J Korean Med Sci.
2014 Sep;29(Suppl 2):S109-S116. 10.3346/jkms.2014.29.S2.S109.
Estimated 24-Hour Urine Sodium Excretion Is Correlated with Blood Pressure in Korean Population: 2009-2011 Korean National Health and Nutritional Examination Survey
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Hallym Kidney Research Institute, Seoul, Korea.
- 2Department of Internal Medicine, Inje University College of Medicine, Seoul, Korea.
- 3Research Institute of Salt and Health, Seoul K-Clinic, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. mednep@snubh.org
- KMID: 2069801
- DOI: http://doi.org/10.3346/jkms.2014.29.S2.S109
Abstract
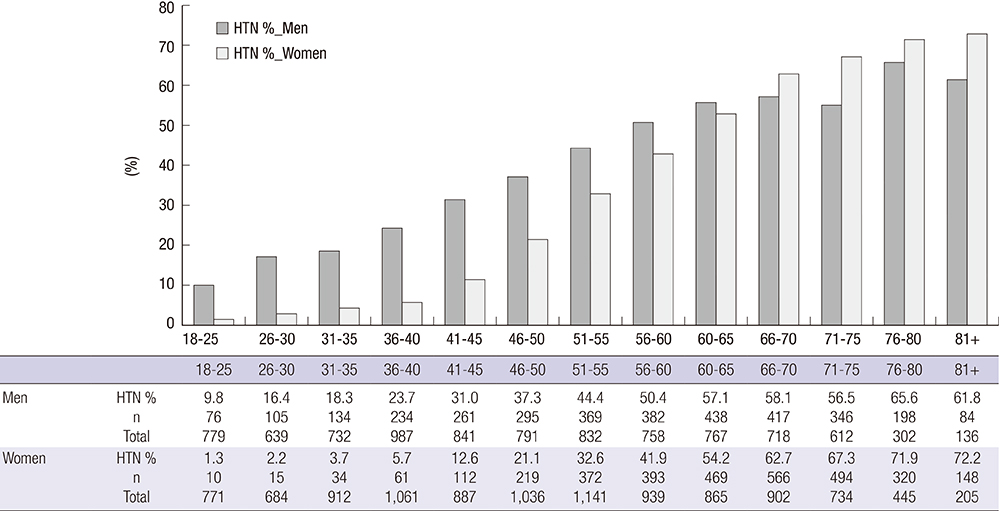
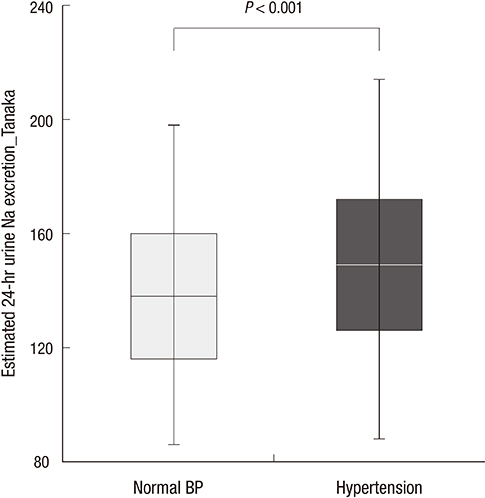
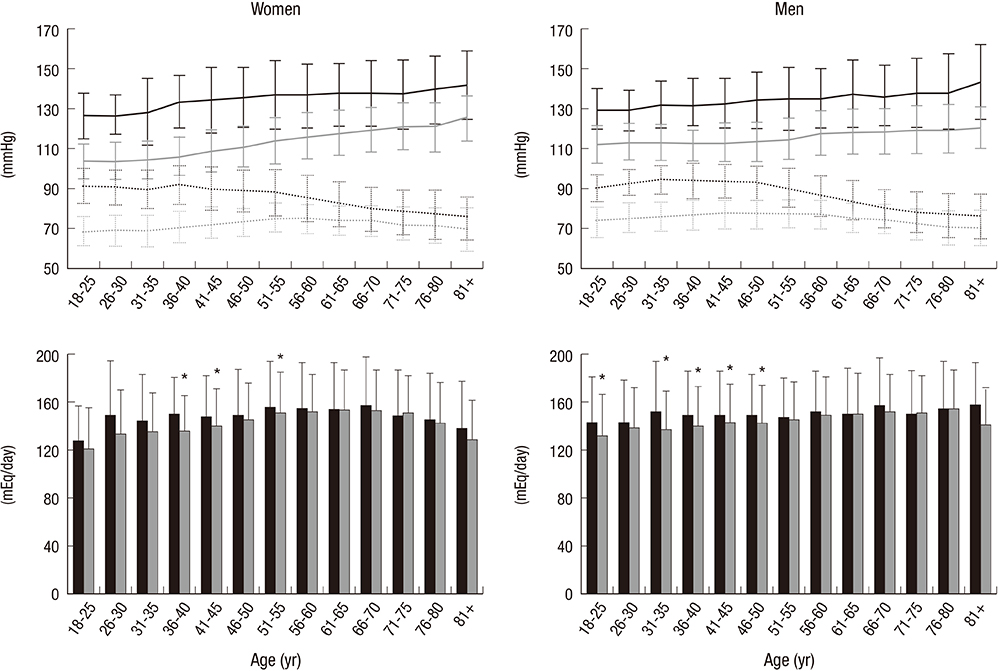
- No large-scale studies have investigated the association between salt intake and hypertension in Korean population. To investigate the relationship of blood pressure to salt consumption, we analyzed data from 19,476 participants in the 2009-2011 Korean National Health and Nutritional Examination Survey (KNHANES). Urinary sodium excretion over 24-hr (24HUNa) was estimated from spot urine tests using Tanaka's equation. The study subjects were stratified into hypertensive and normotensive groups. Hypertensive participants (n=6,552, 33.6%) had higher estimated 24HUNa, 150.4+/-38.8 mEq/day, than normotensive participants, 140.5+/-34.6 mEq/day (P<0.001). The association between 24HUNa and blood pressure outcomes was not affected by adjustment for other risk factors for hypertension (odds ratio 0.001; 95% confidence interval 0.001-0.003; P<0.001). Increases in 24HUNa of 100 mEq/day were associated with a 6.1+/-0.3/2.9+/-0.2 mmHg increase in systolic/diastolic blood pressure in all participants. This effect was stronger in hypertensive participants (increase of 8.1+/-0.5/3.4+/-0.3 mmHg per 100 mEq/day) and smaller in normotensive participants (2.9+/-0.3/1.3+/-0.2 mmHg). These results support recommendations for low salt intake in Korean population to prevent and control adverse blood pressure levels.
Keyword
MeSH Terms
Figure
Reference
-
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010; 303:2043–2050.2. He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002; 16:761–770.3. Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003; 17:471–480.4. Kaplan NM. Primary hypertension: pathogenesis. In : Kaplan NM, editor. Kaplan's clinical hypertension. Philadelphia: Lippincott Williams & Wilkins;2006. p. 50–121.5. Cruz-Coke R, Etcheverry R, Nagel R. Influence of migration on blood-pressure of easter islanders. Lancet. 1964; 1:697–699.6. Ward RH, Chin PG, Prior IA. Tokelau Island Migrant Study. Effect of migration on the familial aggregation of blood pressure. Hypertension. 1980; 2:I43–I54.7. O'Shaughnessy KM, Karet FE. Salt handling and hypertension. J Clin Invest. 2004; 113:1075–1081.8. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001; 344:3–10.9. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010; 362:590–599.10. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hr urinary sodium and potassium excretion. BMJ. 1988; 297:319–328.11. KNHANES. KNHANES statistical information system. accessed on 1 April 2014. Available at https://knhanes.cdc.go.kr/knhanes/index.do.12. Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, Mertz W, Smith JC Jr. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr. 1984; 40:786–793.13. Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-hr urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002; 16:97–103.14. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139:137–147.15. Ogura M, Kimura A, Takane K, Nakao M, Hamaguchi A, Terawaki H, Hosoya T. Estimation of salt intake from spot urine samples in patients with chronic kidney disease. BMC Nephrol. 2012; 13:36.16. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31–41.17. Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, Kastarinen M, Poulter N, Primatesta P, Rodriguez-Artalejo F, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003; 289:2363–2369.18. World Health Organization. Global status report on noncommunicable diseases 2010. accessed on 1 April 2014. Available at http://www.who.int/nmh/publications/ncd_report2010/en/.19. World Health Organization. Prevention of cardiovascular disease 2007. accessed on 1 April 2014. Available at http://www.who.int/cardiovascular_diseases/publications/Prevention_of_Cardiovascular_DisDise/en/.20. Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013; 3:e003733.21. He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014; 4:e004549.22. Hofman A, Hazebroek A, Valkenburg HA. A randomized trial of sodium intake and blood pressure in newborn infants. JAMA. 1983; 250:370–373.23. Geleijnse JM, Hofman A, Witteman JC, Hazebroek AA, Valkenburg HA, Grobbee DE. Long-term effects of neonatal sodium restriction on blood pressure. Hypertension. 1997; 29:913–917.24. Kotchen TA, Cowley AW Jr, Frohlich ED. Salt in health and disease: a delicate balance. N Engl J Med. 2013; 368:1229–1237.25. He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension. 2003; 42:1093–1099.26. Mann SJ, Gerber LM. Estimation of 24-hrr sodium excretion from spot urine samples. J Clin Hypertens (Greenwich). 2010; 12:174–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Estimated Amount of 24-Hour Urine Sodium Excretion Is Positively Correlated with Stomach and Breast Cancer Prevalence in Korea
- Methodological issues in estimating sodium intake in the Korea National Health and Nutrition Examination Survey
- Evaluation of Random Urine Sodium and Potassium Compensated by Creatinine as Possible Alternative Markers for 24 Hours Urinary Sodium and Potassium Excretion
- High Sodium Intake in Women with Metabolic Syndrome
- 24-hour urine sodium excretion among renal donors in India: a cross-sectional study