Glia as a Link between Neuroinflammation and Neuropathic Pain
- Affiliations
-
- 1Department of Pharmacology, Brain Science & Engineering Institute, Kyungpook National University School of Medicine, Daegu 700-422, Korea. ksuk@knu.ac.kr
- KMID: 2150733
- DOI: http://doi.org/10.4110/in.2012.12.2.41
Abstract
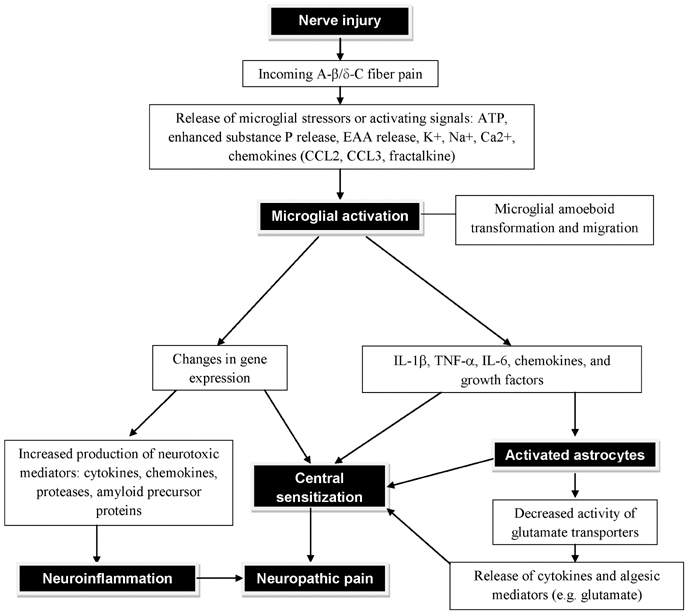
- Contemporary studies illustrate that peripheral injuries activate glial components of the peripheral and central cellular circuitry. The subsequent release of glial stressors or activating signals contributes to neuropathic pain and neuroinflammation. Recent studies document the importance of glia in the development and persistence of neuropathic pain and neuroinflammation as a connecting link, thereby focusing attention on the glial pathology as the general underlying factor in essentially all age-related neurodegenerative diseases. There is wide agreement that excessive glial activation is a key process in nervous system disorders involving the release of strong pro-inflammatory cytokines, which can trigger worsening of multiple disease states. This review will briefly discuss the recent findings that have shed light on the molecular and cellular mechanisms of glia as a connecting link between neuropathic pain and neuroinflammation.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Paeoniflorin ameliorates neuropathic pain-induced depression-like behaviors in mice by inhibiting hippocampal neuroinflammation activated
via TLR4/NF-κB pathway
Hualei Bai, Shize Chen, Tiezheng Yuan, Dongyuan Xu, Songbiao Cui, Xiangdan Li
Korean J Physiol Pharmacol. 2021;25(3):217-225. doi: 10.4196/kjpp.2021.25.3.217.Acute Phase Protein Lipocalin-2 Is Associated with Formalin-induced Nociception and Pathological Pain
Mithilesh Kumar Jha, Sangmin Jeon, Myungwon Jin, Won-Ha Lee, Kyoungho Suk
Immune Netw. 2013;13(6):289-294. doi: 10.4110/in.2013.13.6.289.Gabexate mesilate ameliorates the neuropathic pain in a rat model by inhibition of proinflammatory cytokines and nitric oxide pathway
via suppression of nuclear factor-κB
Seon Hee Oh, Hyun Young Lee, Young Joon Ki, Sang Hun Kim, Kyung Joon Lim, Ki Tae Jung
Korean J Pain. 2020;33(1):30-39. doi: 10.3344/kjp.2020.33.1.30.
Reference
-
1. Kriegstein A, Alvarez-Buylla A. The glial nature of embryonic and adult neural stem cells. Annu Rev Neurosci. 2009. 32:149–184.
