Korean Circ J.
2012 May;42(5):329-334. 10.4070/kcj.2012.42.5.329.
The Number of Endothelial Progenitor Cells is Decreased in Patients With Non-Dipper Hypertension
- Affiliations
-
- 1Department of Cardiovascular Center, Regional Cardiocerebrovascular Disease Center, Wonkwang University Hospital, Iksan, Korea. cardionh@wonkwang.ac.kr
- 2Institute of Wonkwang Medical Science, Iksan, Korea.
- KMID: 2028761
- DOI: http://doi.org/10.4070/kcj.2012.42.5.329
Abstract
- BACKGROUND AND OBJECTIVES
Circulating endothelial progenitor cells (EPCs) play a key role in the maintenance of endothelial homeostasis and promote vascular repair. A reduced number of EPCs and the functional activity have been associated with several cardiovascular risk factors. However, the relationship between the number of EPCs and circadian rhythm of the blood pressure (BP) remains unclear. The purpose of the present study was to evaluate the relationship between the circadian rhythm of the BP and EPCs in patients with essential hypertension.
SUBJECTS AND METHODS
A total of 45 patients with essential hypertension who were newly identified by outpatient BP measurements, underwent 24-hour ambulatory BP monitoring. Among the 45 patients with essential hypertension, 20 were classified as dippers (12 men and 8 women; mean age 48+/-14 years) and 25 as non-dippers (14 men and 11 women; mean age 52+/-18 years). The EPC count was isolated from the peripheral bloodstream and quantified by flow cytometry.
RESULTS
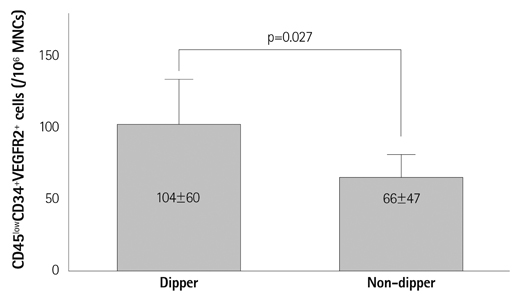
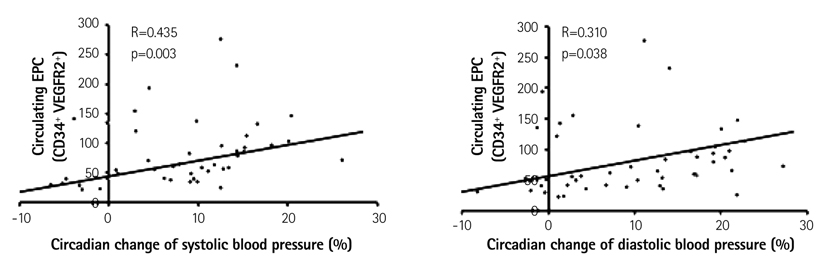
The baseline clinical characteristics were similar between the dipper and non-dipper hypertensive patients. The circulating EPCs were statistically reduced in the non-dipper patients as compared to the dippers (104+/-60 vs. 66+/-47 EPCs per 106 mononuclear cells, p=0.027). The circulating EPC level correlated positively with the circadian changes in the systolic and diastolic BP (r=0.435, p=0.003, and r=0.310, p=0.038, respectively).
CONCLUSION
The present study demonstrated that the EPC count was reduced in the peripheral bloodstream in non-dipper hypertensive patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Juonala M, Viikari JS, Rönnemaa T, Helenius H, Taittonen L, Raitakari OT. Elevated blood pressure in adolescent boys predicts endothelial dysfunction: the Cardiovascular Risk in Young Finns Study. Hypertension. 2006. 48:424–430.2. Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994. 24:793–801.3. Gehling UM, Ergün S, Schumacher U, et al. In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood. 2000. 95:3106–3112.4. Vasa M, Fichtlscherer S, Aicher A, et al. Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res. 2001. 89:E1–E7.5. Werner N, Kosiol S, Schiegl T, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005. 353:999–1007.6. Hill JM, Zalos G, Halcox JP, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003. 348:593–600.7. Kohara K, Nishida W, Maguchi M, Hiwada K. Autonomic nervous function in non-dipper essential hypertensive subjects: evaluation by power spectral analysis of heart rate variability. Hypertension. 1995. 26:808–814.8. Choi JH, Oh SK, Yun KH, et al. Effect of early statin therapy on circulating endothelial progenitor cells during the acute phase in patients with acute myocardial infarction. Korean Circ J. 2008. 38:411–418.9. Asahara T, Murohara T, Sullivan A, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997. 275:964–967.10. Kong D, Melo LG, Gnecchi M, et al. Cytokine-induced mobilization of circulating endothelial progenitor cells enhances repair of injured arteries. Circulation. 2004. 110:2039–2046.11. Urbich C, Dimmeler S. Endothelial progenitor cells: characterization and role in vascular biology. Circ Res. 2004. 95:343–353.12. Hristov M, Weber C. Endothelial progenitor cells: characterization, pathophysiology, and possible clinical relevance. J Cell Mol Med. 2004. 8:498–508.13. Chironi G, Walch L, Pernollet MG, et al. Decreased number of circulating CD34+KDR+ cells in asymptomatic subjects with preclinical atherosclerosis. Atherosclerosis. 2007. 191:115–120.14. Schmidt-Lucke C, Rössig L, Fichtlscherer S, et al. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005. 111:2981–2987.15. Imanishi T, Moriwaki C, Hano T, Nishio I. Endothelial progenitor cell senescence is accelerated in both experimental hypertensive rats and patients with essential hypertension. J Hypertens. 2005. 23:1831–1837.16. Oliveras A, Soler MJ, Martínez-Estrada OM, et al. Endothelial progenitor cells are reduced in refractory hypertension. J Hum Hypertens. 2008. 22:183–190.17. Bahlmann FH, de Groot K, Mueller O, Hertel B, Haller H, Fliser D. Stimulation of endothelial progenitor cells: a new putative therapeutic effect of angiotensin II receptor antagonists. Hypertension. 2005. 45:526–529.18. Yu Y, Fukuda N, Yao EH, et al. Effects of an ARB on endothelial progenitor cell function and cardiovascular oxidation in hypertension. Am J Hypertens. 2008. 21:72–77.19. Dernbach E, Urbich C, Brandes RP, Hofmann WK, Zeiher AM, Dimmeler S. Antioxidative stress-associated genes in circulating progenitor cells: evidence for enhanced resistance against oxidative stress. Blood. 2004. 104:3591–3597.20. Yun KH, Shin IS, Park EM, et al. Effect of additional statin therapy on endothelial function and prognosis in patients with vasospastic angina. Korean Circ J. 2008. 38:638–643.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Differentiation of Pluripotent Stem Cells towards Endothelial Progenitor Cells – Potential Application in Pulmonary Arterial Hypertension
- Endothelial Progenitor Cells' Classification and Application in Neurological Diseases
- Prevalence of early renal damage between dippers and non-dippers in mild to moderate Korean hypertensives
- Endothelial progenitor cells and mesenchymal stem cells from human cord blood
- Regular Exercise Training Increases the Number of Endothelial Progenitor Cells and Decreases Homocysteine Levels in Healthy Peripheral Blood