J Korean Acad Conserv Dent.
2011 Jan;36(1):26-36. 10.5395/JKACD.2011.36.1.26.
The effect of tumor necrosis factor (TNF)-alpha to induce matrix metalloproteinase (MMPs) from the human dental pulp, gingival, and periodontal ligament cells
- Affiliations
-
- 1Department of Conservative Dentistry, St. Paul's Hospital, The Catholic University School of Medicine, Seoul, Korea.
- 2Oral Biology Institutue, Kyung Hee University, Seoul, Korea. gwchoi@khu.ac.kr
- 3Department of Conservative Dentistry, Kyung Hee University School of Dentistry, Seoul, Korea.
- KMID: 1446081
- DOI: http://doi.org/10.5395/JKACD.2011.36.1.26
Abstract
OBJECTIVES
In the present study, three kinds of tissues cells (pulp, gingiva, and periodontal ligament) were investigated if those cells express MMP and TIMP when they were stimulated with neuropeptides (substance P, CGRP) or proinflammatory cytokine, TNF-alpha.
MATERIALS AND METHODS
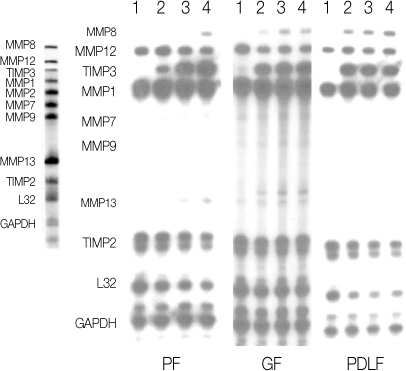
The cells cultured from human dental pulp (PF), gingiva (GF) and periodontal ligament were (PDLF) stimulated with Mock, SP, TNF-alpha, and CGRP for 24 hrs and 48 hrs. for an RNase protection assay and Enzyme Linked Immunosorbent Assay. Cells (PF, GF and PDLF) seeded in 100 mm culture dish were stimulated with SP (10(-5), 10(-8) M) or only with medium (Mock stimulation) for 4hrs and for 24 hrs for RNase Protection Assay, and they were stimulated with CGRP (10(-5) M) and TNF-alpha (2 ng/mL) for 24 hrs and with various concentraion of TNF-alpha (2, 10, and 100 ng/mL) for Rnase Protection Assay with a human MMP-1 probe set including MMP 1, 2, 8, 7, 8, 9, 12, and TIMP 2, 3. In addition, cells (PF, GF and PDLF) were stimulated with Mock and various concentraion of TNF-alpha(2, 10, and 100 ng/mL) for 24 hrs and with TNF-alpha(10 ng/mL) for 48 hrs, and the supernatents from the cells were collected for Enzyme Linked Immunosorbent Assay (ELISA) for MMP-1 and MMP-13.
RESULTS
The expression of MMPs in PF, GF, PDLF after stimulation with SP and CGRP were not changed compared with Mock stimulation for 4 hrs and 24 hrs. The expression of MMP-1, -12, -13 24 hrs after stimulation with TNF-alpha were upregulated, however the expression of TIMP-3 in PF, GF, PDLF after stimulation with TNF-alpha were downregulated. TNF-alpha (2 ng/mL, 10 ng/mL, 100 ng/mL) increased MMP-1 and MMP-12 expression in PF dose dependently for 24 hrs.
CONCLUSIONS
TNF-alpha in the area of inflammation may play an important role in regulating the remodeling of dentin, cementum, and alveolar bone.
Keyword
MeSH Terms
-
Dental Cementum
Dental Pulp
Dentin
Enzyme-Linked Immunosorbent Assay
Gingiva
Humans
Inflammation
Matrix Metalloproteinases
Neuropeptides
Periodontal Ligament
Ribonucleases
Seeds
Substance P
Tissue Inhibitor of Metalloproteinase-3
Tumor Necrosis Factor-alpha
Matrix Metalloproteinases
Neuropeptides
Ribonucleases
Substance P
Tissue Inhibitor of Metalloproteinase-3
Tumor Necrosis Factor-alpha
Figure
Reference
-
1. Park SH, Hsiao GY, Huang GT. Role of substance P and calcitonin gene-related peptide in the regulation of interleukin-8 and monocyte chemotactic protein-1 expression in human dental pulp. Int Endod J. 2004. 37:185–192.
Article2. Patel T, Park SH, Lin LM, Chiappelli F, Huang GT. Substance P induces interleukin-8 sectretion from human dental pulp cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 96:478–485.
