Korean Circ J.
2011 Apr;41(4):191-197. 10.4070/kcj.2011.41.4.191.
Non-Dipper Pattern is a Determinant of the Inappropriateness of Left Ventricular Mass in Essential Hypertensive Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. jhs2003@hanyang.ac.kr
- KMID: 2028943
- DOI: http://doi.org/10.4070/kcj.2011.41.4.191
Abstract
- BACKGROUND AND OBJECTIVES
Inappropriately high left ventricular mass (iLVM) is known to be related to cardiovascular prognosis. A non-dipper pattern has a greater mean left ventricular (LV) mass than the dipper pattern in hypertensive patients. However, the appropriateness of LV mass in dipper or non-dipper patterns has not been adequately investigated. The aim of this study was to define the relationship between nocturnal dipping and the appropriateness of LV mass.
SUBJECTS AND METHODS
Using the ambulatory blood pressure monitoring (ABPM) database, the data of 361 patients who underwent ABPM and echocardiography was analyzed retrospectively. Appropriateness of LV mass was calculated as observed/predicted ratio of LV mass (OPR) using a Korean-specified equation. Nocturnal dipping was expressed as percent fall in systolic blood pressure (BP) during the night compared to the day.
RESULTS
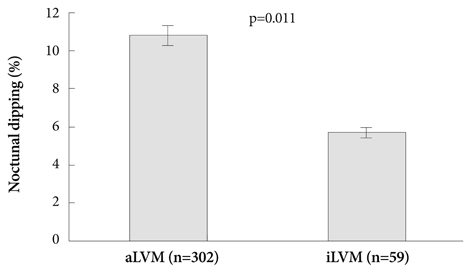
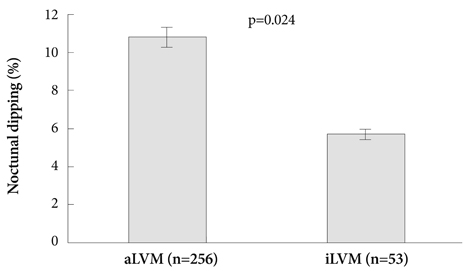
Daytime, nighttime and 24 hours BP in hypertensive patients was 140.4+/-14.8 mmHg, 143.7+/-15.2 mmHg and 129.4+/-20.0 mmHg, respectively. OPR was 106.3+/-19.9% and nocturnal dipping was 10.2+/-10.9 mmHg. In a multiple linear regression model, 24 hours systolic BP (beta=0.097, p=0.043) and nocturnal dipping (beta=-0.098, p=0.046) were independent determinants of OPR as well as age (beta=0.130, p=0.025) and body mass index (BMI) (beta=0.363, p<0.001). Odds ratio of the non-dipper pattern was 2.134 for iLVM (p=0.021) and 3.694 for obesity (p<0.001; BMI >25 kg/m2).
CONCLUSION
The non-dipper pattern is independently associated with iLVM in hypertensive patients as well as obesity.
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of the Relationship between Circadian Blood Pressure Variation and Left Atrial Function Using Strain Imaging
Chan Seok Park, Gun-Hee An, Young-Woon Kim, Youn-Jung Park, Mi-Jeong Kim, Eun Joo Cho, Sang-Hyun Ihm, Hae-Ok Jung, Hee-Yeol Kim, Hui-Kyung Jeon, Ho-Joong Youn, Jae-Hyung Kim
J Cardiovasc Ultrasound. 2011;19(4):183-191. doi: 10.4250/jcu.2011.19.4.183.
