Korean Circ J.
2014 Jan;44(1):30-36. 10.4070/kcj.2014.44.1.30.
High Sodium Intake in Women with Metabolic Syndrome
- Affiliations
-
- 1Cardiovascular Center, Dongguk University Ilsan Hospital, Goyang, Korea. mooyong_rhee@dumc.or.kr
- 2Division of Cardiology, Department of Internal Medicine, College of Medicine, Dongguk University, Gyeongju, Korea.
- 3Clinical Trial Center, Dongguk University Ilsan Hospital, Goyang, Korea.
- 4Nutrition Safety Policy Division, Food Nutrition and Dietary Safety Bureau, Ministry of Food and Drug Safety, Osong, Korea.
- 5Department of Statistics, Survey Research Center, Dongguk University, Seoul, Korea.
- KMID: 1859239
- DOI: http://doi.org/10.4070/kcj.2014.44.1.30
Abstract
- BACKGROUND AND OBJECTIVES
Metabolic syndrome and high sodium intake are associated with frequent cardiovascular events. Few studies have estimated sodium intake in subjects with metabolic syndrome by 24-hour urine sodium excretion. We evaluated sodium intake in individuals with metabolic syndrome.
SUBJECTS AND METHODS
Participants were recruited by random selection and through advertisement. Twenty four-hour urine collection, ambulatory blood pressure measurements, and blood test were performed. Sodium intake was estimated by 24-hour urine sodium excretion. Participants receiving antihypertensive medications were excluded from analysis.
RESULTS
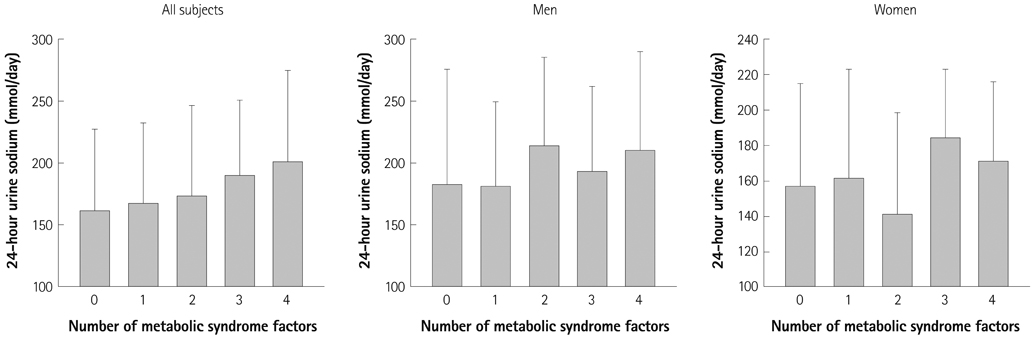
Among the 463 participants recruited, subjects with metabolic syndrome had higher levels of 24-hour urine sodium excretion than subjects without metabolic syndrome (p=0.0001). There was a significant relationship between the number of metabolic syndrome factors and 24-hour urine sodium excretion (p=0.001). The proportion of subjects with metabolic syndrome was increased across the tertile groups of 24-hour urine sodium excretion (p<0.0001). The association of high sodium intake and metabolic syndrome was significant only among women. Among the factors related to metabolic syndrome, body mass index had an independent association with 24-hour urine sodium excretion (p<0.0001).
CONCLUSION
Women with metabolic syndrome exhibited significantly higher sodium intake, suggesting that dietary education to reduce sodium consumption should be emphasized for women with metabolic syndrome.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Inverse association of improved adherence to dietary guidelines with metabolic syndrome: the Seoul Metabolic Syndrome Management program
Dongwoo Ham, YoungYun Cho, Mi-Suk Park, Yun-Sug Park, Sun-Young Kim, Hye-Min Seol, Yoo Mi Park, Sunok Woo, Hyojee Joung, Do-Sun Lim
Nutr Res Pract. 2020;14(6):621-636. doi: 10.4162/nrp.2020.14.6.621.Three clustering patterns among metabolic syndrome risk factors and their associations with dietary factors in Korean adolescents: based on the Korea National Health and Nutrition Examination Survey of 2007-2010
Yeon Yu, YoonJu Song
Nutr Res Pract. 2015;9(2):199-206. doi: 10.4162/nrp.2015.9.2.199.
