J Korean Diabetes Assoc.
2007 Jan;31(1):44-50. 10.4093/jkda.2007.31.1.44.
Activin A and Glucose Derived Human Pancreatic Ductal Cells into Insulin-producing Cells
- Affiliations
-
- 1Samsung Biomedical Research Institute (SBRI), Korea.
- 2Department of Life Science, College of Natural Sciences, Chungang University, Korea.
- 3Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- KMID: 2008095
- DOI: http://doi.org/10.4093/jkda.2007.31.1.44
Abstract
-
BACKGROUND: Cellular replacement therapy holds promise for the treatment of diabetes mellitus but donor tissue is severely limited. Human postnatal pancreatic ductal cells are a potential source of new beta cells. Therefore, we investigated the potential of human pancreatic ductal cells could be differentiated into endocrine cells that would be capable of secreting insulin in response to glucose.
METHODS
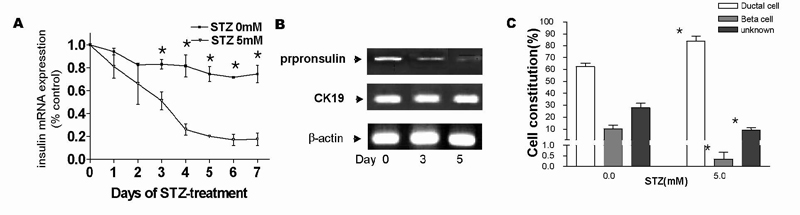
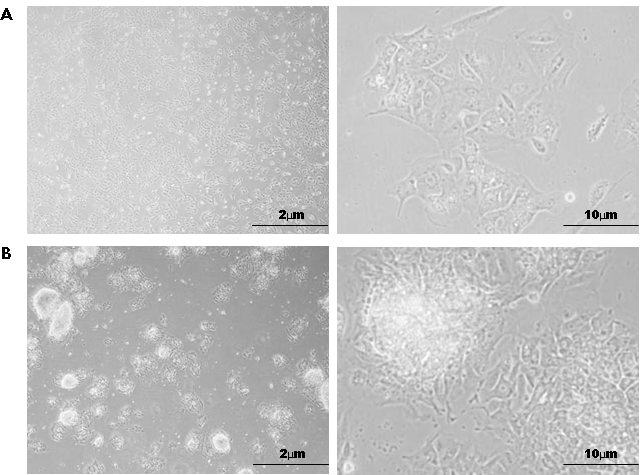
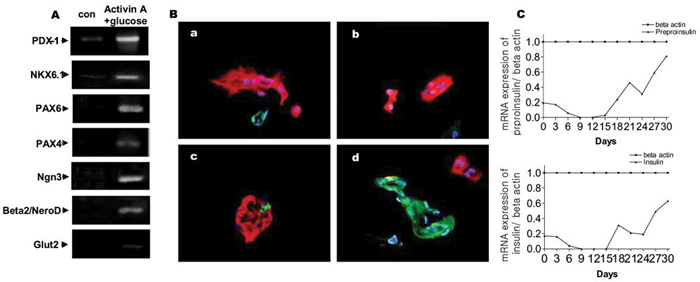
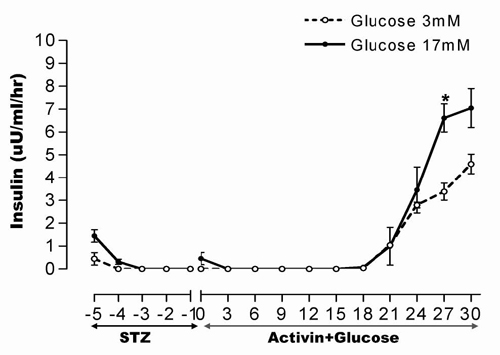
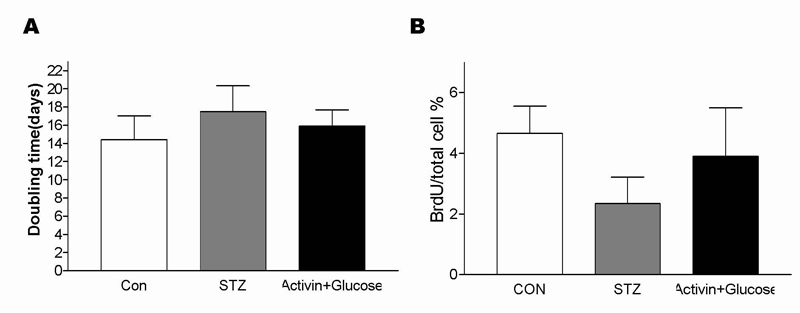
Cell fractions enriched with pancreatic ductal cells after human islet isolation were treated with streptozotocin to remove residual beta cells, grown in monolayer culture, changed the media for differentiation in the presence of activin A and glucose, supplemented with 10% FCS. The differentiation markers, insulin secretion and cell proliferation were examined. RESULT: No insulin was detectable in cell preparations after 5 days of treatment with streptozotocin. In monolayer culture, 80% of the streptozotocin-treated pancreatic ductal cells expressed cytokeratin-19. Cell cultures with a high proportion of cytokeratin-19 cells had greater plasticity for differentiation into cells with phenotypic and functional markers of beta cells. This property were significantly enhanced by treatment of activin A and glucose. The differentiated human pancreatic ductal cells secreted insulin sensitively responded with high glucose.