Reference
-
1. Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991. 114:345–352.2. Celentano A, Palmieri V, Esposito ND, et al. Inappropriate left ventricular mass in normotensive and hypertensive patients. Am J Cardiol. 2001. 87:361–363.3. de Simone G, Verdecchia P, Pede S, Gorini M, Maggioni AP. Prognosis of inappropriate left ventricular mass in hypertension: the MAVI study. Hypertension. 2002. 40:470–476.4. Ikeda M, Kohno M, Yasunari K, et al. Natriuretic peptide family as a novel antimigration factor of vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 1997. 17:731–736.5. Inoue M, Kanda T, Arai M, et al. Impaired expression of brain natriuretic peptide gene in diabetic rats with myocardial infarction. Exp Clin Endocrinol Diabetes. 1998. 106:484–488.6. Chen HH, Burnett JC. Natriuretic peptides in the pathophysiology of congestive heart failure. Curr Cardiol Rep. 2000. 2:198–205.7. Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. SAMPLE study group. Study on ambulatory monitoring of blood pressure and lisinopril evaluation. Circulation. 1997. 95:1464–1470.8. Ikeda T, Matsuda K, Itoh H, et al. Plasma levels of brain and atrial na-triuretic peptides elevate in proportion to left ventricular end-systolic wall stress in patients with aortic stenosis. Am Heart J. 1997. 133:307–314.9. Devereux RB, Roman MJ, de Simone G, et al. Relations of left ventricular mass to demographic and hemodynamic variables in American Indians: the Strong Heart study. Circulation. 1997. 96:1416–1423.10. Rim SJ. Blood pressure variation and cardiovascular risks. Korean Circ J. 2008. 38:131–134.11. O'Brien E, Asmar R, Beilin L, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens. 2005. 23:697–701.12. Lim YH, Lee JU, Kim KS, et al. Association between inappropriateness of left ventricular mass and left ventricular diastolic dysfunction: a study using the tissue doppler parameter, e/e'. Korean Circ J. 2009. 39:138–144.13. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450–458.14. Shin J, Kim KS, Kim SG, et al. Influences of body size and cardiac workload on the left ventricular mass in healthy Korean adults with normal body weight and blood pressure. Korean Circ J. 2005. 35:335–340.15. Glower DD, Spratt JA, Snow ND, et al. Linearity of the Frank-Starling relationship in the intact heart: the concept of preload recruitable stroke work. Circulation. 1985. 71:994–1009.16. de Simone G, Devereux RB, Kimball TR, et al. Interaction between body size and cardiac workload: influence on left ventricular mass dur-ing body growth and adulthood. Hypertension. 1998. 31:1077–1082.17. de Simone G, Devereux RB, Roman MJ, Alderman MH, Laragh JH. Relation of obesity and gender to left ventricular hypertrophy in normotensive and hypertensive adults. Hypertension. 1994. 23:600–606.18. Palmieri V, de Simone G, Roman MJ, Schwartz JE, Pickering TG, Devereux RB. Ambulatory blood pressure and metabolic abnormalities in hypertensive subjects with inappropriately high left ventricular mass. Hypertension. 1999. 34:1032–1040.19. Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006. 113:898–918.20. Routledge F, McFetridge-Durdle J, Dean C. Night-time blood pres sure patterns and target organ damage: a review. Can J Cardiol. 2007. 23:132–138.21. Parati G, Staessen JA. Day-night blood pressure variations: mechanisms, reproducibility and clinical relevance. J Hypertens. 2007. 25:2377–2380.22. Krauser DG, Devereux RB. Ventricular hypertrophy and hypertension: prognostic elements and implications for management. Herz. 2006. 31:305–316.23. Hermida RC, Ayala DE, Mojon A, Fernandez JR. Effects of time of antihypertensive treatment on ambulatory blood pressure and clinical characteristics of subjects with resistant hypertension. Am J Hypertens. 2010. 23:432–439.24. de la Sierra A, Redon J, Banegas JR, et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009. 53:466–472.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Ventricular Geometric Patterns of Dippers and Non-Dippers in Essential Hypertension
- The Relation of Circadian Blood Pressure Variation to Left Ventricular Mass, Diastolic Function, and Dynamic QT Dispersion
- Patterns of Left Ventricular Remodeling in Essential Hypertension
- 24 hour circadian pattern of blood pressure and its related target organ damage in hypertensive subjects
- Interrlationship between Left Ventricular Mass and Diurnal Variations of Blood Pressure in Patients with Esssntial Hypertension