Infect Chemother.
2014 Dec;46(4):269-273. 10.3947/ic.2014.46.4.269.
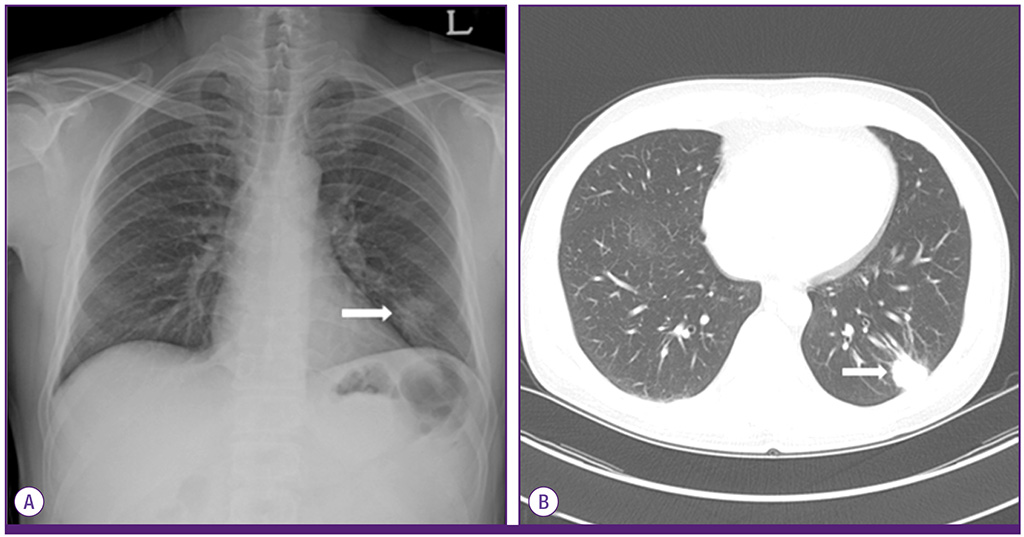
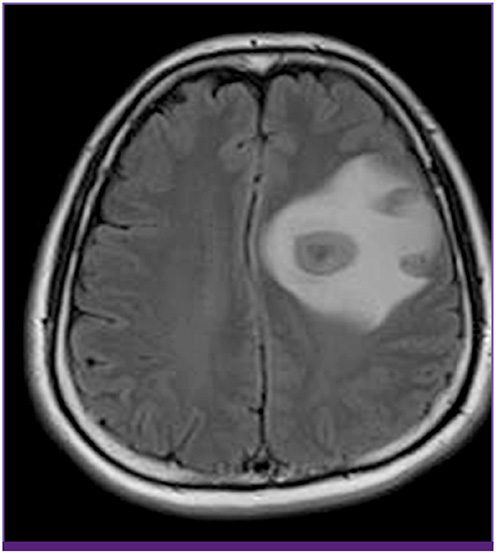
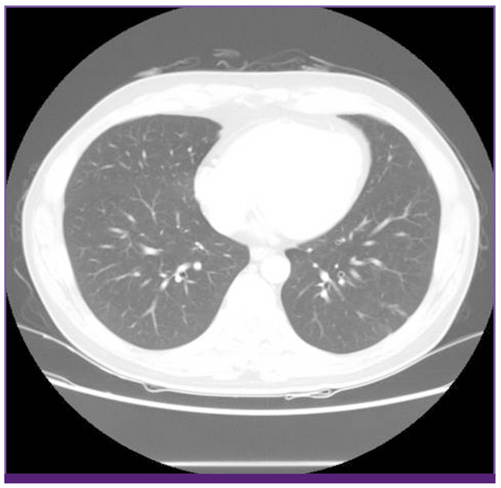
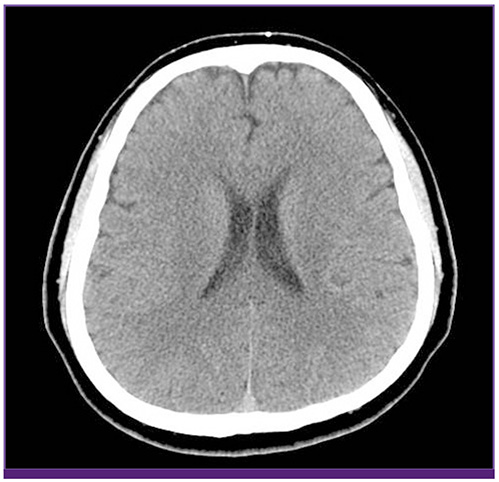
A Case of Disseminated Infection due to Actinomyces meyeri Involving Lung and Brain
- Affiliations
-
- 1Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. soleemd@amc.seoul.kr
- 2Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2170498
- DOI: http://doi.org/10.3947/ic.2014.46.4.269
Abstract
- Actinomyces meyeri is rarely isolated in cases of actinomycosis. The identification of A. meyeri had historically been difficult and unreliable. With the recent development of 16S ribosomal RNA (16S rRNA) sequencing, Actinomyces species such as A. meyeri can be isolated much more reliably. A. meyeri often causes disseminated disease, which can be secondary to frequent pulmonary infections. A penicillin-based regimen is the mainstay of A. meyeri treatment, with a prolonged course usually required. Here, we report a case of pulmonary actinomycosis with brain abscess caused by A. meyeri that was initially thought to represent lung cancer with brain metastasis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Olecranon Osteomyelitis due to Actinomyces meyeri: Report of a Culture-Proven Case
Ji-Yeon Kim, Eun Kyung Kang, Song Mi Moon, Yiel-Hea Seo, Juhyeon Jeong, Hyuni Cho, Dongki Yang, Yoon Soo Park
Infect Chemother. 2016;48(3):234-238. doi: 10.3947/ic.2016.48.3.234.
