Korean J Crit Care Med.
2015 Aug;30(3):218-221. 10.4266/kjccm.2015.30.3.218.
Management of Cyanide Intoxication with Extracorporeal Membrane Oxygenation and Continuous Renal Replacement Therapy
- Affiliations
-
- 1Department of Neurology, Ewha Womans University School of Medicine, Mokdong Hospital, Seoul, Korea.
- 2Department of Emergency Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- 3Department of Anesthesiology, Ewha Womans University Mokdong Hospital, Seoul, Korea. sicuab@hotmail.com
- KMID: 2227653
- DOI: http://doi.org/10.4266/kjccm.2015.30.3.218
Abstract
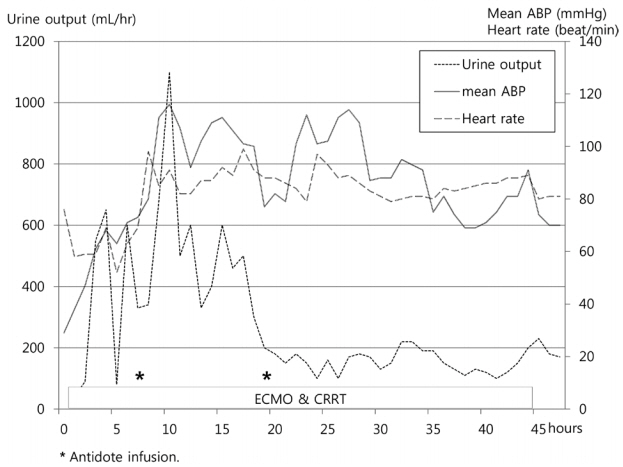
- Cyanide intoxication results in severe metabolic acidosis and catastrophic prognosis with conventional treatment. Indications of extracorporeal membrane oxygenation (ECMO) and continuous renal replacement therapy (CRRT) are expanding to poisoning cases. A 50-year-old male patient arrived in the emergency room due to mental change after ingestion of cyanide as a suicide attempt 30 minutes prior. He was comatose, and brain stem reflexes were absent. Initial laboratory analysis demonstrated severe metabolic acidosis with increased lactic acid of 25 mM/L. Shock and acidosis were not corrected despite a large amount of fluid resuscitation with highdose norepinephrine and continuous renal replacement therapy. We decided to apply ECMO and CRRT to allow time for stabilization of hemodynamic status. After administration of antidote infusion, although the patient had the potential to progress to brain death status, vital signs were improved with correction of acidosis. We considered the evaluation for organ donation. We report a male patient who showed typical cyanide intoxication as lethal metabolic acidosis and cardiac impairment, and the patient recovered after antidote administration during vital organ support through ECMO and CRRT.
Keyword
MeSH Terms
-
Acidosis
Brain Death
Brain Stem
Coma
Cyanides
Eating
Emergency Service, Hospital
Extracorporeal Membrane Oxygenation*
Hemodynamics
Humans
Lactic Acid
Male
Middle Aged
Norepinephrine
Organ Transplantation
Poisoning
Prognosis
Reflex
Renal Replacement Therapy*
Resuscitation
Shock
Suicide
Tissue and Organ Procurement
Vital Signs
Cyanides
Lactic Acid
Norepinephrine
Figure
Reference
-
References
1. Reade MC, Davies SR, Morley PT, Dennett J, Jacobs IC; Australian Resuscitation Council. Review article: management of cyanide poisoning. Emerg Med Australas. 2012; 24:225–38.
Article2. Auzinger GM, Scheinkestel CD. Successful extracorporeal life support in a case of severe flecainide intoxication. Crit Care Med. 2001; 29:887–90.
Article3. Sauer SW, Keim ME. Hydroxocobalamin: improved public health readiness for cyanide disasters. Ann Emerg Med. 2001; 37:635–41.
Article4. Mitchell BL, Bhandari RK, Bebarta VS, Rockwood GA, Boss GR, Logue BA. Toxicokinetic profiles of α-ketoglutarate cyanohydrin, a cyanide detoxification product, following exposure to potassium cyanide. Toxicol Lett. 2013; 222:83–9.
Article5. Lee SW, Kim JS. Antidotes of cyanide intoxication. J Korean Med Assoc. 2013; 56:1076–83.
Article6. Rachinger J, Fellner FA, Stieglbauer K, Trenkler J. MR changes after acute cyanide intoxication. AJNR Am J Neuroradiol. 2002; 23:1398–401.7. Masson R, Colas V, Parienti JJ, Lehoux P, Massetti M, Charbonneau P, et al. A comparison of survival with and without extracorporeal life support treatment for severe poisoning due to drug intoxication. Resuscitation. 2012; 83:1413–7.
Article8. Ravishankar DK, Kashi SH, Lam FT. Organ transplantation from donor who died of cyanide poisoning: a case report. Clin Transplant. 1998; 12:142–3.9. Snyder JW, Unkle DW, Nathan HM, Yang SL. Successful donation and transplantation of multiple organs from a victim of cyanide poisoning. Transplantation. 1993; 55:425–7.
Article10. Barkoukis TJ, Sarbak CA, Lewis D, Whittier FC. Multiorgan procurement from a victim of cyanide poisoning. A case report and review of the literature. Transplantation. 1993; 55:1434–6.11. Wood DM, Dargan PI, Jones AL. Poisoned patients as potential organ donors: postal survey of transplant centres and intensive care units. Crit Care. 2003; 7:147–54.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An adolescent female with intentional ingestion of a large amount of metformin requiring extracorporeal membrane oxygenation and continuous renal replacement therapy
- Simultaneous Extracorporeal Membrane Oxygenation, Renal Replacement Therapy, and Plasma Exchange for Thrombocytopenia-Associated Multiple Organ Failure
- Continuous Renal Replacement Therapy in Infants and Neonates
- Anesthetic management including extracorporeal membrane oxygenation therapy of liver transplant recipient with life-threatening hypoxemia: a case report
- Extracorporeal Membrane Oxygenation and Continuous Renal Replacement Therapy for Treatment of Calcium Channel Blockers, Angiotensin II Receptor Blockers, and Metformin Overdose