Korean J Radiol.
2009 Oct;10(5):447-454. 10.3348/kjr.2009.10.5.447.
MR Diagnosis of a Pulmonary Embolism: Comparison of P792 and Gd-DOTA for First-Pass Perfusion MRI and Contrast-Enhanced 3D MRA in a Rabbit Model
- Affiliations
-
- 1Department of Biomedical Engineering, Emory University and Georgia Institute of Technology, Atlanta, GA, USA.
- 2Department of Radiology, University of Virginia Health System, Charlottesville, VA, USA. kdh2n@virginia.edu
- 3Department of Radiology, Gulhane Military Medical Academy, Ankara, Turkey.
- 4Guerbet Research, Aulnay-sous-Bois, France.
- 5Department of Radiology, Kagawa University Faculty of Medicine, Kagawa, Japan.
- 6Department of Diagnostic Radiology, Osaka Neurosurgical Hospital, Kagawa, Japan.
- KMID: 1093959
- DOI: http://doi.org/10.3348/kjr.2009.10.5.447
Abstract
OBJECTIVE
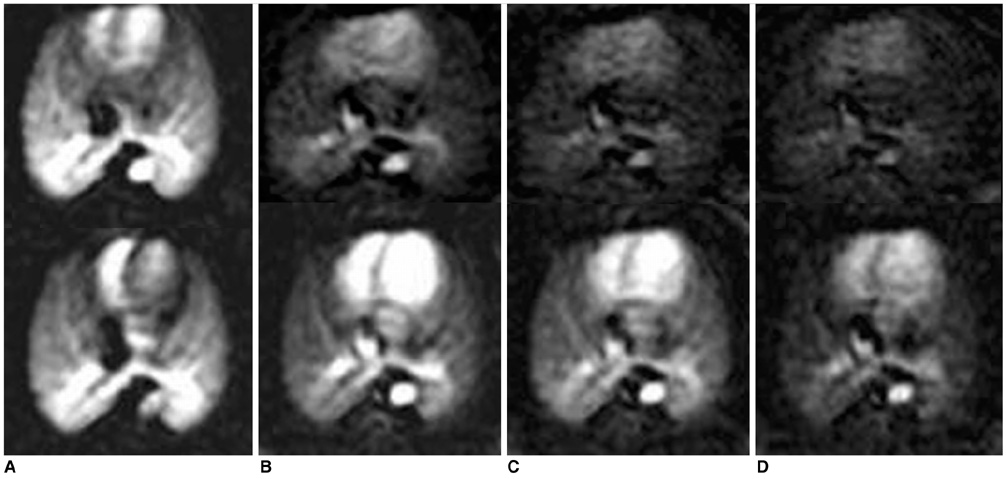
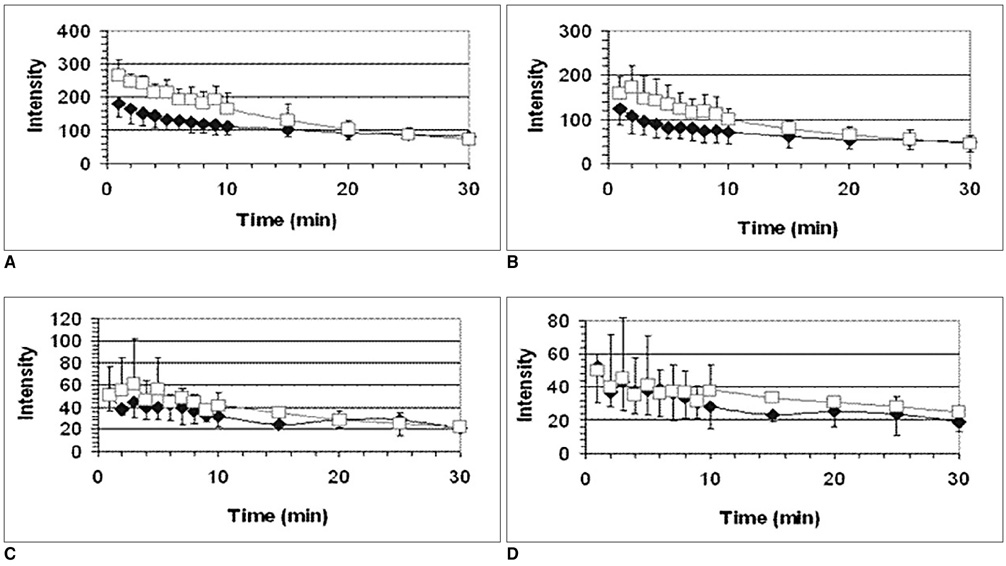
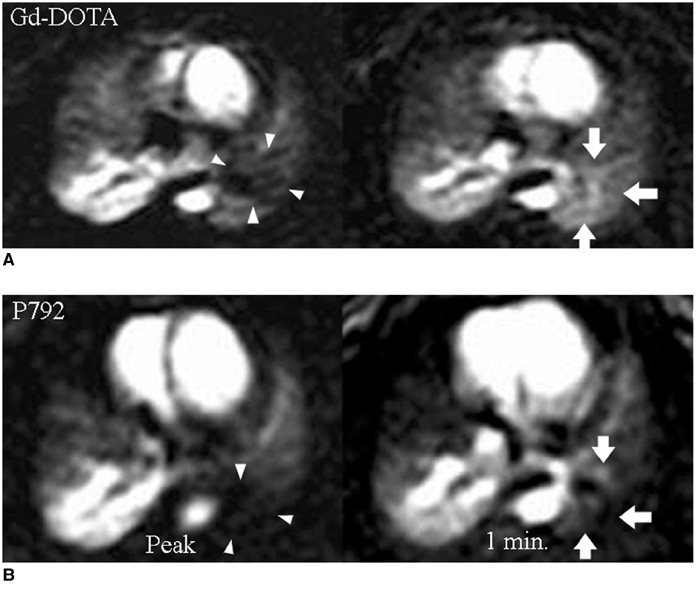
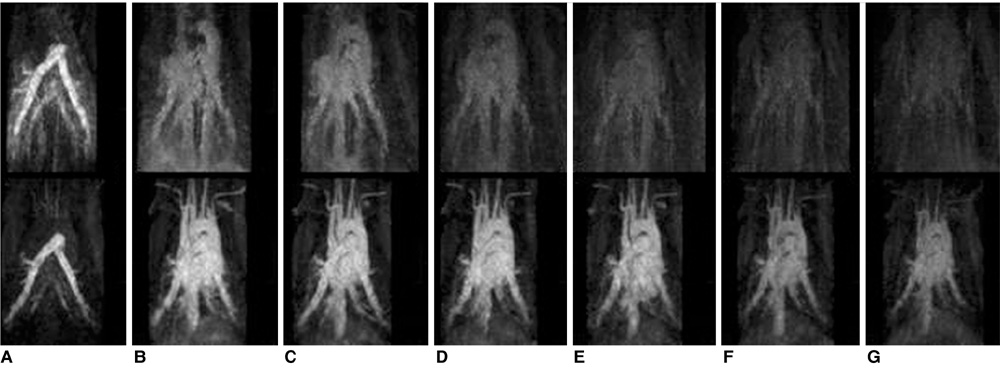
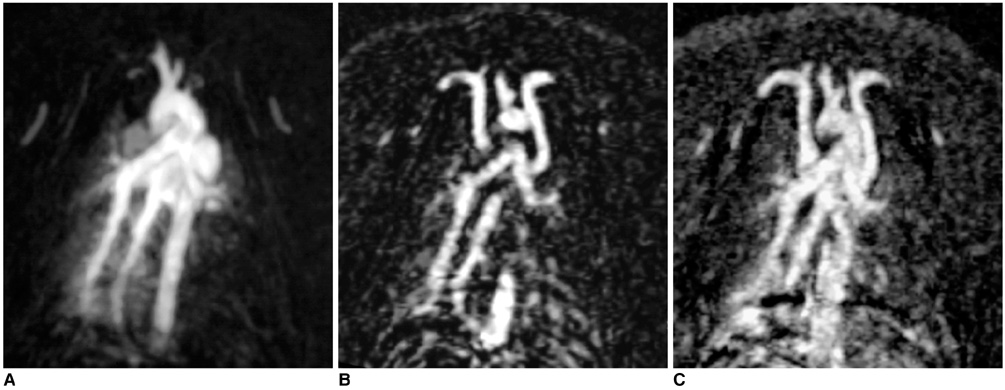
