Korean Circ J.
2011 Apr;41(4):184-190. 10.4070/kcj.2011.41.4.184.
Decreased Glomerular Filtration Rate is an Independent Predictor of In-Hospital Mortality in Patients With ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention
- Affiliations
-
- 1St. Carollo Hospital, Suncheon, Korea.
- 2Chonnam National University, Gwangju, Korea. myungho@chollian.net
- 3Kyungpook National University, Daegu, Korea.
- 4Keimyung University Dongsan Medical Center, Daegu, Korea.
- 5Pusan National University Hospital, Busan, Korea.
- 6Yeungnam University Hospital, Daegu, Korea.
- 7Chungnam National University Hospital, Daejon, Korea.
- 8Seoul National University Bundang Hospital, Seongam, Korea.
- 9Chungbuk National University, Cheongju, Korea.
- 10Kyunghee University Hospital, Seoul, Korea.
- 11Yonsei University Hospital, Seoul, Korea.
- 12Wonju University Hospital, Wonju, Korea.
- 13Catholic University Hospital, Seoul, Korea.
- 14Asan Medical Center, Seoul, Korea.
- KMID: 2028942
- DOI: http://doi.org/10.4070/kcj.2011.41.4.184
Abstract
- BACKGROUND AND OBJECTIVES
Patients with renal dysfunction (RD) experience worse prognosis after myocardial infarction (MI). The aim of the present study was to investigate the impact of admission estimated glomerular filtration rate (eGFR) on clinical outcomes of patients undergoing primary percutaneous coronary intervention (PCI) for ST-segment elevation MI (STEMI).
SUBJECTS AND METHODS
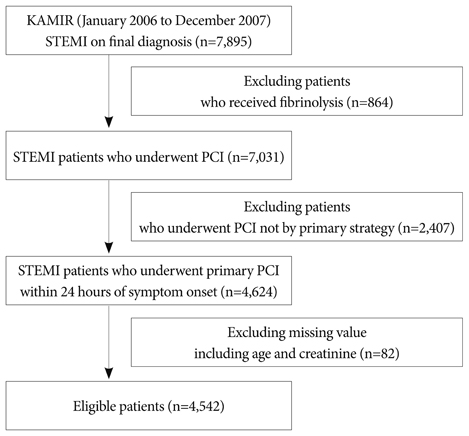
We retrospectively evaluated 4,542 eligible patients from the Korea Acute Myocardial Infarction Registry (KAMIR). Patients were divided into three groups according to eGFR (mL/min/1.73 m2): normal renal function (RF) group (eGFR > or =60, n=3,515), moderate RD group (eGFR between 30 to 59, n=894) and severe RD group (eGFR <30, n=133). Baseline characteristics, angiographic and procedural results, and in-hospital outcomes between the three groups were compared.
RESULTS
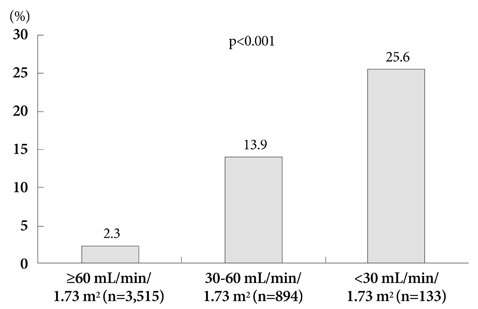
Age, gender, Killip class > or =3, hypertension, diabetes, congestive heart failure, peak creatine kinase-MB, high sensitivity C-reactive protein, B-type natriuretic peptide, left ventricle ejection fraction, multivessel disease, infarct-related artery and rate of successful PCI were significantly different between the 3 groups (p<0.05). With decline in RF, in-hospital complications developed with an increasing frequency (14.1% vs. 31.8% vs. 45.5%, p<0.0001). In-hospital mortality rate was significantly higher in the moderate and severe RD groups as compared to the normal RF group (2.3% vs. 13.9% vs. 25.6%, p<0.0001). Using multivariate logistic regression analysis, adjusted odds ratio for in-hospital mortality was 2.67 {95% confidence interval (CI) 1.44-4.93, p=0.002} in the moderate RD group, and 4.09 (95% CI 1.48-11.28, p=0.006) in the severe RD group as compared to the normal RF group.
CONCLUSION
Decreased admission eGFR was associated with worse clinical courses and it was an independent predictor of in-hospital mortality in STEMI patients undergoing primary PCI.
