Lab Anim Res.
2012 Mar;28(1):39-46. 10.5625/lar.2012.28.1.39.
Anti-hypercholesterolemic and anti-atherosclerotic effects of polarized-light therapy in rabbits fed a high-cholesterol diet
- Affiliations
-
- 1College of Veterinary Medicine, Chungbuk National University, Cheongju, Korea. solar93@cbu.ac.kr
- 2Department of Biomedical Laboratory Science, Daejeon University, Daejeon, Korea.
- KMID: 2312091
- DOI: http://doi.org/10.5625/lar.2012.28.1.39
Abstract
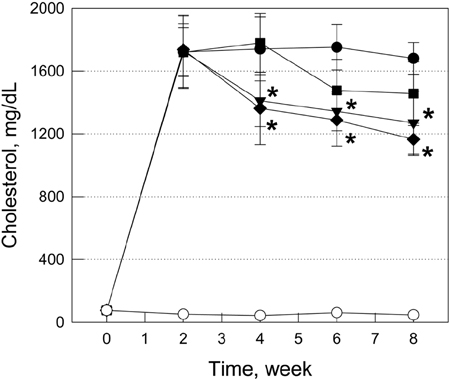
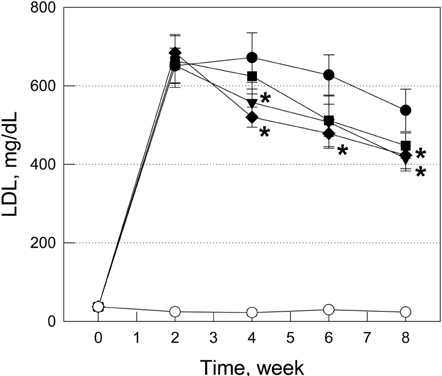
- The effects of polarized-light therapy (PLT) on high-cholesterol diet (HCD)-induced hypercholesterolemia and atherosclerosis were investigated in comparison with that of lovastatin in rabbits. Hypercholesterolemia was induced by feeding male New Zealand white rabbits with 1% cholesterol in diet for 2 weeks and maintained with 0.5% cholesterol for 6 weeks, followed by normal diet for 2 weeks for recovery. Lovastatin (0.002% in diet) or daily 5-min or 20-min PLT on the outside surface of ears was started 2 weeks after induction of hypercholesterolemia. Hypercholesterolemic rabbits exhibited great increases in serum cholesterol and low-density lipoproteins (LDL) levels, and finally severe atheromatous plaques formation covering 57.5% of the arterial walls. Lovastatin markedly reduced both the cholesterol and LDL, but the reducing effect (47.5%) on atheroma formation was relatively low. By comparison, 5-min PLT preferentially decreased LDL, rather than cholesterol, and thereby potentially reduced the atheroma area to 42.2%. Notably, 20-min PLT was superior to lovastatin in reducing both the cholesterol and LDL levels as well as the atheromatous plaque formation (26.4%). In contrast to the increases in blood alanine transaminase and aspartate transaminase following lovastatin treatment, PLT did not cause hepatotoxicity. In addition, PLT decreased platelets and hematocrit level. The results indicate that PLT attenuates atherosclerosis not only by lowering blood cholesterol and LDL levels, but also by improving blood flow without adverse effects. Therefore, it is suggested that PLT could be a safe alternative therapy for the improvement of hypercholesterolemia and atherosclerosis.
MeSH Terms
Figure
Cited by 2 articles
-
An ethanolic extract of
Angelica gigas improves atherosclerosis by inhibiting vascular smooth muscle cell proliferation
Ja Young Jang, Jihyun Kim, Jingmei Cai, Youngeun Kim, Kyungha Shin, Tae-Su Kim, Sung-Pyo Lee, Sung Kyeong Park, Ehn-Kyoung Choi, Yun-Bae Kim
Lab Anim Res. 2014;30(2):84-89. doi: 10.5625/lar.2014.30.2.84.Anti-atherosclerotic effects of perilla oil in rabbits fed a high-cholesterol diet
Yeseul Cha, Ja Young Jang, Young-Hwan Ban, Haiyu Guo, Kyungha Shin, Tae-Su Kim, Sung-Pyo Lee, Jieun Choi, Eun-Suk An, Da-Woom Seo, Jung-Min Yon, Ehn-Kyoung Choi, Yun-Bae Kim
Lab Anim Res. 2016;32(3):171-179. doi: 10.5625/lar.2016.32.3.171.
