Korean Circ J.
2012 Mar;42(3):164-172. 10.4070/kcj.2012.42.3.164.
Prognostic Impact of Baseline High-Sensitivity C-Reactive Protein in Patients With Acute Myocardial Infarction Undergoing Percutaneous Coronary Intervention Based on Body Mass Index
- Affiliations
-
- 1Department of Cardiovascular Medicine, Chonnam National University College of Medicine, Gwangju, Korea. myungho@chollian.net
- 2Department of Cardiology, Apollo Gleneagles Hospital, Kolkata, India.
- 3Department of Cardiology, Chungbuk National University College of Medicine, Daejeon, Korea.
- 4Department of Cardiovascular Medicine, Kyunghee University College of Medicine, Seoul, Korea.
- 5Department of Cardiology, Yeungnam University College of Medicine, Daegu, Korea.
- 6The Brain Korea 21 of Chonnam National University, Gwangju, Korea.
- KMID: 2225030
- DOI: http://doi.org/10.4070/kcj.2012.42.3.164
Abstract
- BACKGROUND AND OBJECTIVES
Serum high sensitivity C-reactive protein (hs-CRP) is a marker of inflammation and may lead to the development of atherosclerosis, adversely affecting mortality. The aim of this study was to evaluate the relationship between baseline hs-CRP level and 12-month clinical outcomes in patients with acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI) according to their body mass index (BMI) status.
SUBJECTS AND METHODS
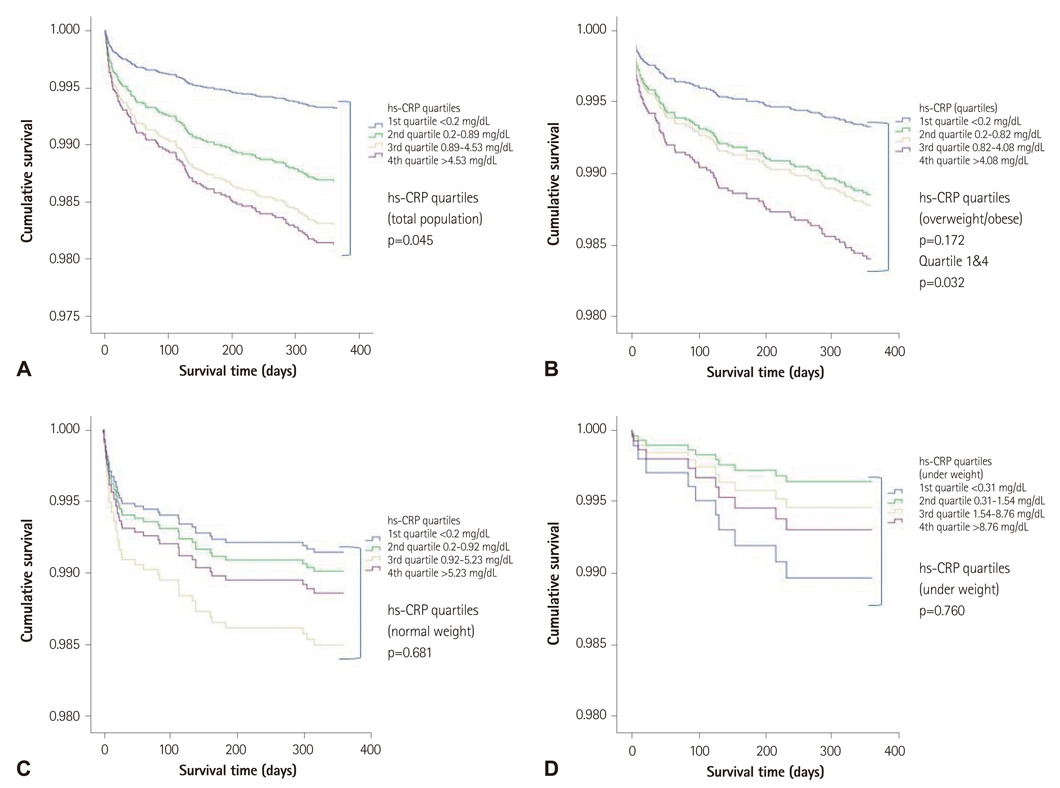
Using data from the Korea Acute Myocardial Infarction Registry from November 2005 to September 2008, a total of 8174 consecutive AMI patients were studied. Cox proportional hazard model revealed that higher baseline levels of hs-CRP was associated with 12-month all-cause mortality (p=0.045). To further understand this association, patients were divided into 3 groups based on their body mass index: 1) overweight/obese, 2) normal weight, and 3) underweight patients. Then each group was stratified into quartiles based on their hs-CRP.
RESULTS
In overweight/obese patients, Cox model showed significant association of hs-CRP with 12-month mortality when adjusted for age and gender (p<0.001), however, after adjustment with multiple covariates, mortality was highest in the 4th quartile {HR 2.382, (1.079-5.259), p=0.032} though statistically insignificant (p=0.172). We observed no significant association of serum hs-CRP with 12-month mortality in normal weight (p=0.681) and underweight (p=0.760) patients.
CONCLUSION
Higher baseline hs-CRP level (> or =4.08 mg/dL) in overweight/obese AMI patients showed significant association with 12-month all-cause mortality independent of other prognostic markers.