Article2. Moalem G, Tracey DJ. Immune and inflammatory mechanisms in neuropathic pain. Brain Res Rev. 2006. 51:240–264.
Article3. Aamodt S. Focus on glia and disease. Nat Neurosci. 2007. 10:1349.
Article4. Watkins LR, Milligan ED, Maier SF. Glial activation: a driving force for pathological pain. Trends Neurosci. 2001. 24:450–455.
Article5. McMahon SB, Cafferty WB, Marchand F. Immune and glial cell factors as pain mediators and modulators. Exp Neurol. 2005. 192:444–462.
Article6. Coull JA, Beggs S, Boudreau D, Boivin D, Tsuda M, Inoue K, Gravel C, Salter MW, De Koninck Y. BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain. Nature. 2005. 438:1017–1021.
Article7. Garrison CJ, Dougherty PM, Kajander KC, Carlton SM. Staining of glial fibrillary acidic protein (GFAP) in lumbar spinal cord increases following a sciatic nerve constriction injury. Brain Res. 1991. 565:1–7.
Article8. Meller ST, Dykstra C, Grzybycki D, Murphy S, Gebhart GF. The possible role of glia in nociceptive processing and hyperalgesia in the spinal cord of the rat. Neuropharmacology. 1994. 33:1471–1478.
Article9. Colburn RW, DeLeo JA, Rickman AJ, Yeager MP, Kwon P, Hickey WF. Dissociation of microglial activation and neuropathic pain behaviors following peripheral nerve injury in the rat. J Neuroimmunol. 1997. 79:163–175.
Article10. Milligan ED, Mehmert KK, Hinde JL, Harvey LO, Martin D, Tracey KJ, Maier SF, Watkins LR. Thermal hyperalgesia and mechanical allodynia produced by intrathecal administration of the human immunodeficiency virus-1 (HIV-1) envelope glycoprotein, gp120. Brain Res. 2000. 861:105–116.
Article11. Chacur M, Milligan ED, Gazda LS, Armstrong C, Wang H, Tracey KJ, Maier SF, Watkins LR. A new model of sciatic inflammatory neuritis (SIN): induction of unilateral and bilateral mechanical allodynia following acute unilateral peri-sciatic immune activation in rats. Pain. 2001. 94:231–244.
Article12. Raghavendra V, Tanga FY, DeLeo JA. Complete Freunds adjuvant-induced peripheral inflammation evokes glial activation and proinflammatory cytokine expression in the CNS. Eur J Neurosci. 2004. 20:467–473.
Article13. Möller T. Neuroinflammation in Huntington's disease. J Neural Transm. 2010. 117:1001–1008.
Article14. Björkqvist M, Wild EJ, Thiele J, Silvestroni A, Andre R, Lahiri N, Raibon E, Lee RV, Benn CL, Soulet D, Magnusson A, Woodman B, Landles C, Pouladi MA, Hayden MR, Khalili-Shirazi A, Lowdell MW, Brundin P, Bates GP, Leavitt BR, Möller T, Tabrizi SJ. A novel pathogenic pathway of immune activation detectable before clinical onset in Huntington's disease. J Exp Med. 2008. 205:1869–1877.
Article15. Garden GA, Möller T. Microglia biology in health and disease. J Neuroimmune Pharmacol. 2006. 1:127–137.
Article16. Weydt P, Möller T. Neuroinflammation in the pathogenesis of amyotrophic lateral sclerosis. Neuroreport. 2005. 16:527–531.
Article17. Block ML, Hong JS. Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog Neurobiol. 2005. 76:77–98.
Article18. Mrak RE, Griffin WS. Interleukin-1, neuroinflammation, and Alzheimer's disease. Neurobiol Aging. 2001. 22:903–908.
Article19. Phillis JW, Horrocks LA, Farooqui AA. Cyclooxygenases, lipoxygenases, and epoxygenases in CNS: their role and involvement in neurological disorders. Brain Res Rev. 2006. 52:201–243.