To compare P792 (gadomelitol, a rapid clearance blood pool MR contrast agent) with gadolinium-tetraazacyclododecanetetraacetic acid (Gd-DOTA), a standard extracellular agent, for their suitability to diagnose a pulmonary embolism (PE) during a first-pass perfusion MRI and 3D contrast-enhanced (CE) MR angiography (MRA). MATERIALS AND METHODS: A perfusion MRI or CE-MRA was performed in a rabbit PE model following the intravenous injection of a single dose of contrast agent. The time course of the pulmonary vascular and parenchymal enhancement was assessed by measuring the signal in the aorta, pulmonary artery, and lung parenchyma as a function of time to determine whether there is a significant difference between the techniques. CE-MRA studies were evaluated by their ability to depict the pulmonary vasculature and following defects between 3 seconds and 15 minutes after a triple dose intravenous injection of the contrast agents. RESULTS: The P792 and Gd-DOTA were equivalent in their ability to demonstrate PE as perfusion defects on first pass imaging. The signal from P792 was significantly higher in vasculature than that from Gd-DOTA between the first and the tenth minutes after injection. The results suggest that a CE-MRA PE could be reliably diagnosed up to 15 minutes after injection. CONCLUSION: P792 is superior to Gd-DOTA for the MR diagnosis of PE.
