Korean Diabetes J.
2008 Jun;32(3):196-203. 10.4093/kdj.2008.32.3.196.
The Effects of D-Chiro-Inositol on Glucose Metabolism in 3T3-L1 Cells
- Affiliations
-
- 1Department of Internal Medicine, Eulji University School of Medicine, Korea.
- 2Korea Association of Health Promotion, Korea.
- 3Department of Internal Medicine, Chungnam National University School of Medicine, Korea.
- KMID: 2298090
- DOI: http://doi.org/10.4093/kdj.2008.32.3.196
Abstract
-
BACKGROUND: The target of the treatment of metabolic syndrome and diabetes is an improvement of insulin resistance. D-chiro-inositol (DCI) plays a role in a phospholipid mediating intracellular insulin action. In the previous studies, the urine level of DCI were decreased in the diabetic animal with insulin resistance. Some clinical studies showed that DCI improved a glucose level and HbA1c. Therefore we studied the relationship between DCI and glucose metabolism, especially insulin resistance.
METHODS
To investigate the mechanism of DCI affecting the glucose metabolism, we examined the effects of DCI on 2-deoxyglucose uptake, gene expression of adipocytokines and AMPK pathway by using RT-PCR and western blot in 3T3-L1 cells.
RESULTS
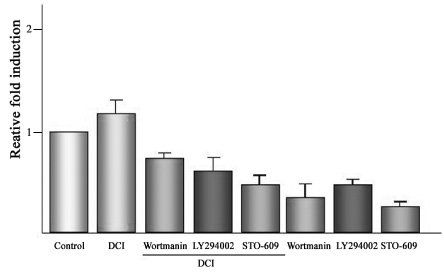
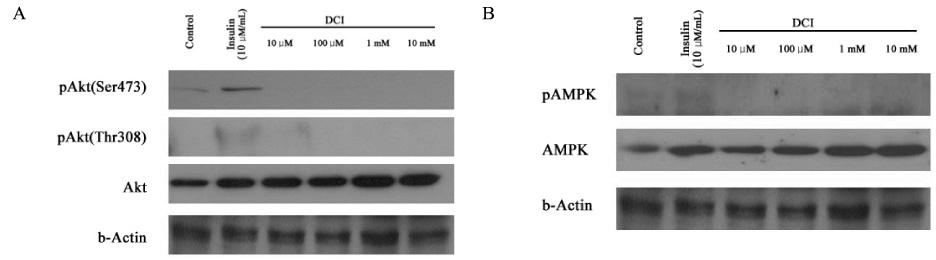
Insulin-stimulated 2-deoxyglucose uptake increased in DCI-treated cells by about 1.2-fold (relative to the control) and was inhibited by phosphoinositide 3-kinase (PI3 Kinase) inhibitors (Wortmanin, LY294002) and AMPK inhibitor (STO-609). In Western blot analysis, it didn't show the difference of phosphorylation of Akt and AMPK between DCI-treated group and control in 3T3-L1 cells. However, DCI decreased the gene expression of resistin in 3T3-L1 cells.
CONCLUSION
DCI may involve other pathway of insulin signaling, but not PI3 Kinase and AMPK signaling pathways and it may be useful in managing metabolic syndrome by improving insulin resistance through increasing glucose uptake and decreasing resistin relevant to insulin resistance.
MeSH Terms
Figure
Reference
-
1. Reaven GM. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.
Article3. Krentz AJ. Insulin resistance. BMJ. 1996. 313:1385–1389.4. Cefalu WT. Insulin resistance: cellular and clinical concepts. Exp Biol Med. 2001. 226:13–26.
Article5. Mlinar B, Marc J, Janez A, Pfeifer M. Molecular mechanisms of insulin resistance and associated diseases. Clinica Chimica Acta. 2007. 375:20–35.
Article6. Moller DE, Bjorbaek C, Vidal-Puig A. Candidate genes for insulin resistance. Diabetes car. 1996. 19:396–400.