Article20. Sriram K, O'Callaghan JP. Divergent roles for tumor necrosis factor-alpha in the brain. J Neuroimmune Pharmacol. 2007. 2:140–153.21. Ubogu EE, Cossoy MB, Ransohoff RM. The expression and function of chemokines involved in CNS inflammation. Trends Pharmacol Sci. 2006. 27:48–55.
Article22. Weed DL. The merger of bioethics and epidemiology. J Clin Epidemiol. 1991. 44:Suppl 1. 15S–22S.
Article23. Baptista MJ, Cookson MR, Miller DW. Parkin and alpha-synuclein: opponent actions in the pathogenesis of Parkinson's disease. Neuroscientist. 2004. 10:63–72.
Article24. Gilron I, Watson CP, Cahill CM, Moulin DE. Neuropathic pain: a practical guide for the clinician. CMAJ. 2006. 175:265–275.
Article25. Kielian T. Microglia and chemokines in infectious diseases of the nervous system: views and reviews. Front Biosci. 2004. 9:732–750.
Article26. Ransohoff RM, Glabinski A, Tani M. Chemokines in immune-mediated inflammation of the central nervous system. Cytokine Growth Factor Rev. 1996. 7:35–46.
Article27. Cartier L, Hartley O, Dubois-Dauphin M, Krause KH. Chemokine receptors in the central nervous system: role in brain inflammation and neurodegenerative diseases. Brain Res Brain Res Rev. 2005. 48:16–42.
Article28. Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996. 19:312–318.
Article29. Clayton DF, George JM. Synucleins in synaptic plasticity and neurodegenerative disorders. J Neurosci Res. 1999. 58:120–129.
Article30. Becher B, Prat A, Antel JP. Brain-immune connection: immuno-regulatory properties of CNS-resident cells. Glia. 2000. 29:293–304.
Article31. Scholz J, Woolf CJ. The neuropathic pain triad: neurons, immune cells and glia. Nat Neurosci. 2007. 10:1361–1368.
Article32. Halassa MM, Fellin T, Haydon PG. The tripartite synapse: roles for gliotransmission in health and disease. Trends Mol Med. 2007. 13:54–63.
Article33. Pocock JM, Kettenmann H. Neurotransmitter receptors on microglia. Trends Neurosci. 2007. 30:527–535.
Article34. Watkins LR, Wieseler-Frank J, Milligan ED, Johnston I, Maier SF. Chapter 22 Contribution of glia to pain processing in health and disease. Handb Clin Neurol. 2006. 81:309–323.
Article35. Gwak YS, Kang J, Unabia GC, Hulsebosch CE. Spatial and temporal activation of spinal glial cells: role of gliopathy in central neuropathic pain following spinal cord injury in rats. Exp Neurol. 2012. 234:362–372.
Article36. Julius D, Basbaum AI. Molecular mechanisms of nociception. Nature. 2001. 413:203–210.
Article37. Scholz J, Woolf CJ. Can we conquer pain? Nat Neurosci. 2002. 5:Suppl. 1062–1067.
Article38. Block ML, Zecca L, Hong JS. Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci. 2007. 8:57–69.
Article39. Lobsiger CS, Cleveland DW. Glial cells as intrinsic components of non-cell-autonomous neurodegenerative disease. Nat Neurosci. 2007. 10:1355–1360.
Article40. Vallejo R, Tilley DM, Vogel L, Benyamin R. The role of glia and the immune system in the development and maintenance of neuropathic pain. Pain Pract. 2010. 10:167–184.
Article41. Colburn RW, Rickman AJ, DeLeo JA. The effect of site and type of nerve injury on spinal glial activation and neuropathic pain behavior. Exp Neurol. 1999. 157:289–304.
Article42. Raghavendra V, Tanga F, DeLeo JA. Inhibition of microglial activation attenuates the development but not existing hypersensitivity in a rat model of neuropathy. J Pharmacol Exp Ther. 2003. 306:624–630.