Reference
-
1. Fazili T, Blair D, Riddell S, Kiska D, Nagra S. Actinomyces meyeri infection: case report and review of the literature. J Infect. 2012; 65:357–361.
Article2. Colmegna I, Rodriguez-Barradas M, Rauch R, Clarridge J, Young EJ. Disseminated Actinomyces meyeri infection resembling lung cancer with brain metastases. Am J Med Sci. 2003; 326:152–155.
Article3. Apothéloz C, Regamey C. Disseminated infection due to Actinomyces meyeri: case report and review. Clin Infect Dis. 1996; 22:621–625.4. Marty HU, Wüst J. Disseminated actinomycosis caused by Actinomyces meyeri. Infection. 1989; 17:154–155.
Article5. Kuijper EJ, Wiggerts HO, Jonker GJ, Schaal KP, de Gans J. Disseminated actinomycosis due to Actinomyces meyeri and Actinobacillus actinomycetemcomitans. Scand J Infect Dis. 1992; 24:667–672.
Article6. Song EH, Kwon HH, Jang EY, Kim MN, Lee SO, Kim YS, Woo JH. A case of brain abscess caused by Actinomyces meyeri and Haemophilus aphrophilus. Korean J Med. 2008; 74:Suppl 1. S144–S148.7. Park YM, Won IS, Kim JI, Cho HJ, Seo JG, Kim JY, Kim EY, Park SH, Park YS, Seo YH, Cho YK. A case of central nervous system actinomycosis presenting as brain abscess. Infect Chemother. 2009; 41:249–252.
Article8. Ham HY, Jung S, Jung TY, Heo SH. Cerebral actinomycosis: unusual clinical and radiological findings of an abscess. J Korean Neurosurg Soc. 2011; 50:147–150.
Article9. Kolbert CP, Persing DH. Ribosomal DNA sequencing as a tool for identification of bacterial pathogens. Curr Opin Microbiol. 1999; 2:299–305.
Article10. Kim OS, Cho YJ, Lee K, Yoon SH, Kim M, Na H, Park SC, Jeon YS, Lee JH, Yi H, Won S, Chun J. Introducing EzTaxon-e: a prokaryotic 16S rRNA gene sequence database with phylotypes that represent uncultured species. Int J Syst Evol Microbiol. 2012; 62:716–721.
Article11. Clinical and laboratory standards institute (CLSI). Interpretive criteria for identification of bacteria and fungi by DNA target sequencing; approved guideline. MM18-A. Wayne, PA: CLSI;2008.12. Smego RA, Foglia G. Actinomycosis. Clin Infect Dis. 1998; 26:1255–1261. quiz 1262-3.
Article13. Pordy RC. Lumpy jaw due to Actinomyces meyerii: report of the first case and review of the literature. Mt Sinai J Med. 1988; 55:190–193.14. Hall V, Talbot PR, Stubbs SL, Duerden BI. Identification of clinical isolates of actinomyces species by amplified 16S ribosomal DNA restriction analysis. J Clin Microbiol. 2001; 39:3555–3562.
Article15. Holdeman LV, Cato EP, Moore WE. Anaerobe laboratory manual. 4th ed. Blacksburg, Virginia: Virginia Polytechnic Institute and State University;1977. p. 61–62.16. Hennrikus EF, Pederson L. Disseminated actinomycosis. West J Med. 1987; 147:201–204.17. Russo T. Agents of actinomycosis. Mandell, Douglas and Bennett's principles and practice of infectious diseases. 7th ed. Philadelphia, PA: Churchill Livingstone Elsevier;2010. p. 209–219.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Olecranon Osteomyelitis due to Actinomyces meyeri: Report of a Culture-Proven Case
- Disseminated Invasive Mycobacterium marinum Infection Involving the Lung of a Patient with Diabetes Mellitus
- A Case with Mixed Infection of Actinomyces and Aspergillus in the Lung
- Disseminated aspergillosis in malignant lymphoma: a case report
- A Case of Disseminated Nocardiosis in Kidney Transplant Recipient