Infect Chemother.
2016 Sep;48(3):234-238. 10.3947/ic.2016.48.3.234.
Olecranon Osteomyelitis due to Actinomyces meyeri: Report of a Culture-Proven Case
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Gachon University School of Medicine, Gil Medical Center, Incheon, Korea.
- 3Department of Laboratory Medicine, Gachon University School of Medicine, Gil Medical Center, Incheon, Korea.
- 4Department of Pathology, Gachon University School of Medicine, Gil Medical Center, Incheon, Korea.
- 5Department of Physiology, Gachon University School of Medicine, Gil Medical Center, Incheon, Korea.
- 6Division of Infectious Diseases, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea. ysparkok2@gmail.com
- KMID: 2466439
- DOI: http://doi.org/10.3947/ic.2016.48.3.234
Abstract
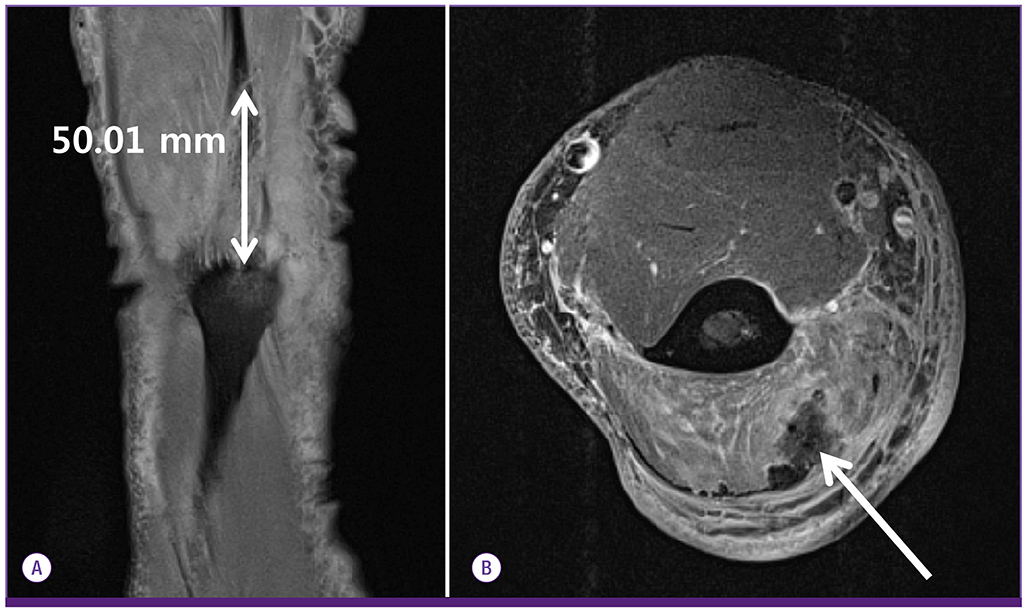
- Actinomyces meyeri is a Gram positive, strict anaerobic bacterium, which was first described by Meyer in 1911. Primary actinomycotic osteomyelitis is rare and primarily affects the cervicofacial region, including mandible. We present an unusual case of osteomyelitis of a long bone combined with myoabscess due to A. meyeri. A 70-year-old man was admitted for pain and pus discharge of the right elbow. Twenty-five days before admission, he had hit his elbow against a table. MRI of the elbow showed a partial tear of the distal triceps tendon and myositis. He underwent open debridement and partial bone resection for the osteomyelitis of the olecranon. Biopsy showed no sulfur granules, but acute and chronic osteomyelitis. The excised tissue grew A. meyeri and Peptoniphilus asaccharolyticus. Intravenous ceftriaxone was administered and switched to oral amoxicillin. Infection of the extremities of actinomycosis often poses diagnostic difficulties, but it should not be neglected even when the characteristic pathologic findings are not present.
Keyword
MeSH Terms
Figure
Reference
-
1. Smego RA Jr, Foglia G. Actinomycosis. Clin Infect Dis. 1998; 26:1255–1261.
Article2. Russo TA. Agents of Actinomycosis. In : Bennett JE, Dolin R, Blaser MJ, editors. Principles and Practice of Infectious Diseases. 8th ed. Philadelphia: Elsevier Saunders;2015. p. 2864–2872.3. Lee MJ, Ha YE, Park HY, Lee JH, Lee YJ, Sung KS, Kang CI, Chung DR, Song JH, Peck KR. Osteomyelitis of a long bone due to Fusobacterium nucleatum and Actinomyces meyeri in an immunocompetent adult: a case report and literature review. BMC Infect Dis. 2012; 12:161.4. Bettesworth J, Gill K, Shah J. Primary actinomycosis of the foot: a case report and literature review. J Am Col Certif Wound Spec. 2009; 1:95–100.
Article5. Pang DK, Abdalla M. Osteomyelitis of the foot due to Actinomyces meyeri: a case report. Foot Ankle. 1987; 8:169–171.6. Padhi S, Dash M, Turuk J, Sahu R, Panda P. Primary actinomycosis of hand. Adv Biomed Res. 2014; 3:225.
Article7. Reiner SL, Harrelson JM, Miller SE, Hill GB, Gallis HA. Primary actinomycosis of an extremity: a case report and review. Rev Infect Dis. 1987; 9:581–589.
Article8. Vandevelde AG, Jenkins SG, Hardy PR. Sclerosing osteomyelitis and Actinomyces naeslundii infection of surrounding tissues. Clin Infect Dis. 1995; 20:1037–1039.
Article9. Fazili T, Blair D, Riddell S, Kiska D, Nagra S. Actinomyces meyeri infection: case report and review of the literature. J Infect. 2012; 65:357–361.
Article10. Park HJ, Park KH, Kim SH, Sung H, Choi SH, Kim YS, Woo JH, Lee SO. A case of disseminated infection due to Actinomyces meyeri involving lung and brain. Infect Chemother. 2014; 46:269–273.
Article11. Hall V, Talbot PR, Stubbs SL, Duerden BI. Identification of clinical isolates of actinomyces species by amplified 16S ribosomal DNA restriction analysis. J Clin Microbiol. 2001; 39:3555–3562.
Article12. Holm P. Studies on the aetiology of human actinomycosis. The “other” microbes of actinomycosis and their importance. Acta Pathol Microbiol Scand. 1950; 27:736–751.13. Smego RA Jr. Actinomycosis of the central nervous system. Rev Infect Dis. 1987; 9:855–865.
Article14. Murdoch DA. Gram-positive anaerobic cocci. Clin Microbiol Rev. 1998; 11:81–120.
Article15. Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, Gleizal A, Boussel L, Laurent F, Braun E, Chidiac C, Ader F, Ferry T. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014; 7:183–197.16. Fass RJ, Scholand JF, Hodges GR, Saslaw S. Clindamycin in the treatment of serious anaerobic infections. Ann Intern Med. 1973; 78:853–859.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Disseminated Infection due to Actinomyces meyeri Involving Lung and Brain
- Osteomyelitis Resulting from Chronic Septic Olecranon Bursitis: Report of Two Cases
- Primary Sternal Osteomyelitis Caused by Actinomyces israelii
- Separation of Unfused Olecranon Epiphysis in an Adult Baseball Pitcher: A Case Report
- Nonunion of a Stress Fracture Through the Olecranon Epiphyseal Plate in an Adolescent Judo Player: A Case Report