Reference
-
1. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988; 297:319–328.2. Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007; 334:885–888.3. Tuomilehto J, Jousilahti P, Rastenyte D, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001; 357:848–851.4. MacGregor GA, Markandu ND, Sagnella GA, Singer DR, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet. 1989; 2:1244–1247.5. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001; 344:3–10.6. Jee SH, Jo J. Linkage of epidemiologic evidence with the clinical aspects of metabolic syndrome. Korean Circ J. 2012; 42:371–378.7. Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002; 288:2709–2716.8. Kim D, Choi SY, Choi EK, et al. Distribution of coronary artery calcification in an asymptomatic Korean population: association with risk factors of cardiovascular disease and metabolic syndrome. Korean Circ J. 2008; 38:29–35.9. Chen J, Gu D, Huang J, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009; 373:829–835.10. Kim BK, Lim YH, Kim SG, Kim YM, Shin J. Relationship between sodium intake and blood pressure according to metabolic syndrome status in the Korean National Health and Nutrition Examination Survey. Blood Press Monit. 2012; 17:120–127.11. Stamler J, Elliott P, Chan Q. the INTERMAP Research Group. INTERMAP appendix table, tables of contents (tables A). J Hum Hypertens. 2003; 17:665–758.12. Yoshita K, Miura K, Okayama A, et al. A validation study on food composition tables for the international cooperative INTERMAP study in Japan. Environ Health Prev Med. 2005; 10:150–156.13. Kwon YJ, Kim JY, Kwon KI, et al. Differences between analyzed and estimated sodium contents of food composition table or food exchange list. J Korean Soc Food Sci Nutr. 2010; 39:535–541.14. World Health Organization. Reducing salt intake in populations: report of a WHO forum and technical meeting 5-7 October 2006, Paris, France. Geneva: World Health Organization;2007.15. Rhee MY, Shin SJ, Park SH, Kim SW. Sodium intake of a city population in Korea estimated by 24-h urine collection method. Eur J Clin Nutr. 2013; 67:875–880.16. Knuiman JT, Hautvast JG, van der Heyden L, et al. A multi-centre study on completeness of urine collection in 11 European centres. I. Some problems with the use of creatinine and 4-aminobenzoic acid as markers of the completeness of collection. Hum Nutr Clin Nutr. 1986; 40:229–237.17. Rabi DM, Daskalopoulou SS, Padwal RS, et al. The 2011 Canadian Hypertension Education Program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol. 2011; 27:415–433. e1–e2.18. Lim JH, Kim YK, Kim YS, Na SH, Rhee MY, Lee MM. Relationship between serum uric acid levels, metabolic syndrome, and arterial stiffness in Korean. Korean Circ J. 2010; 40:314–320.19. Lee JS, Park J, Kim J. Dietary factors related to hypertension risk in Korean adults-data from the Korean national health and nutrition examination survey III. Nutr Res Pract. 2011; 5:60–65.20. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001; 37(2 Pt 2):429–432.21. Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2009; 19:123–128.22. Yang Q, Liu T, Kuklina EV, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011; 171:1183–1191.23. Baudrand R, Campino C, Carvajal CA, et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin Endocrinol (Oxf). 2013; [Epub ahead of print].24. Khaw KT, Bingham S, Welch A, et al. Blood pressure and urinary sodium in men and women: the Norfolk Cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). Am J Clin Nutr. 2004; 80:1397–1403.25. He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension. 2008; 51:629–634.26. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006; 49:59–75.27. Sung JK, Kim JY. Obesity and preclinical changes of cardiac geometry and function. Korean Circ J. 2010; 40:55–61.28. Ando K, Fujita T. Pathophysiology of salt sensitivity hypertension. Ann Med. 2012; 44:Suppl 1. S119–S126.29. Shin SJ, Lim CY, Rhee MY, et al. Characteristics of sodium sensitivity in Korean populations. J Korean Med Sci. 2011; 26:1061–1067.30. Liu K, Cooper R, McKeever J, et al. Assessment of the association between habitual salt intake and high blood pressure: methodological problems. Am J Epidemiol. 1979; 110:219–226.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Dietary Sodium-to-Potassium Ratio and Metabolic Syndrome in Korean Adults: Using Data from the Korean National Health and Nutrition Examination Survey 2013-2015
- High fiber and high carbohydrate intake and its association with the metabolic disease using the data of KNHANES 2013 ~ 2017
- Relationship between Kimchi and Metabolic Syndrome in Korean Adults: Data from the Korea National Health and Nutrition Examination Surveys (KNHANES) 2007~2012
- Calcium Status and Bone Mineral Density by the Level of Sodium Intake in Young Women
- Assessment of Nutrient Intake for Middle Aged with and without Metabolic Syndrome Using 2005 and 2007 Korean National Health and Nutrition Survey