Keyword
MeSH Terms
-
Animals
Contrast Media/administration & dosage
Heterocyclic Compounds/administration & dosage/*diagnostic use
Imaging, Three-Dimensional
Injections, Intravenous
Magnetic Resonance Angiography/*methods
Magnetic Resonance Imaging/*methods
Organometallic Compounds/administration & dosage/*diagnostic use
Pulmonary Embolism/*diagnosis
Rabbits
Figure
Reference
-
1. Carson JL, Kelley MA, Duff A, Weg JG, Fulkerson WJ, Palevsky HI, et al. The clinical course of pulmonary embolism. N Engl J Med. 1992. 326:1240–1245.2. Goldhaber SZ. Pulmonary embolism. N Engl J Med. 1998. 339:93–104.3. Barritt DW, Jordan SC. Anticoagulant drugs in the treatment of pulmonary embolism. A controlled trial. Lancet. 1960. 1:1309–1312.4. The PIOPED Investigators. Value of the ventilation/perfusion scan in acute pulmonary embolism: result of the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED). JAMA. 1990. 263:2753–2759.5. Meaney JF, Weg JG, Chenevert TL, Stafford-Johnson D, Hamilton BH, Prince MR. Diagnosis of pulmonary embolism with magnetic resonance angiography. N Engl J Med. 1997. 336:1422–1427.6. Oudkerk M, van Beek EJ, Wielopolski P, van Ooijen PM, Brouwers-Kyuper EM, Bongaerts AH, et al. Comparison of contrast-enhanced magnetic resonance angiography and conventional pulmonary angiography for the diagnosis of pulmonary embolism: a prospective study. Lancet. 2002. 359:1643–1647.7. Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999. 42:952–962.8. Griswold MA, Jakob PM, Heidemann RM, Nittka M, Jellus V, Wang J, et al. Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med. 2002. 47:1202–1210.9. Ohno Y, Higashino T, Takenaka D, Sugimoto K, Yoshikawa T, Kawai H, et al. MR angiography with sensitivity encoding (SENSE) for suspected pulmonary embolism: comparison with MDCT and ventilation-perfusion scintigraphy. AJR Am J Roentgenol. 2004. 183:91–98.10. Hatabu H, Tadamura E, Levin DL, Chen Q, Li W, Kim D, et al. Quantitative assessment of pulmonary perfusion with dynamic contrast-enhanced MRI. Magn Reson Med. 1999. 42:1033–1038.11. Fink C, Ley S, Puderbach M, Plathow C, Bock M, Kauczor HU. 3D pulmonary perfusion MRI and MR angiography of pulmonary embolism in pigs after a single injection of a blood pool MR contrast agent. Eur Radiol. 2004. 14:1291–1296.12. Port M, Corot C, Rousseaux O, Raynal I, Devoldere L, Idee JM, et al. P792: a rapid clearance blood pool agent for magnetic resonance imaging: preliminary results. MAGMA. 2001. 12:121–127.13. Port M, Corot C, Raynal I, Idee JM, Dencausse A, Lancelot E, et al. Physicochemical and biological evaluation of P792, a rapid clearance blood pool agent for magnetic resonance imaging. Invest Radiol. 2001. 36:445–454.14. Keilholz SD, Mai VM, Berr SS, Fujiwara N, Hagspiel KD. Comparison of first-pass Gd-DOTA and FAIRER MR perfusion imaging in a rabbit model of pulmonary embolism. J Magn Reson Imaging. 2002. 16:168–171.15. Corot C, Violas X, Robert P, Port M. Pharmacokinetics of three gadolinium chelates with different molecular sizes shortly after intravenous injection in rabbits: relevance to MR angiography. Invest Radiol. 2000. 35:213–218.16. Corot C, Violas X, Robert P, Gagneur G, Port M. Comparison of different types of blood pool agents (P792, MS325, USPIO) in a rabbit MR angiography-like protocol. Invest Radiol. 2003. 38:311–319.17. Kluge A, Muller C, Hansel J, Gerriets T, Bachmann G. Real-time MR with TrueFISP for the detection of acute pulmonary embolism: initial clinical experience. Eur Radiol. 2004. 14:709–718.18. Goyen M, Laub G, Ladd ME, Debatin JF, Barkhausen J, Truemmler KH, et al. Dynamic 3D MR angiography of the pulmonary arteries in under four seconds. J Magn Reson Imaging. 2001. 13:372–377.19. Dirksen MS, Lamb HJ, Kunz P, Robert P, Corot C, de Roos A. Improved MR coronary angiography with use of a new rapid clearance blood pool contrast agent in pigs. Radiology. 2003. 227:802–808.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dynamic Contrast-Enhanced MRI Using a Macromolecular MR Contrast Agent (P792): Evaluation of Antivascular Drug Effect in a Rabbit VX2 Liver Tumor Model
- Contrast-enhanced Magnetic Resonance Imaging of Brain Metastases at 7.0T versus 1.5T: A Preliminary Result
- Strong Contrast Stagnation of Unilateral Vertebral Artery on Three-Dimensional Black Blood-Enhanced MRI Predicts Acute Medulla Infarction
- 3D Whole-Heart Coronary MR Angiography at 1.5T in Healthy Volunteers: Comparison between Unenhanced SSFP and Gd-Enhanced FLASH Sequences
- Comparison of Gadomer-17 and Gd-DTPA in image quality of contrast-enhanced MR angiographies using flow phantom model