Article7. Reaven GM. Pathophysiology of insulin resistance in human disease. Physiol Rev. 1995. 75:473–486.
Article8. DeFronzo RA, Bonnadonna RC, Ferrannini E. Pathogenesis of NIDDM. A ballanced overview. Diabetes Care. 1992. 15:318–368.9. Ferrannini E, Buzziogoli G, Bonadinna R. Insulin resistance in essential hypertension. N Engl J Med. 1987. 317:350–357.
Article10. Shamiss A, Carroll J, Rosenthal T. Insulin reistance in secondary hypertension. Am J Hypertens. 1992. 5:26–28.11. Polonsky KS, Sturis J, Bell GI. Seminars in Medicine of Beth Israel Hospital, Boston. Non-insulin-depenedent diabetes mellitus - genetically programmed failure of the beta cell to compensate for insulin resistance. N Engl J Med. 1996. 334:777–783.12. Bailey CJ, Turner RC. Metformin N Engl. Med. 1996. 334:574–579.13. Olefsky JM. Treatment of insulin resistance with peroxisome proliferator-activated receptor gamma agonist. J Clin Invest. 2000. 106:462–472.14. Jones DR, Varela-Nieto I. The role of glycosyl-phophatidylinositol in signal transduction. Int J Biochem Cell Biol. 1998. 30:313–326.15. Alan RS, Marvin IS, Steven J, Pedero C. Putative mediators of insulin action: Regulation of pyruvate dehydrogenase and adenylate cyclase activities. Proc Natl Acd Sci USA. 1982. 79:3513–3517.16. Ortmeyer HK, Bodkin NL, Hansen BC, Larner J. In vivo D-chiro-inositol activates skeletal muscle glycogen synthase and inactivates glycogen phosphorylase in rhesus monkeys. J Nutr Biochem. 1995. 6:499–503.
Article17. Galasko GT, Abes S, Lilley K, Zhang C, Larner J. Circulating factors and insulin resistance. II The action of the novel myo-inositol cyclic 1,2-inositol phosphate phosphoglycan insulin antagonist from human in regulating pyruvate dehydrogenase phosphatase. J Clin Endocrinol Metab. 1996. 81:1051–1057.18. Daughaday WH, Larner J. The renal excretion of inositol in normal and diabetic human being. J Clin Invest. 1954. 33:326–332.19. Sun TH, Heimark DB, Nguygen T, Nadler JL, Larner J. Both myo-inositol to chiro-inositol epimerase activates and chiro-inositol to myo-inositol ratios are decreased in tissues of GK type 2 diabetic rats compared Wistar controls. Biochem Biophys Biophys Commun. 2002. 293:1092–1098.20. Kennigton AS, Hill CR, Craig J, Bogardus CR, Raz I, Ortmeyer HK. Low urinary chiro-inositol excretion in noninsulin-dependent diabetes mellitus. N Engl J Med. 1990. 323:373–378.21. Bates SH, Jones RB, Bailey CJ. Insulin-like effect of pinitol. Br J Pharmacol. 2000. 130:1944–1948.
Article22. Ostlund RE JR, McGill JB, Herskowitz I, Kipnis DM, Santiago JV. D-Chiro-Inositol metabolism in diabetes mellitus. Proc Natl Acad Sci USA. 1993. 90:9988–9992.
Article23. Shashkin PN, Shashkina EF, Fernqvist-Forbes E, Zhou YP, Grill V. Insulin mediators in man: effects of glucose ingestion and insulin resistance. Diabetologia. 1997. 40:557–563.
Article24. Larner J, Allan G, Kessier C, Reamer P, Gunn R, Huang LC. Phosphoinositol glycan derived mediators and insulin resistance. Prospects for diagnosis and therapy. J Basic Clin Physiol Pharmacol. 1998. 9:127–137.
