the pathologic staging of small cell lung cancer in the forthcoming (seventh) edition of the TNM classification for lung cancer. J Thorac Oncol. 2009. 4:1049–1059.13. Rades D, Schild SE, Lohynska R, Veninga T, Stalpers LJ, Dunst J. Two radiation regimens and prognostic factors for brain metastases in nonsmall cell lung cancer patients. Cancer. 2007. 110:1077–1082.14. Mariya Y, Sekizawa G, Matsuoka Y, Seki H, Sugawara T. Outcome of stereotactic radiosurgery for patients with non-small cell lung cancer metastatic to the brain. J Radiat Res (Tokyo). 2010. 51:333–342.15. Pan HC, Sheehan J, Stroila M, Steiner M, Steiner L. Gamma knife surgery for brain metastases from lung cancer. J Neurosurg. 2005. 102:Suppl. 128–133.16. Griffin TW, Pajak TF, Gillespie BW, Davis LW, Brady LW, Rubin P, et al. Predicting the response of head and neck cancers to radiation therapy with a multivariate modelling system: an analysis of the RTOG head and neck registry. Int J Radiat Oncol Biol Phys. 1984. 10:481–487.17. Weissman DE. Glucocorticoid treatment for brain metastases and epidural spinal cord compression: a review. J Clin Oncol. 1988. 6:543–551.18. Gülbaş H, Erkal HS, Serin M. The use of recursive partitioning analysis grouping in patients with brain metastases from non-small-cell lung cancer. Jpn J Clin Oncol. 2006. 36:193–196.19. Rodrigus P, de Brouwer P, Raaymakers E. Brain metastases and non-small cell lung cancer. Prognostic factors and correlation with survival after irradiation. Lung Cancer. 2001. 32:129–136.20. Gow CH, Chien CR, Chang YL, Chiu YH, Kuo SH, Shih JY, et al. Radiotherapy in lung adenocarcinoma with brain metastases: effects of activating epidermal growth factor receptor mutations on clinical response. Clin Cancer Res. 2008. 14:162–168.21. Lind JS, Lagerwaard FJ, Smit EF, Senan S. Phase I study of concurrent whole brain radiotherapy and erlotinib for multiple brain metastases from non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2009. 74:1391–1396.22. Altavilla G, Arrigo C, Santarpia MC, Galletti G, Picone G, Marabello G, et al. Erlotinib therapy in a patient with non-small-cell lung cancer and brain metastases. J Neurooncol. 2008. 90:31–33.23. Shimato S, Mitsudomi T, Kosaka T, Yatabe Y, Wakabayashi T, Mizuno M, et al. EGFR mutations in patients with brain metastases from lung cancer: association with the efficacy of gefitinib. Neuro Oncol. 2006. 8:137–144.24. Eichler AF, Kahle KT, Wang DL, Joshi VA, Willers H, Engelman JA, et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro Oncol. 2010. 12:1193–1199.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letters to the Editor: Gamma Knife Radiosurgery for Brain Metastases in Patients Harboring Four or More Lesions : Survival and Prognostic Factors
- The Effect of Epidermal Growth Factor Receptor Mutation on Intracranial Progression-Free Survival of Non-Small Cell Lung Cancer Patients with Brain Metastasis Underwent Gamma Knife Radiosurgery
- Clinical Analysis of Gamma Knife Radiosurgery for Brain Metastases
- Prognosis of Non-Small Cell Lung Cancer with Synchronous Brain Metastases Treated with Gamma Knife Radiosurgery
- Therapeutic Effect of Gamma Knife Radiosurgery for Multiple Brain Metastases