CONCLUSION
Human pancreatic ductal cells are a potential source of new glucose -induced insulin producing cells that may be developed further for clinical use. Therefore, the present data support a possible role for human adult pancreatic ductal cells, following expansion and differentiation, as a source of insulin by transplantation cells to type I diabetes patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Arias AE, Bendayan M. Differentiation of pancreatic acinar cells into duct-like cells in vitro. Lab Invest. 1993. 69:518–530.2. De Lisle RC, Logsdon CD. Pancreatic acinar cells in culture: expression of acinar and ductal antigens in a growthrelated manner. Eur J Cell Biol. 1990. 51:64–75.3. Hall PA, Lemoine NR. Rapid acinar to ductal transdifferentiation in cultured human exocrine pancreas. J Pathol. 1992. 166:97–103.4. Soria B, Skoudy A, Martin F. From stem cells to beta cells: New strategies in cell therapy of diabetes mellitus. Diabetologia. 2001. 44:407–415.5. Zhao M, Amiel SA, Christie MR, Rela M, Heaton N, Huang GC. Insulin-producing cells derived from human pancreatic non-endocrine cell cultures reverse streptozotocin-induced hyperglycaemia in mice. Diabetologia. 2005. 48:2051–2061.6. Klein T, Frandsen U, Heller RS, Serup P. IMPAN Cells: A pancreatic model for differentiation into endocrine cells. Arch Biochem Biophys. 2001. 395:259–263.7. Bonner-Weir S, Taneja M, Weir GC. In vitro cultivation of human islets from expanded ductal tissue. Proc Natl Acad Sci USA. 2000. 97:7999–8004.8. Ramiya VK, Maraist M, Arfors KE, scharz DA, Peck AB, Cornelius JG. Reversal of insulin dependent diabetes using islets generated in vitro from pancreatic stem cells. Nat Med. 2000. 6:278–282.9. Soria B, Roche E, Berna G, Quinto TL, Reig JA, Martin F. Insulin secreting cells derived from embryonic stem cells normalize glycemia in streptozotocin-induced diabetic mice. Diabetes. 2000. 49:157–162.10. Assady S, Maor G, Amit M, Eldor JI, Skorecki KL, Tzukerman M. Insulin production by human embryonic stem cells. Diabetes. 2001. 50:1691–1697.11. Lumelsky N, Blondel O, Laeng P, Velasco I, Ravin R, Mckay R. Differentiation of embryonic stem cells to insulin-secreting structures similar to pancreatic islets. Science. 2001. 292:1389–1394.12. Terada N, Hamazaki T, Oka M, Hoki M, Mastalerz DM, Nakano Y, Meyer EM, Morel L, Petersen BE, Scott EW. Bone marrow cells adopt the phenotype of other cells by spontaneous cell fusion. Nature. 2002. 416:542–545.13. Ogata T, Park KY, Seno M, Kojima I. Reversal of streptozotocin-induced hyperglycemia by transplantation of pseudoislets consisting of beta cells derived from ductal cells. Endocr J. 2004. 51:381–386.14. Hemmati-Brivanlou A, Melton DA. Inhibition of activin receptor signaling promotes neuralization in Xenopus. Cell. 1994. 77:273–281.15. Moriya N, Komazaki S, Takahashi S, Yokota C, Asashima M. In vitro pancreas formation from Xenopus ectoderm treated with activin and retinoic acid. Dev Growth Differ. 2000. 42:593–602.16. Yamaoka T, Idehara C, Yano M, Matsushita T, Yamada T, Li S, Moritani M, Hata J, Sugino H, Noji S, Itakura M. Hypoplasia of pancreatic islets in transgenic mice expressing activin receptor mutants. J Clin Invest. 1998. 102:294–301.17. Rabinovitch A, Blondel B, Murray T, Mintz DH. Cyclic adenosine-3, 5-monophosphate stimulates islet B cell replication in neonatal rat pancreatic monolayer cultures. J Clin Invest. 1980. 66:1065–1071.18. Elsner M, Tiedge M, Lenzen S. Mechanism underlying resistance of human pancreatic beta cells against toxicity of streptozotocin and alloxan. Diabetologia. 2003. 46:1713–1714.19. Kaltsas GA, Mukherjee JJ, Isidori A. Treatment of advanced neuroendocrine tumours using combination chemotherapy with lomustine and 5-fluorouracil. Clin Endocrinol (Oxf). 2002. 57:169–183.20. Delaunoit T, Ducreux M, Boige V. The doxorubicin-streptozotocin combination for the treatment of advanced well-differentiated pancreatic endocrine carcinoma; a judicious option? Eur J Cancer. 2004. 40:515–520.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Activin A Converts Pancreatic Ductal Cells into Insulin-Secreting Cells
- Cell Replacement and Regeneration Therapy for Diabetes
- Umbilical Cord Derived Mesenchymal Stem Cells Useful in Insulin Production - Another Opportunity in Cell Therapy
- Pancreatic Diseases: Genetics and Modeling Using Human Pluripotent Stem Cells
- Pancreatic Exocrine and Endocrine Cell Differentiation during Pancreatic Regeneration