Article25. Asplin I, Galasko G, Larner J. chiro-inositol deficiency and insulin resistance: A comparison of the chiro -inositol- and the myo-inositol-containg insulin mediators isolated from urine, hemodialysate, and muscle of control and type II diabetic subjects. Proc Natl Acad Sci USA. 1993. 90:5924–5928.26. Orlicky DJ, Lieber JG, Morin CL, Evans RM. Synthesis and accumulation of a receptor regulatory protein associated with lipid droplet accumulation in 3T3-L1 cells. J Lipid Res. 1998. 39:1152–1161.
Article27. Nia JB, Roland G, David EJ. Regulated transport of the glucose transporter GLUT4 Nature molecula. biology. 2002. 3:267–277.28. Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature. 2001. 414:799–806.
Article29. Kido Y, Nakae J, Accili D. The Insulin Receptor and Its Cellular Targets. J Clin Enodocrinol Metab. 2001. 86:972–979.
Article30. Robert VF. Insulin-Sensitive Phospholipid Signaling System and Glucose Transport. Update II. Exp Biol Med Vol. 2001. 226:283–295.31. Chen H. Cellular inflammatory response: Novel insights for obesity and insulin resistance. Pharmacol Res. 2006. 53:469–477.32. Zhao YF, Feng DD, Chen C. Contribution of adipocyte-derived factors to beta-cell dysfunction in diabetes. Int J Biochem Cell Biol. 2006. 38:804–819.
Article33. Ryu ST, Park SO, Kim SH. The Relation of Serum Adiponectin and Resistin Concentrations with Metabolic Risk Factors. J Kor Soc Endocrinol. 2005. 20:444–451.
Article34. Davis A, Christinansen M, Horoxitz JF, Klein S, Hellerstein MK. Effect of pinitol treatment on insulin action in subjects with insulin resistance. Diabetes Care. 2000. 23:1000–1005.
Article35. Kim JI, Kim JC, Kang MJ, Lee MS, Kim JJ. Effects of pinitol isolated from soybeans on glycemic control and cardiovascular risk factors in Korean patients with type II diabetes mellitus: a randomized controlled study. Eur J Clin Nutr. 2005. 59:456–458.36. Kang MJ, Kim JI, Yoon SY, Kim JC, Cha IJ. Pinitol from soybeans postprandial blood glucose in patients with type 2 diabetes mellitus. J Med Food. 2006. 9:182–186.38. Kahn BB, Alquier T, Carling D, Hardie DG. AMP-activated protein kinase: Ancient energy gauge provides clues to modern understanding of metabolism. Cell metab. 2005. 1:15–25.
Article39. Ronti T, Lupattelli G, Mannarino E. The endocrine function of adipose tissue: an update. Clin Endocrinol. 2006. 64:335–365.
Article40. Widajaja A, Stratton IM, Horn M, Holman RR, Turner R. Plasma leptin, obesity, and plasma insulin in type 2 diabetics. J Clin Endocrinol Metab. 1997. 82:654–657.41. Tanizawa Y, Okuya S, Ishihara H, Asano T, Yada T. Direct stimulation of basal insulin secretion from isolated rat pancreatic beta cells. Endocrinology. 1997. 138:4513–4516.42. McTernan CL, McTernan PG, Harte AL, Levick PI, Barnett AH. Resistin, central obesity, and type 2 diabetes. Lancet. 2002. 359:46–47.
Article43. Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR. The hormone resistin link obesity to diabetes. Nature. 2001. 259:46–47.44. Rajala MW, Obici S, Scherer PE, Rossetti L. Adipose-derived resistin and gut-derived resistin-like molecule-beta selectively impair insulin action on glucose production. J Clin Invest. 2003. 111:225–230.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determination of Urinary Myo-/Chiro-Inositol Ratios from Korean Diabetes Patients
- Berberine reduces the expression of adipogenic enzymes and inflammatory molecules of 3T3-L1 adipocyte
- The clinical study to evaluate the safety and efficacy of D-chiro-inositol in patients with type 2 diabetes
- NF-kappaB is involved in the TNF-alpha induced inhibition of the differentiation of 3T3-L1 cells by reducing PPARg expression
- Restoration of the adipogenic gene expression by naringenin and naringin in 3T3-L1 adipocytes