MeSH Terms
Figure
Reference
-
1. Koenig W, Khuseyinova N, Baumert J, Meisinger C. Prospective study of high-sensitivity C-reactive protein as a determinant of mortality: results from the MONICA/KORA Augsburg Cohort Study, 1984-1998. Clin Chem. 2008. 54:335–342.2. Marsik C, Kazemi-Shirazi L, Schickbauer T, et al. C-reactive protein and all-cause mortality in a large hospital-based cohort. Clin Chem. 2008. 54:343–349.3. Kang WY, Jeong MH, Ahn YK, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol. 2010. 55:84–91.4. Devaraj S, O'Keefe G, Jialal I. Defining the proinflammatory phenotype using high sensitive C-reactive protein levels as the biomarker. J Clin Endocrinol Metab. 2005. 90:4549–4554.5. Noh HJ, Kwon NH, Joo SB. Severity of coronary atherosclerosis; influence of mtabolic syndrome risk factor clustering and hs-CRP. Korean Circ J. 2006. 36:802–808.6. Sim DS, Jeong MH, Kang JC. Current management of acute myocardial infarction: experience from the Korea Acute Myocardial Infarction Registry. J Cardiol. 2010. 56:1–7.7. Lee KH, Jeong MH, Ahn YK. Sex differences of the clinical characteristics and early management in the Korea Acute Myocardial Infarction Registry. Korean Circ J. 2007. 37:64–71.8. Sim DS, Kim JH, Jeong MH. Differences in clinical outcomes between patients with ST-elevation versus non-ST-elevation acute myocardial infarction in Korea. Korean Circ J. 2009. 39:297–303.9. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. 363:157–163.10. Apple FS, Wu AH, Jaffe AS. European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J. 2002. 144:981–986.11. Kini AS. Coronary angiography, lesion classification and severity assessment. Cardiol Clin. 2006. 24:153–162. v12. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002. 347:1557–1565.13. Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation. 2003. 107:391–397.14. Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003. 107:363–369.15. Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol. 1999. 19:972–978.16. Bahceci M, Gokalp D, Bahceci S, Tuzcu A, Atmaca S, Arikan S. The correlation between adiposity and adiponectin, tumor necrosis factor alpha, interleukin-6 and high sensitivity C-reactive protein levels: is adipocyte size associated with inflammation in adults? J Endocrinol Invest. 2007. 30:210–214.17. Bastard JP, Maachi M, Van Nhieu JT, et al. Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro. J Clin Endocrinol Metab. 2002. 87:2084–2089.18. Lagathu C, Bastard JP, Auclair M, Maachi M, Capeau J, Caron M. Chronic interleukin-6 (IL-6) treatment increased IL-6 secretion and induced insulin resistance in adipocyte: prevention by rosiglitazone. Biochem Biophys Res Commun. 2003. 311:372–379.19. Verma S, Li SH, Badiwala MV, et al. Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation. 2002. 105:1890–1896.20. Wang CH, Li SH, Weisel RD, et al. C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation. 2003. 107:1783–1790.21. Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999. 282:2131–2135.22. De Sutter J, de Buyzere M, Gheeraert P, et al. Fibrinogen and C-reactive protein on admission as markers of final infarct size after primary angioplasty for acute myocardial infarction. Atherosclerosis. 2001. 157:189–196.23. Saito M, Ishimitsu T, Minami J, Ono H, Ohrui M, Matsuoka H. Relations of plasma high-sensitivity C-reactive protein to traditional cardiovascular risk factors. Atherosclerosis. 2003. 167:73–79.24. Ryu SY, Lee YS, Park J, Kang MG, Kim KS. Relations of plasma high-sensitivity C-reactive protein to various cardiovascular risk factors. J Korean Med Sci. 2005. 20:379–383.25. Araújo JP, Lourenço P, Azevedo A, et al. Prognostic value of high-sensitivity C-reactive protein in heart failure: a systematic review. J Card Fail. 2009. 15:256–266.26. Bursi F, Weston SA, Killian JM, Gabriel SE, Jacobsen SJ, Roger VL. C-reactive protein and heart failure after myocardial infarction in the community. Am J Med. 2007. 120:616–622.27. Alonso-Martínez JL, Llorente-Diez B, Echegaray-Agara M, Olaz-Preciado F, Urbieta-Echezarreta M, González-Arencibia C. C-reactive protein as a predictor of improvement and readmission in heart failure. Eur J Heart Fail. 2002. 4:331–336.28. Asakura M, Ueda Y, Yamaguchi O, et al. Extensive development of vulnerable plaques as a pan-coronary process in patients with myocardial infarction: an angioscopic study. J Am Coll Cardiol. 2001. 37:1284–1288.29. Tataru MC, Heinrich J, Junker R, et al. C-reactive protein and the severity of atherosclerosis in myocardial infarction patients with stable angina pectoris. Eur Heart J. 2000. 21:1000–1008.30. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. N Engl J Med. 2005. 352:29–38.31. Rao AD, Milbrandt EB. To JUPITER and beyond: statins, inflammation, and primary prevention. Crit Care. 2010. 14:310.32. Sever PS, Dahlöf B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial: Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003. 361:1149–1158.33. De Beer FC, Hind CR, Fox KM, Allan RM, Maseri A, Pepys MB. Measurement of serum C-reactive protein concentration in myocardial ischaemia and infarction. Br Heart J. 1982. 47:239–243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prognostic Impact of Hypertriglyceridemia and Abdominal Obesity in Acute Myocardial Infarction Patients Underwent Percutaneous Coronary Intervention
- The Impact of Ischemic Time on the Predictive Value of High-Sensitivity C-Reactive Protein in ST-Segment Elevation Myocardial Infarction Patients Treated by Primary Percutaneous Coronary Intervention
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- 'Obesity Paradox' in Myocardial Infarction Patients
- Cardiac arrest due to an unexpected acute myocardial infarction during head and neck surgery: A case report