Article3. Palosaari H, Wahlgren J, Larmas M, Rönkã H, Sorsa T, Salo T, Tjãderhane L. The Expression of MMPs-8 in human odontoblasts and dental pulp cells is down-regulated by TGF-β1. J Dent Res. 2000. 79:77–84.
Article4. Wisithphrom K, Windsor LJ. The effects of Tumor Necrosis Factor-α, Interleukin-1β, Interleukin-6, and Transforming Growth Factor-β1 on Pulp Fibroblast Mediated Collagen Degradation. J Endod. 2006. 32:853–861.
Article5. Krane SM. Clinical importance of metalloproteinases and their inhibitors. Ann N Y Acad Sci. 1994. 732:1–10.
Article6. Birkedal-Hansen H, Moore WG, Bodden MK, Windser LJ, Birkedal-Hansen B, Decarlo A, Engler JA. Matrix metalloproteinases; a review. Crit Rev Oral Biol Med. 1993. 4:197–250.
Article7. Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol. 2001. 17:463–516.
Article8. Douglas DA, Shi YE, Sang QA. Computational sequence analysis of the tissue inhibitor metalloproteinases family. J Protein Chem. 1997. 16:237–255.9. Dean DD, Martel-Pelletier J, Pelletier JP, Howell OS, Woessner JF Jr. Evidence for metalloproteinases and metalloproteinases inhibitor imbalance in human osteoarthritic cartilage. J Clin Invest. 1989. 84:678–685.
Article10. Stamenkovic I. Matrix metalloproteinases in tumor invasion and metastasis. Semin Cancer Biol. 2000. 10:415–433.
Article11. Tjãderhane L, Palosaari H, Sulkala M, Wahlgren J, Salo T. The Expression of Matrix metalloproteinase (MMPs) in Human odontoblasts. Dentin/Pulp complex. 2000. I45–I51.12. Tani-Ishii N, Wang CY, Stashenko P. Immonolocalization of bone resorptive cytokines in rat pulp and periodontal lesions following surgical pulp exposure. Oral Microbiol Immunol. 1995. 10:213–219.
Article13. Mauviel A, Halcin C, Vasiloudes P, Parks WC, Kurkinen M, Uitto J. Uncoordinate regulation of collagenase, stromelysin, and tissue inhibitor of metalloproteinases genes by prostaglandin E2: selective enhancement of collagenase gene expression in human dermal fibroblasts in culture. J cell Biochem. 1994. 54:465–472.
Article14. Daphna-Iken D, Morrison AR. Interleukin-1β induces interstitial collagenase gene expression and protein secretion in renal mesangial cells. Am J Physiol. 1995. 269:F831–F837.15. Wakisaka S. Neuropeptides in the dental pulp: distribution, origins, and correlation. J Endod. 1990. 16:67–69.
Article16. Fristad I, Kvinnsland IH, Jonsson R, Heyeraas RJ. Effect of intermittent long lasting electrical tooth stimulation and pulpal blood flow and immunocompetent cell: a hemodynamic and immunohistochemical study in young rat molars. Exp Neurol. 1997. 146:230–239.
Article17. Killough SA, Lundy FT, Irwin CR. Substance P expression by human dental pulp fibroblasts: a potential role in neurogenic inflammation. J Endod. 2009. 35:73–77.
Article18. Wang FM, Hu T, Cheng R, Tan H, Zhou XD. Substance P influenced gelatinolytic activity via reactive oxygen species in human pulp cells. Int Endod J. 2008. 41:856–862.
Article19. Coil J, Tam E, Waterfield D. Proinflammatory cytokine profile in pulp fibroblasts stimulated with Lipopolysaccharide and Methyl Mercaptan. J Endod. 2004. 30:88–91.
Article20. Palosaari H, Pennington CJ, Larmas M, Edwards DR, Tjãderhane L, Salo T. Expression profile of matrix metalloproteinase (MMPs) and tissue inhibitor of MMPs in human odontoblasts and pulp tissue. Eur J Oral Sci. 2003. 111:117–127.
Article21. Takiguchi T, Kobayashi M, Suzuki R, Yamaguchi R, Isatsu K, Nishihara T, Nagumo M, Hasegawa K. Recombinant human bone morphogenetic protein-2 stimulates osteoblast differentiation and suppresses matrix metalloproteinases-1 production in human bone cells isolated from mandibule. J Periodontal Res. 1998. 33:476–485.