Keyword
MeSH Terms
-
Arteries
C-Reactive Protein
Creatine
Glomerular Filtration Rate
Heart Failure
Heart Ventricles
Hospital Mortality
Humans
Hypertension
Korea
Logistic Models
Myocardial Infarction
Natriuretic Peptide, Brain
Odds Ratio
Percutaneous Coronary Intervention
Prognosis
Retrospective Studies
C-Reactive Protein
Creatine
Natriuretic Peptide, Brain
Figure
Reference
-
1. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004. 351:1296–1305.2. Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007. 116:85–97.3. Best PJ, Lennon R, Ting HH, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002. 39:1113–1119.4. Pinkau T, Mann JF, Ndrepepa G, et al. Coronary revascularization in patients with renal insufficiency: restenosis rate and cardiovascular outcomes. Am J Kidney Dis. 2004. 44:627–635.5. Al Suwaidi J, Reddan DN, Williams K, et al. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation. 2002. 106:974–980.6. Mielniczuk LM, Pfeffer MA, Lewis EF, et al. Estimated glomerular filtration rate, inflammation, and cardiovascular events after an acute coronary syndrome. Am Heart J. 2008. 155:725–731.7. Beattie JN, Soman SS, Sandber KR, et al. Determinants of mortality after myocardial infarction in patients with advanced renal dysfunction. Am J Kidney Dis. 2001. 37:1191–1200.8. Wright RS, Reeder GS, Herzog CA, et al. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002. 137:563–570.9. Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McMClellan MB. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med. 2002. 137:555–562.10. Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA. 1997. 278:2093–2098.11. Zijlstra F, Hoorntje JC, de Boer MJ, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1999. 341:1413–1419.12. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003. 361:13–20.13. Yamaguchi J, Kasanuki H, Ishii Y, et al. Prognostic significance of serum creatinine concentration for in-hospital mortality in patients with acute myocardial infarction who underwent successful primary percutaneous coronary intervention (from the Heart Institute of Japan Acute Myocardial Infarction [HIJAMI] Registry). Am J Cardiol. 2004. 93:1526–1528.14. Ferrer-Hita JJ, Dominguez-Rodriguez A, Garcia-Gonzalez MJ, Abreu-Gonzalez P. Renal dysfunction is an independent predictor of in-hospital mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Int J Cardiol. 2007. 118:243–245.15. Marenzi G, Moltrasio M, Assanelli E, et al. Impact of cardiac and renal dysfunction on inhospital morbidity and mortality of patients with acute myocardial infarction undergoing primary angioplasty. Am Heart J. 2007. 153:755–762.16. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002. 39:2 Suppl 1. S1–S266.17. Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function: measured and estimated glomerular filtration rate. N Engl J Med. 2006. 354:2473–2483.18. Sorensen CR, Brendorp B, Rask-Madsen C, Kober L, Kjoller E, Torp-Pedersen C. The prognostic importance of creatinine clearance after acute myocardial infarction. Eur Heart J. 2002. 23:948–952.19. Sadeghi HM, Stone GW, Grines CL, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. 2003. 108:2769–2775.20. Namgung J, Doh JH, Lee SY, Huh WS, Park SW, Lee WR. Effect of N-acetylcysteine in prevention of contrast-induced nephropathy after coronary angiography. Korean Circ J. 2005. 35:696–701.21. Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Kimata T, Uemura K. Association of renal insufficiency with in-hospital mortality in Japanese patients with acute myocardial infarction undergoing percutaneous coronary interventions. Int Heart J. 2006. 47:745–752.22. Gibson CM, Pinto DS, Murphy SA, et al. Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol. 2003. 42:1535–1543.23. Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004. 351:1285–1295.24. Lee KH, Jeong MH, Ahn YK, et al. Sex differences of the clinical characteristics and early management in the Korea acute myocardial infarction registry. Korean Circ J. 2007. 37:64–71.25. Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008. 168:987–995.26. Medi C, Montalescot G, Budaj A, et al. Reperfusion in patients with renal dysfunction after presentation with ST-segment elevation or left bundle branch block: GRACE (Global Registry of Acute Coronary Events). JACC Cardiovasc Interv. 2009. 2:26–33.27. McCullough PA, Sandberg KR, Borzak S, Hudson MP, Garg M, Manley HJ. Benefits of aspirin and beta-blockade after myocardial infarction in patients with chronic kidney disease. Am Heart J. 2002. 144:226–232.28. Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003. 42:201–208.29. Lee KH, Lee SR, Kang KP, et al. Periprocedural hemoglobin drop and contrast-induced nephropathy in percutaneous coronary intervention patients. Korean Circ J. 2010. 40:68–73.30. Manoukian SV, Feit F, Mehran R, et al. Impact of major bleeding on 30-day mortality and clinical outcomes in patients with acute coronary syndromes: an analysis from the ACUITY Trial. J Am Coll Cardiol. 2007. 49:1362–1368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Differential Clinical Implications of High-Degree Atrioventricular Block Complicating ST-Segment Elevation Myocardial Infarction according to the Location of Infarction in the Era of Primary Percutaneous Coronary Intervention
- The Impact of Moderate to Severe Renal Insufficiency on Patients With Acute Myocardial Infarction
- Missing Right Coronary Artery in a Patient with Acute Inferior ST Segment Elevation Myocardial Infarction: A Case of Extremely Rare Variation of Coronary Anatomy
- The Operator Volume of Primary Percutaneous Coronary Intervention for ST Segment Elevation Myocardial Infarction Does Not Guarantee Its Quality in Korea