Reference
-
1. Moon SJ. Nutritional problems in Korea. Korean J Nutr. 1996. 29(4):371–380.2. Huh KB. The present status of nutrition-related diseases and its countermeasures. Korean J Nutr. 1990. 23(3):197–207.3. Lee HK. Pattern of disease incidence and nutrition in Korea. Korean J Nutr. 1996. 29(4):381–383.4. Lee YC. Hypercholesterolemia in Korea and nutritional factors. Korean J Lipidol. 1991. 1(1):111–122.5. Spady DK, Woollett LA, Dietschy JM. Regulation of plasma LDL-cholesterol levels by dietary cholesterol and fatty acids. Annu Rev Nutr. 1993. 13:355–381.6. Natio HK. Atherogenesis: current topics on etiology and risk factors. Clin Chem. 1995. 41:132–133.7. Sanders TA, Oakley FR, Miller GJ, Mitropoulos KA, Crook D, Oliver MF. Influence of n-6 versus n-3 polyunsaturated fatty acids in diets low in saturated fatty acids on plasma lipoproteins and hemostatic factors. Arterioscler Thromb Vasc Biol. 1997. 17(12):3449–3460.8. Judd JT, Baer DJ, Clevidence BA, Muesing RA, Chen SC, Weststrate JA, Meijer GW, Wittes J, Lichtenstein AH, Vilella-Bach M, Schaefer EJ. Effects of margarine compared with those of butter on blood lipid profiles related to cardiovascular disease risk factors in normolipemic adults fed controlled diets. Am J Clin Nutr. 1998. 68(4):768–777.9. Keys A. Coronary heart disease in seven countries. Circulation. 1970. 41:1–11.10. Kannel WB, Castelli WP, Gordon T, McNamara PM. Serum cholesterol, lipoproteins, and the risk of coronary heart disease. The Framingham study. Ann Intern Med. 1971. 74(1):1–12.11. Bae HY. The role of oxidized low density lipoprotein in atherogenesis. J Korean Diabetes Assoc. 1999. 23:7–11.12. Glass CK, Witztum JL. Atherosclerosis. the road ahead. Cell. 2001. 104(4):503–516.13. Shin SH. The choice of medicine. Diagnosis and Treatment in Hyperlipidemia. 2000. Haneuyhak, Seoul: Association of Hyperlipidemic Theraphy;315–331.14. Blum A, Simsolo C, Hasin Y. 3-Hydroxy-3-methylglutaryl coenzyme a (HMG-CoA) reductase inhibitors (statins), atherosclerosis and coronary syndromes. Atherosclerosis. 2004. 175(1):1–5.15. Larsen ML, Illingworth DR. Drug treatment of dyslipoproteinemia. Med Clin North Am. 1994. 78(1):225–245.16. Cho JH, Lee NJ, Chai HY, Kim TM, Park JH, Kang JK, Kim YB, Hwang SY. Effect of Hwalgidan SJ-101 on atherosclerosis in hypercholesterolemic rabbits. Lab Anim Res. 2005. 21:149–158.17. Hong SH, Chai HY, Kim TM, Lee NJ, Kim DK, Cho JH, Park JH, Kim YB, Kang JK, Hwang SY. Therapeutic effects of mulberry root-bark (Mori radicis Cortex) ethanol-extracts on atherosclerosis in hypercholesterolemic rabbits. Lab Anim Res. 2005. 21:273–279.18. Hsiang YN, Todd ME, Bower RD. Determining light dose for photodynamic therapy of atherosclerotic lesions in the Yucatan miniswine. J Endovasc Surg. 1995. 2(4):365–371.19. Hayashi J, Saito T, Aizawa K. Change in chemical composition of lipids accumulated in atheromas of rabbits following photodynamic therapy. Lasers Surg Med. 1997. 