Article43. Ledeboer A, Sloane EM, Milligan ED, Frank MG, Mahony JH, Maier SF, Watkins LR. Minocycline attenuates mechanical allodynia and proinflammatory cytokine expression in rat models of pain facilitation. Pain. 2005. 115:71–83.
Article44. DeLeo JA, Winkelstein BA. Physiology of chronic spinal pain syndromes: from animal models to biomechanics. Spine (Phila Pa 1976). 2002. 27:2526–2537.45. Watkins LR, Hutchinson MR, Milligan ED, Maier SF. "Listening" and "talking" to neurons: implications of immune activation for pain control and increasing the efficacy of opioids. Brain Res Rev. 2007. 56:148–169.
Article46. Wieseler-Frank J, Maier SF, Watkins LR. Glial activation and pathological pain. Neurochem Int. 2004. 45:389–395.
Article47. Ji RR, Suter MR. p38 MAPK, microglial signaling, and neuropathic pain. Mol Pain. 2007. 3:33.
Article48. Zhuang ZY, Gerner P, Woolf CJ, Ji RR. ERK is sequentially activated in neurons, microglia, and astrocytes by spinal nerve ligation and contributes to mechanical allodynia in this neuropathic pain model. Pain. 2005. 114:149–159.
Article49. Dubuisson D, Dennis SG. The formalin test: a quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain. 1977. 4:161–174.
Article50. Abbott FV, Franklin KB, Westbrook RF. The formalin test: scoring properties of the first and second phases of the pain response in rats. Pain. 1995. 60:91–102.
Article51. Puig S, Sorkin LS. Formalin-evoked activity in identified primary afferent fibers: systemic lidocaine suppresses phase-2 activity. Pain. 1996. 64:345–355.
Article52. Tjølsen A, Berge OG, Hunskaar S, Rosland JH, Hole K. The formalin test: an evaluation of the method. Pain. 1992. 51:5–17.
Article53. Colpaert FC. Evidence that adjuvant arthritis in the rat is associated with chronic pain. Pain. 1987. 28:201–222.
Article54. Millan MJ, Członkowski A, Morris B, Stein C, Arendt R, Huber A, Höllt V, Herz A. Inflammation of the hind limb as a model of unilateral, localized pain: influence on multiple opioid systems in the spinal cord of the rat. Pain. 1988. 35:299–312.
Article55. Iadarola MJ, Brady LS, Draisci G, Dubner R. Enhancement of dynorphin gene expression in spinal cord following experimental inflammation: stimulus specificity, behavioral parameters and opioid receptor binding. Pain. 1988. 35:313–326.
Article56. Lao L, Zhang RX, Zhang G, Wang X, Berman BM, Ren K. A parametric study of electroacupuncture on persistent hyperalgesia and Fos protein expression in rats. Brain Res. 2004. 1020:18–29.
Article57. Li K, Lin T, Cao Y, Light AR, Fu KY. Peripheral formalin injury induces 2 stages of microglial activation in the spinal cord. J Pain. 2010. 11:1056–1065.
Article58. Lin T, Li K, Zhang FY, Zhang ZK, Light AR, Fu KY. Dissociation of spinal microglia morphological activation and peripheral inflammation in inflammatory pain models. J Neuroimmunol. 2007. 192:40–48.
Article59. Ren K, Dubner R. Neuron-glia crosstalk gets serious: role in pain hypersensitivity. Curr Opin Anaesthesiol. 2008. 21:570–579.
Article60. Gao YJ, Ji RR. Targeting astrocyte signaling for chronic pain. Neurotherapeutics. 2010. 7:482–493.
Article61. Watkins LR, Hutchinson MR, Ledeboer A, Wieseler-Frank J, Milligan ED, Maier SF. Norman Cousins Lecture. Glia as the "bad guys": implications for improving clinical pain control and the clinical utility of opioids. Brain Behav Immun. 2007. 21:131–146.
Article