J Lipid Atheroscler.
2015 Dec;4(2):131-135. 10.12997/jla.2015.4.2.131.
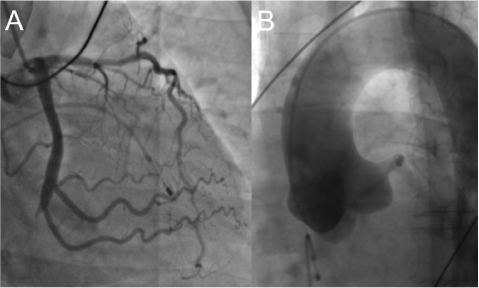
Missing Right Coronary Artery in a Patient with Acute Inferior ST Segment Elevation Myocardial Infarction: A Case of Extremely Rare Variation of Coronary Anatomy
- Affiliations
-
- 1Department of Internal Medicine, Myongji Hospital, Goyang, Korea.
- 2Division of Cardiology, Cardiovascular Center, Myongji hospital, Goyang, Korea. chodk1234@daum.net
- KMID: 2151821
- DOI: http://doi.org/10.12997/jla.2015.4.2.131
Abstract
- We recently encountered an interesting case of acute inferior ST segment elevation myocardial infarction (STEMI). This patient had a rare anatomic variation, single coronary artery. The right coronary artery originate from the left circumflex proper artery, not from aorta, was totally obstructed with thrombi. Though it took more time to figure out the patient's coronary anatomy and the culprit lesion, we successfully performed primary percutaneous coronary intervention within the guideline-recommended time period. We performed left coronary angiography at the beginning. This strategy could be helpful in determining the culprit lesion and preventing unnecessary procedural delay in acute inferior STEMI.
MeSH Terms
Figure
Reference
-
1. Sharbaugh AH, White RS. Single coronary artery. Analysis of the anatomic variation, clinical importance, and report of five cases. JAMA. 1974; 230:243–246.
Article2. Lipton MJ, Barry WH, Obrez I, Silverman JF, Wexler L. Isolated single coronary artery: diagnosis, angiographic classification, and clinical significance. Radiology. 1979; 130:39–47.
Article3. Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992; 20:640–647.
Article4. Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation. 2002; 105:2449–2454.5. Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990; 21:28–40.
Article6. Chung SK, Lee SJ, Park SH, Lee SW, Shin WY, Jin DK. An extremely rare variety of anomalous coronary artery: right coronary artery originating from the distal left circumflex artery. Korean Circ J. 2010; 40:465–467.
Article7. Kim D, Jeong MH, Lee KH, Lee MG, Park KH, Sim DS, et al. Successful primary percutaneous coronary intervention in a patient with acute myocardial infarction and single coronary artery ostium. Korean Circ J. 2012; 42:284–287.
Article8. Choi KL, Kwon JI, Jung WH, Kim EA, Choi SJ, Jin DK, et al. Stenting of an anormalous coronary artery in acute myocardial infarction. Korean Circ J. 1998; 28:1378–1381.9. Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr, Messenger JC, et al. Relation between door-toballoon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015; 385:1114–1122.
Article10. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.
Article11. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. Society for Cardiovascular Angiography and Interventions. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013; 82:E1–E27.12. Chia BL, Yip JW, Tan HC, Lim YT. Usefulness of ST elevation II/III ratio and ST deviation in lead I for identifying the culprit artery in inferior wall acute myocardial infarction. Am J Cardiol. 2000; 86:341–343.
Article13. Verouden NJ, Barwari K, Koch KT, Henriques JP, Baan J, van der Schaaf RJ, et al. Distinguishing the right coronary artery from the left circumflex coronary artery as the infarct-related artery in patients undergoing primary percutaneous coronary intervention for acute inferior myocardial infarction. Europace. 2009; 11:1517–1521.
Article14. Taglieri N, Saia F, Alessi L, Cinti L, Reggiani ML, Lorenzini M, et al. Diagnostic performance of standard electrocardiogram for prediction of infarct related artery and site of coronary occlusion in unselected STEMI patients undergoing primary percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care. 2014; 3:326–339.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography
- Precordial ST-Segment Elevation in Acute Right Ventricular Myocardial Infarction
- A Case of Acute ST-Segment Elevation Myocardial Infarction Mimicking Stress Induced Cardiomyopathy; Demonstration of Typical Echocardiographic Finding Correlated with Unusual Distribution of Left Anterior Descending Coronary Artery
- A Rare Coronary Anomaly: Atypical Double Right Coronary Artery With an Acute Inferior Myocardial Infarction
- A Case of Coronary Artery Dissection after Blunt Chest Trauma Resulting in ST-Segment Elevation Myocardial Infarction