Article22. Johansson N, Saarialho-Kere U, Airola K, Herva R, Nissinen L, Westermarck J, Vuorio E, Heino J, Kãhãri VM. Collagenase-3 (MMP-3) is expressed by hypertrophic chodrocytes, periosteal cells, and osteoblasts during human fetal bone development. Dev Dyn. 1997. 208:387–397.
Article23. Lin SK, Wang CC, Huang S, Lee JJ, Chiang CP, Lan WH, Hong CY. Induction of dental pulp fibroblast matrix metalloproteinase-1 and tissue inhibitor of metalloproteinase-1 gene expression by interleukin-1α and tumor necrosis factor-α through a prostaglandin-dependent pathway. J Endod. 2001. 27:185–188.
Article24. O'Boskey FJ, Panagakos FS. Cytokines stimulate matrix metalloproteinase production by human pulp cells during long-term culture. J Endod. 1998. 24:7–10.25. Ueda I, Matsushima K. Stimulation of plasminogen activator activity and matrix metalloproteinase of human dental pulp derived cells by tumor necrosis factor-α. J Endod. 2001. 27:175–179.
Article26. Wahlgren J, Salo T, Teronen O, Sorsa T, Tjaderhane L. Matrix metalloproteinase-8 (MMP-8) in pulpal and periapical inflammation and periapical root-canal exudates. Int Endod J. 2002. 35:897–904.
Article27. Bond M, Murry G, Bennett MR, Amour A, Knauper V, Newby AC, Baker AH. Localization of the death domain of tissue inhibitor of metalloproteinases-3 to the N-terminus metalloproteinase inhibition is associated with proapoptotic activity. J Biol Chem. 2000. 275:41358–41363.
Article28. Yu WH, Yu CS-S, Meng Q, Brew K, Woessner JF. TIMP-3 binds to sulfated glycosaminoglycans of the extracellular matrix. J Biol Chem. 2000. 275:31226–31232.
Article29. Hummel V, Kallmann BA, Wagner S, Füller T, Bayas A, Tonn JC, Benveniste EN, Toyka KV, Rieckmann P. Production of MMPS in Cerebral Endothelial Cells and Their Role in Shedding Adhesion Molecules. J Neuropathol EXP Neurol. 2001. 60:320–328.
Article30. Sulkala M, Larmas M, Sorsa T, Salo T, Tjãderhane L. 771;derhane L. The localization of matrix metalloproteinase-20 (MMP-20, Enamelysin) in mature human teeth. J Dent Res. 2002. 81:603–607.
Article31. Leeman MF, Curran S, Murray GI. The structure, regulation, and function of human matrix metalloproteinase-13. Crit Rev Biochem Mol Biol. 2002. 37:149–166.
Article32. Sawa Y, Horie Y, Yamaoka Y, Ebata N, Kim T, Yoshida S. Production of colony-stimulating factor in human dental pulp fibroblasts. J Dent Res. 2003. 82:96–100.
Article33. Langton KP, Barker MD, Mckie N. Localization of the functional domains of human tissue inhibitor of metalloproteinases-3 and the effects of a Sorsby's fundus dystrophy mutation. J Biol Chem. 1998. 273:16778–16781.
Article34. Graves DT, Cochran D. The Contribution of interleukin-1 and Tumor Necrosis Factor to Periodontal Tissue Destruction. J Periodontol. 2003. 74:391–401.
Article35. Takashiba S, Naruishi K, Murayama Y. Perspective of cytokine regulation for periodontal treatment: fibroblast biology. J Periodontol. 2003. 74:103–110.
Article36. Thomson BM, Mundy GR, Chambers TJ. Tumor necrosis factor-α and β induce osteoblastic cells to stimulate osteoclastic bone resorption. J Immunol. 1987. 138:775–779.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-inflammatory effects of PPARgamma on human dental pulp cells
- Vitamin D maintains E-cadherin intercellular junctions by downregulating MMP-9 production in human gingival keratinocytes treated by TNF-α
- Expression of mRNA for matrix metalloproteinases and tissue inhibitors of metalloproteinases in human gingival and periodontal ligament fibroblasts treated with lipopolysaccharide from Prevotella intermedia
- The effect of neuropeptides on secretion of Interleukin-8 (IL-8)
- Comparison of the Effects of Matrix Metalloproteinase Inhibitors on TNF-alpha Release from Activated Microglia and TNF-alpha Converting Enzyme Activity