21(3):287–293.20. Amemiya T, Nakajima H, Katoh T, Rakue H, Miyagi M, Ibukiyama C. Photodynamic therapy of atherosclerosis using YAG-OPO laser and Porfimer sodium, and comparison with using argon-dye laser. Jpn Circ J. 1999. 63(4):288–295.21. Lymans'kyi IuP, Tamarova ZA, Hutliar SO, Bidkov IeH. The examination of the analgetic action of polarized light. Fiziol Zh. 2000. 46(6):105–111.22. Lymans'kyi IuP, Tamarova ZA, Hutliar SO. Suppression of visceral pain by action of the low intensity polarized light on acupuncture antinociceptive points. Fiziol Zh. 2003. 49(5):43–51.23. Samosiuk IZ, Kulikovich IuN, Tamarova ZA, Samosiuk NI, Kazhanova AK. Pain relief by low-intensity frequency-modulated millimeter waves acting on the acupuncture points. Vopr Kurortol Fizioter Lech Fiz Kult. 2000. 4:7–11.24. Hafkamp AM, Havinga R, Sinaasappel M, Verkade HJ. Effective oral treatment of unconjugated hyperbilirubinemia in Gunn rats. Hepatology. 2005. 41(3):526–534.25. Tamarova ZA, Lymans'kyi IuP, Hutliar SO. Comparative testing of analgesia induced by polarized light and analgetics. Fiziol Zh. 2005. 51(2):57–64.26. Limansky YP, Tamarova ZA, Gulyar SA. Suppression of pain by exposure of acupuncture points to polarized light. Pain Res Manag. 2006. 11(1):49–57.27. Rastad C, Ulfberg J, Lindberg P. Improvement in Fatigue, Sleepiness, and Health-Related Quality of Life with Bright Light Treatment in Persons with Seasonal Affective Disorder and Subsyndromal SAD. Depress Res Treat. 2011. 2011:543906.28. Kobayashi H, Matsushita M, Oda K, Nishikimi N, Sakurai T, Komori K. Effects of atherosclerotic plaque on the enlargement of an experimental model of abdominal aortic aneurysm in rabbits. Eur J Vasc Endovasc Surg. 2004. 28(1):71–78.29. Anistchow N, Chalatow S. Ueber experimentelle cholesterinstetase und die bedeutung fur die enstehung einiger pathdogischer prozesse. Zebtrabl Allg Pathol. 1913. 24:1–9.30. McClelland GA, Stubbs RJ, Fix JA, Pogany SA, Zentner GM. Enhancement of 3-hydroxy-3-methylglutaryl-coenzyme A (HMGCoA) reductase inhibitor efficacy through administration of a controlled-porosity osmotic pump dosage form. Pharm Res. 1991. 8(7):873–876.31. Yim JE, Choue RW, Kim YS. Effects of dietary counceling and HMG Co A reductase inhibitor treatment on serum lipid levels in hyperlipidemic patients. Korean J Lipidol. 1998. 8(1):61–76.32. MacDonald JS, Gerson RJ, Kornbrust DJ, Kloss MW, Prahalada S, Berry PH, Alberts AW, Bokelman DL. Preclinical evaluation of lovastatin. Am J Cardiol. 1988. 62(15):16J–27J.33. de Denus S, Spinler SA, Miller K, Peterson AM. Statins and liver toxicity: a meta-analysis. Pharmacotherapy. 2004. 24(5):584–591.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-atherosclerotic effects of perilla oil in rabbits fed a high-cholesterol diet
- Effect of Eicosapentaenioc acid and Butyrated hydroxyanisole on Hypercholestrolemic Diet Induced Atherogenesis in Rabbit
- Efficacy of Diet Therapy in Korea Hypercholesterolemic Patients
- Short Term Effects of Hypercholesterolemia on Corpus Cavernosal Tissue in Rabbits
- Effects of grape pomace on the antioxidant defense system in diet-induced hypercholesterolemic rabbits